Abstract
Purpose To evaluate the results of conventional extracapsular cataract extraction and phacoemulsification cataract surgery, in renal transplant patients.
Methods A total of 11 eyes of eight renal transplant recipients who underwent cataract surgery in Ankara between 1995 and January 2001 were evaluated. Each individual underwent routine ophthalmologic examination including visual acuity with Snellen chart testing, slit-lamp examination, intraocular pressure measurement, and fundus examination. Of these, seven patients had posterior subcapsular cataracts and four had nuclear cataracts. Conventional extracapsular cataract extraction (cECCE) was performed in four eyes with single-piece all-polymethylmethacrylate posterior chamber intraocular lens implantation. The other seven eyes were treated with small-incision phacoemulsification and implantation of a foldable hydrophilic acrylic lens.
Results We observed intraoperative posterior capsule rupture and vitreous loss in one patient, postoperative intraocular tension elevation in one patient, and sterile suture infiltration in one patient in our series. Average of the visual acuities 6 months after the operation was 20/30 (range, 20/60–20/20).
Conclusions In this, the first published report to describe outcomes of cataract surgery in renal transplant patients, most complications were associated with high of steroids use and immunosuppressives, and were independent of the type of cataract surgery used, either ECCE or phacoemulsification surgery. The study suggests the need for additional care before, during, and after operation.
Similar content being viewed by others
Introduction
Renal transplantation significantly improves the prognosis for individuals with chronic renal failure (CRF) and, as kidney function is almost completely restored, problems associated with uraemia are eliminated.1 However CRF patients often exhibit coagulation defects, malnutrition, altered immune response, and wound healing defects.2 The eye in CRF patients is affected in many ways because of haematological and metabolic alterations that occur during the course of the disease.3
The ocular complications that arise after renal transplantation have been well documented and include opportunistic infections, steroid-induced posterior subcapsular cataracts, and elevated intraocular pressure (IOP). Cytomegalovirus (CMV) retinitis and other opportunistic retinal and choroidal infections are additional complications. The majority of these problems develop because of immunosuppressive treatment and steroid therapy.
Visual outcomes and the complications of cataract operations in renal transplant patients are poorly documented in the medical literature. Our aim in this study was to investigate the results of cataract surgery in a group of kidney recipients who were on long-term immunosuppressive therapy that included steroids. To our knowledge, this is the first report to discuss the outcomes of cataract surgery in this patient group.
Materials and methods
A total of 11 eyes of eight renal transplant recipients who underwent cataract surgery between December 1995 and January 2001 at Başkent University Hospital in Ankara were retrospectively evaluated. In all, six patients were males, two were females, with a mean patient age of 46 years (range, 23–61 years). The mean follow-up period (1–4.5 years) after renal transplantation was 2.3 years. Each individual underwent routine ophthalmologic examination with Snellen visual acuity testing, slit-lamp examination, IOP measurement, and fundus examination. Of these, seven patients had posterior subcapsular steroid cataracts and four had nuclear cataracts. The preoperative ocular findings included inactive CMV retinitis in one patient who had been treated with intravitreal and intravenous gancyclovir and choroidal granuloma and perivasculitis caused by miliary tuberculosis in a second patient and who had been treated with a 12-month course of medical therapy.
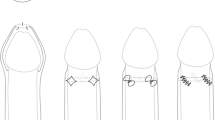
In four eyes, conventional extracapsular cataract extraction (cECCE) was performed with single-piece all-polymethylmethacrylate (PMMA lens; Biotech, France) posterior chamber intraocular lens implantation. The other seven eyes were treated with small-incision phacoemulsification and implantation of a foldable hydrophilic acrylic lens (Acrysoft, Alcon, USA). Cohesive type (Biolon, Chauvin, France) of viscoelastic material was used in ECCE and Disperse Type (Viscoat, Alcon, Belgium) of viscoelastic material was used during phacoemulsification operations. All patients received subconjunctival injections of antibiotics and steroids postoperatively and were also prescribed a 4-week course of topical dexamethasone phosphate (at 3-h intervals initially) and topical tobramycin sulphate (at 4-h intervals initially), with doses and dosing schedules tapered in accordance with routine clinical postoperative response.
