Abstract
Introduction Aberrant facial nerve regeneration (AFR) following facial nerve palsy may give rise to ptosis because of increased orbicularis tone. We describe a series of patients presenting with ptosis where the underlying aetiology of AFR was often not recognized by the referring clinicians.
Methods Retrospective case review.
Results A total of 15 cases with ptosis, secondary to AFR, were seen at the Royal Adelaide Hospital Oculoplastic Clinic between 2000 and 2002. Of these, 10 (67%) were referred by general ophthalmologists. Ptosis was the only reason for referral in 11 patients (73%) and features of AFR or a past history of facial nerve palsy were not mentioned in seven referrals (overall 46%). All patients reported a previous facial palsy. The palpebral aperture was reduced on the affected side with reduction in both upper and lower margin reflex distance (MRD) by a mean of 1.5±0.7 mm (P <0.001) and 1.0±0.3 mm (P <0.001), respectively. The orbicularis tone was increased and strength reduced on the affected side in all patients. However, none had lagophthalmos. Signs of AFR were demonstrated in all patients with either an increase in ptosis or eyelid closure on the affected side during cheek puffing.
Conclusion Patients with AFR following facial nerve palsy may present with ptosis without recognition of the underlying aetiology. Signs of AFR ptosis include a decreased palpebral aperture with a reduced upper and lower MRD. The diagnosis can be established with demonstration of an increase in ptosis during cheek puffing. Recognition of AFR is important in these cases owing to the implications for management and post-operative patient satisfaction.
Similar content being viewed by others
Introduction
Aberrant facial nerve regeneration (AFR) following facial nerve palsy may cause facial nerve synkinesis and ptosis.1 The latter is usually because of increased orbicularis tone and increases with synkinetic orofacial muscle contraction.2 These patients may be referred for ptosis surgery without recognition of the causal AFR or even a past history of facial nerve palsy.
Methods
A retrospective review of the clinic notes in the Oculoplastic Clinic, Royal Adelaide Hospital was carried out. All patients with acquired ptosis and an underlying diagnosis of AFR after facial nerve palsy, seen between August 2000 and 2002, were identified.
The case notes were reviewed and patients' demographics recorded. The referral details, time of onset of facial palsy, and patients' presenting complaints were noted.
Patients were examined by an Oculoplastic surgeon. Ophthalmic examination details and measurements were recorded and clinical photographs taken. Outcome measures included marginal reflex distance (MRD), levator function (LF), superior skin crease (SC), orbicularis tone, strength, presence of lagophthalmos, and presence of AFR. The upper and lower MRD are defined as the distance between the upper and lower eyelid margin and the light reflex in the pupil, respectively, with the eyes in the primary position and the patient looking directly at a pen torch held by the examiner. Features of AFR were defined as movement of the upper eyelid with cheek puffing or jaw movement. Crocodile tears were defined as epiphora with repeated cheek puffing or jaw movement. Electromyography (EMG) was performed in one case. Surgical and non-surgical treatments as well as outcomes were recorded.
Statistical analysis
Continuous data were analysed using a paired, two-tailed t-test and described as mean and standard deviation (mean±SD) and a probability of less than 0.05 was considered to be statistically significant.
Results
A total of 15 patients (11 women and four men, mean age 57±15 years, range 42–79 years) were identified. Nine out of 15 patients (60%) were referred by general ophthalmologists for further surgical management of ptosis, four were referred by general practitioners, and one patient was referred by a neurologist. In 11 of 15 patients (73%), ptosis was the only reason for referral. Ptosis and epiphora were the reasons for referral in the remaining four cases (Table 1). Nine patients (60%) complained of features of AFR (synkinetic facial movements or crocodile tears) and four of these were not recognized in the referral letter (patients 5, 11, 14, and 15).
All 15 patients reported a previous facial palsy. The median duration from facial nerve palsy to presentation was 3.0 years, range 1 and 40 years. The main cause of facial palsy was Bell's palsy (13/15 patients, 87%), and temporal bone fracture following closed head injury was the cause in the remaining two cases.
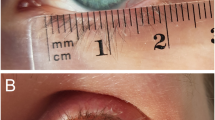
All patients with unilateral ptosis had a reduced upper MRD in comparison to the normal side (1.5±0.7 mm, P<0.001). The lower eyelid was also raised on the affected side with a reduced lower MRD in comparison to the normal side (mean 1.0±0.3 mm, P<0.001) (Figure 1). There was no significant difference in the LF and SC between the affected and unaffected side. The orbicularis tone was increased and strength decreased on the affected side in all cases; however, no patient had lagophthalmos.
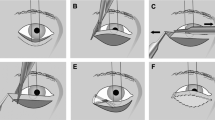
Signs of AFR were present in all patients. All patients demonstrated an increase in ptosis and narrowing of the palpebral aperture on the affected side during cheek puffing (Figure 2). Six patients (43%) demonstrated this on jaw movements to the contralateral side (Marin–Amat syndrome) and seven patients had crocodile tears (Table 1).
EMG was performed in one patient to confirm the diagnosis and showed synkinesis of the orbicularis oculi and oris muscles on the affected side. Only one patient had significant brow ptosis. Frontalis overaction was seen in another. Two patients had significant dermatochalasis.
Surgical procedures were performed in seven patients with good outcome (Table 1). Patients who underwent anterior levator resection did not develop lagophthalmos or exposure symptoms. Botulinum toxin was administered to the eyelid and lacrimal gland in one patient; symptoms of both eyelid closure and crocodile tears were improved at 3 months follow-up.