On admission and at each follow-up visit, a routine ophthalmological examination was repeated.
Results
The mean preoperative best corrected visual acuity (BCVA) in the 11 eyes was 20/100 (range, 20/200–20/60). At 6 months postsurgery, the mean BCVA was 20/30 (range, 20/60–20/20). The pre- and postoperative visual acuity for each eye are shown in Figure 1. Intraoperative posterior capsule rupture and vitreous loss occurred in one patient during phacoemulsification surgery. As a result, anterior vitrectomy with lens implantation into the sulcus was performed. There were no intraoperative complications in any of the other seven patients.
Postoperatively, three of the 11 eyes (seven of them had preoperative steroid-type cataract) developed visually significant posterior capsular opacification within 6 months and were treated with yttrium–aluminium–garnet laser (YAG) capsulotomy. One of the 11 eyes that had undergone phacoemulsification showed IOP elevation on the first day after surgery, which may have been because of retained Disperse Type viscoelastic material. In this case, the IOP was successfully controlled with topical antiglaucoma therapy. A further eye developed suture infiltrates (Figure 2). Cultures of the conjunctiva, and cultures and smears from corneal scrapings, showed no microbial growth, and healing occurred after 2 weeks of topical steroid treatment. The two eyes that had had previous retinal (CMV) and choroidal (tuberculosis) infections, respectively, showed no recurrence of these problems. One of the eight eyes was diagnosed with hypertensive retinopathy before the operation, and this condition remained after the cataract surgery (Figure 3).
Discussion
Changes in ocular osmolarity and related lens opacity have been reported in patients with CRF. Berlyne et al4 described 50% punctate cataract development in clear lenses in CRF patients, noting that these resembled lesions in patients with other hypocalcaemic conditions. It is suspected that the factors that predispose patients to cataract development in CRF are related to changes in calcium metabolism, such as hypocalcaemia, hyperparathyroidism, and sudden metabolic and osmotic changes during haemodialysis.5 Ocular complications in renal transplant patients are reportedly associated with significant morbidity. Lens opacity is the most common of these problems.
Corticosteroids used for immunosuppression in kidney transplant recipients can either accelerate or increase cataract formation. Steroid use is the most frequent cause of cataract development, and the likelihood of such problems depends on the dosage and dosing interval used. In addition to cataract formation, steroid use in kidney recipients may also lead to IOP elevation, opportunistic infection, retinal vascular occlusion, and increased incidence of hypertensive and diabetic retinopathy.6
In the current study, 11 eyes of eight patients were treated with cataract extraction and lens implantation. Phacoemulsification was performed in seven eyes and cECCE in four eyes. Visually significant posterior capsular opacification occurred in 36% of the treated eyes (one phacoemulsification case and two cECCE cases). This high incidence of posterior capsular opacification requiring YAG capsulotomy might be related to the distribution of cataract types in our series, since the majority (seven of 11) of the eyes we studied had steroid-induced-type posterior subcapsular cataracts.7
Development of opportunistic CMV, herpes simplex, herpes zoster, cryptococcosis, candidiasis, or toxoplasmosis infections secondary to immuno-suppression is of great concern to both clinicians and patients, because the end result is often irreversible visual damage. Prior to surgery, one of our patients had had CMV retinitis and one had had choroidal granuloma and perivasculitis related to miliary tuberculosis. Neither of these individuals developed reactivation of the infections postoperatively.
CRF patients on haemodialysis typically exhibit reduced ocular immunoglobulin and lysozyme levels in the anterior segment as a result of lower ocular tear levels. This compromise of defense mechanisms predisposes the patient to inflammation at the ocular surface. Consequently, there is a high frequency of suture infiltration, as reported by Dursun et al8 where 10 out of the 14 eyes in CRF patients developed suture infiltration after cataract surgery. There are fewer of these complications after renal transplantation because ocular tear levels and tear function usually return to normal. Only one of the 11 eyes in the kidney recipients we studied developed suture infiltration after cataract surgery.
In addition to elevated blood pressure, other factors in the aetiology of retinopathy in advanced renal disease are (i) diffuse metabolic imbalances caused by nitrogen retention, (ii) excess renin formation, and (iii) hypervolaemia because of water and sodium retention.9,10,11 Steroid use in renal transplant patients may increase the risk of hypertensive retinopathy through sodium and water retention. In one of our eight patients, the signs of hypertensive retinopathy were aggravated by cataract surgery.
In this, the first published report to describe outcomes of cataract surgery in renal transplant patients, we feel it important to underline the importance of extra preoperative care to CRF patients; systemic problems such as control of hypertension, tendency for haemorrhage, and diabetes, can always alter the results of cataract surgery. In addition, during surgery special precautions should be taken to minimise trauma, and dispersive viscoelastic material should be used to decrease the risk of haemorrhage. Finally, postoperatively, it is advisable to follow up patients more frequently as they might have wider range of complications than is usual.
The limitation of this study resides in its noncontrolled design. Owing to the small sample studied we were unable to carry out a statistical analysis. It would be of interest in future studies to analyse prospectively cataract operation complications and outcomes in patients with CRF and compare these to patients with renal transplantation, and with patients with no pre-existing disease.
References
Andreoli E, Evanoff V, Ketch L . Chronic renal failure. In: Andreoli E, Bennet J, Carpenter J, Plum F, Smith H (ed). Cecil's Essentials of Medicine. WB Saunders Co.: Philadelphia, 1993: pp 244–254.
Burke JF, Francos GC . Surgery in the patient with acute or chronic renal failure. Med Clin North Am 1987; 71: 489–497.
Aydin P, Oto S, Kadayifçilar S, Dursun D . Ophthalmological problems in renal transplant patients. Transplant Proc 1996; 28: 2312–2313.
Berlyne GM, Ari JB, Danovitch GM, Blumental M . Cataracts of chronic renal failure. Lancet 1972; I: 509–511.
Osman EM, Abboud OI, Musa AR, Mohammed KE . Cataract in chronic renal failure. Nephrol Dial Transplant 1992; 7: 1162.
Laiba H, Oliver M, Shimshoni M . Intraocular pressure fluctuations during regular hemodialysis and ultrafiltration. Acta Ophthalmol (Copenh) 1990; 68: 320–322.
Argento C, Nunez E, Wainsztein R . Incidence of postoperative posterior capsular opacification with types of senile cataracts. J Cataract Refract Surg 1992; 18: 585–588.
Dursun D, Akova Y, Akman A, Oto S, Aydın P . Complications of extracapsular cataract surgery in chronic renal failure patients. Eye 2000; 14: 176–179.
La Piana FG . Renal diseases. In: Duane TP, Jaeger EA (eds). Clinical Ophthalmology, Vol 5, chapter 37, Harper & Row: Philadelphia, 1978, pp 1–6.
Murphy RP, Chew EY . Hypertension. In: Ryan SJ, Schachat AP, Murphy RB, Patz A (eds). Retina, Vol 2, Chapter 78. CV Mosby: St Louis, 1989, pp 449–455.
Alm A, Bill A . Ocular circulation. Clinical application. In: Moses RA, Hart WM (eds). Adler's Physiology of the Eye. CV Mosby: Missouri, 1987, pp 183–203.
Author information
Authors and Affiliations
Corresponding author
Additional information
Presented partly at ‘25 years in Renal Transplantation’ Conference, November 2001, Ankara, Turkey
The authors have no proprietary interest
Rights and permissions
About this article
Cite this article
Akbulut, A., Tayanç, E., Çetinkaya, A. et al. Results of cataract surgery in renal transplantation patients. Eye 17, 346–349 (2003). https://doi.org/10.1038/sj.eye.6700365
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6700365