Discussion
AFR is a documented complication after peripheral facial nerve palsy and may give rise to ptosis. The variable ptosis is because of increased muscle tone in the orbicularis oculi on the affected side, exacerbated by synkinesis.1,2 Our series demonstrated the fact that AFR may be under-recognized as a cause of ptosis by both general practitioners and ophthalmologists. Signs of AFR may be subtle and include a reduced palpebral aperture owing to increased orbicularis oculi muscle tone. The upper and lower MRD are both significantly reduced on the affected side. In all patients, the diagnosis of ptosis owing to AFR was confirmed by instructing the patients to puff their cheeks resulting in increased ptosis, or even eyelid closure.
Marin–Amat syndrome describes synkinesis of orbicularis oculi and jaw movements. Wartenberg3 suggests that the automatic closure of one eye on opening of the mouth is contingent on movement of the lower facial muscles and not of the mandible. The pathogenesis of the abnormal facial synkinesis is unknown but thought to be because of a ‘misdirection’ of regenerating nerve fibres, originally supplying orbicularis oculi, to other facial muscles.1 Two additional mechanisms, a peripheral ephaptic transmission of impulses between axons or synaptic reorganization within the facial nerve nucleus, are also postulated.4 EMG testing helps confirm the clinical diagnosis of AFR, demonstrating a ‘synkinetic spread’.5 This was performed in one case in our series and also demonstrated synkinesis of the orbicularis oculi and oris, whereby, attempted eyelid closure resulted in twitching of the orbicularis oris.
The reported incidence of synkinesis in facial nerve palsy varies greatly ranging from 9 to 55%.1 Yamamoto et al6 found that synkinesis occurs most frequently in the 24–39th weeks of facial palsy. Celik et al2 noted that synkinesis develops at least 4 months after the onset of facial palsy. In our study, patients with ptosis secondary to AFR presented between 1 and 40 years after facial palsy. The onset of AFR was unclear in most of the patients in our series. AFR has also been reported in patients with hemifacial spasm.3 However, none of the patients in our series reported or demonstrated features of hemifacial spasm and all had suffered facial palsy in the past.
The diagnosis of AFR is important, as the treatment for these patients differs from other forms of ptosis. Preoperative evaluation is essential in order to identify the patient's actual symptoms: ptosis or synkinesis. Preoperative counselling, in order to avoid patient dissatisfaction, is also required (Figure 3a). The patient must be aware that despite symmetry of height and contour of the upper eyelids following the operation, the raised lower eyelid on the affected side may still give rise to a reduced and possibly variable palpebral aperture, depending on the degree of synkinesis (Figure 3b). Ptosis surgery should be approached cautiously, as the underlying increased orbicularis tone may give rise to unpredictability of the postoperative upper eyelid height. Furthermore, orbicularis weakness may compromise eyelid closure postoperatively. In our series, all patients treated surgically were successful with anterior levator resection, browpexy, or blepharoplasty.
Botulinum toxin type A (BTXA) has chemodenervative effects and is a useful treatment option for patients with motor and autonomic effects of AFR.7,8 The effect of botulinum toxin can last 3–4 months.7 Although Boroojerdi et al 8 reported only focal side effects of temporary orbicularis oculi muscle weakness, BXTA may also cause local side effects of ptosis, diplopia, dry eyes, malposition of the lower eyelid, pain, and local bruising.9
In conclusion, AFR as a cause of ptosis is often under-recognized. The ptosis is variable with reduction in both upper and lower MRD on the affected side. The diagnosis can be established by the presence of increased orbicularis tone on the affected side and an increase in ptosis with cheek puffing. Recognition of the underlying pathology is important in these cases owing to the implications for management and postoperative patient satisfaction.
References
Monteserra L, Benito M . Facial synkinesis and aberrant regeneration of facial nerve. In: Jankovic J and Tolosa E (eds). Advances in Neurology. Raven Press: New York, 1998 pp 211–224.
Celik M, Forta H, Vural C . The development of synkinesis after facial nerve paralysis. Eur Neurol 2000; 43: 147–151.
Wartenberg R . Inverted Marcus Gunn Phenomenon (so called Marin Amat Syndrome). Arch Neurol Psychiatr 1948; 60: 584–596.
Moran CJ, Neely JG . Patterns of facial nerve synkinesis. Laryngoscope 1996; 106: 1491–1495.
Kimura J, Rodnitzky RL, Okawara SH . Electrophysiologic analysis of aberrant regeneration after facial nerve paralysis. Neurology 1975; 25: 989–993.
Yamamoto E, Nishimura H, Hirono Y . Occurrence of sequelae in Bell's palsy. Acta Otolaryngol 1998; 446: 93–96.
Keegan DJ, Geerling G, Lee JP, Blake G, Collin JR, Plant GT . Botulinum toxin treatment for hyperlacrimation secondary to aberrant regenerated seventh nerve palsy or salivary gland transplantation. Br J Ophthalmol 2002; 86: 43–46.
Boroojerdi B, Ferbert A, Schwarz M, Herath H, Noth J . Botulinum toxin treatment of synkinesia and hyperlacrimation after facial palsy. J Neurol Neurosurg Psychiatry 1998; 65: 111–4.
Dutton JJ . Botulinum-A toxin in the treatment of craniocervical muscle spasms: short- and long-term, local and systemic effects. Surv Ophthalmol 1996; 41: 51–65.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chen, C., Malhotra, R., Muecke, J. et al. Aberrant facial nerve regeneration (AFR): an under-recognized cause of ptosis. Eye 18, 159–162 (2004). https://doi.org/10.1038/sj.eye.6700599
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6700599
Keywords
This article is cited by
-
Botulinumtoxin bei okulären Folgen nach Fazialisparese
Der Ophthalmologe (2012)