Abstract
Background Age-related maculopathy (ARM) or degeneration (ARMD) is the leading cause of irreversible blindness in developed countries. Despite several studies on the morphology of ARMD, the aetiology is unknown and factor(s) contributing to the pathogenesis remain to be characterised. More recent studies have demonstrated that cholesterol esters and lipids are present within Bruch's membrane deposits and drusen, and dietary fat intake is associated with ARMD. The product of Obgene, leptin, is a recently discovered peptide participating in human metabolism. There is a direct relationship between serum leptin and diet, and lipoprotein metabolism, but the role of leptin in the course of ARMD has not previously been investigated.
Purpose This cross-sectional case–control study investigated whether serum leptin level was associated with ARMD as a new possible risk factor and to assess its relationship with disease severity.
Methods A total of 32 patients with ARM or ARMD (17 men, 15 women) and 20 age- and sex-matched healthy control subjects without ARMD (11 men, nine women) from a similar ethnic background were enrolled in this multicentre study. Body mass index (BMI) (weight (kg)/height (m2)) was calculated for each group. The presence of maculopathy was assessed on the basis of colour fundus photographs using an international classification system. Patients were classified as early-ARM (n=16) or late-ARMD (n=16) using clinical examination and grading of photographs. Serum leptin levels were measured by an enzyme-linked immunosorbent assay kit. The Mann–Whitney U test or χ2 test was used for statistics as indicated, and P<0.05 was considered to be significant.
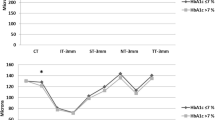
Results The age, sex ratio, and BMI between groups were comparable. Patients with maculopathy had significantly (P<0.001) lower leptin levels (mean±SD, 6.01±2.55 ng/ml) than control subjects (13.21±2.27 ng/ml). In addition, late-ARMD patients had significantly lower leptin levels (3.81±0.58 ng/ml) than early-ARM patients (8.21±1.68 ng/ml, P<0.001) or control subjects (P<0.001).
Conclusion Leptin seems to be a possible newly associated factor in the course of ARM and may be involved in the lipid composition of the macular lesions, especially in late-ARMD.
Similar content being viewed by others
Introduction
Age-related macular degeneration (ARMD) is the foremost cause of blindness among the elderly population in industrialised countries, and the early stages of the disease are called age-related maculopathy (ARM).1,2 The cause of the disease remains obscure; however, but genetic factors,3 atherosclerosis,4 oxidative stress,5 decreased antioxidants,6 and higher cholesterol and plasminogen levels7,8,9 have all been implicated in the pathogenesis, although data are still scarce and inconsistent. It is, therefore, urgent to determine the factor(s) that may lead to this disease.
Leptin, a newly discovered adipose-derived 16-kDa peptide (which communicates the status of peripheral fat cells and lipids to the brain), continues to attract considerable interest.10 It appears to act as a hormonal signal between peripheral adipose tissue and lipids and the feeding centres in the hypothalamus, and reduces adipocyte mass. It can induce haemopoietic cell activation and can enhance the production of macrophages, suggesting a role in the host defence.11 Serum leptin concentration closely reflects the total lipid amount of the body and directly inhibits intracellular lipid concentrations by reducing fatty acid and triglyceride synthesis.12 It has also been proposed that leptin has a direct metabolic effect on lipoprotein metabolism or lipase activities. If the serum leptin level is deficient, fatty acid synthesis would increase by the inhibition of mitochondrial fatty acid uptake and oxidation, resulting in higher intracellular fatty acid and triglyceride levels.13
Photoreceptor-retinal pigment epithelium (RPE) complex contains high levels of polyunsaturated fatty acids. Therefore, the macular area is highly susceptible to oxidative damage and lipid peroxidation with its near-arterial oxygen level.14 Lipofuscin phototoxicity (lipid/protein aggregates) was described and suggested to be toxic to RPE cells, thus supporting a role for lipofuscin in ageing and ARMD.15 RPE regulates the lipid metabolism of the photoreceptors by catalysis of membrane outer segments. Blood lipid uptake is mediated by specific LDL receptors and this affects the lipid metabolism of the photoreceptor-RPE complex.16 As a result, deficiency in LDL receptor regulation might lead to intracellular accumulation of lipids, which might play a role in the pathogenesis of ARMD. In addition, the total fat intake is positively associated with risk of ARMD, which may be due to individual fatty acid intake like linolenic acid.17 Furthermore, cholesterol esters and lipids accumulate within Bruch's membrane deposits and drusen, and cause an increase in the amount of peroxidised lipids with age, suggesting a role for lipids in the aetiology of ARMD.18,19 Therefore, it is plausible that leptin may participate in the pathophysiology of ARMD, and we expect a decreased serum leptin concentration in ARMD patients. This multicentre study aimed for the first time to assess whether serum leptin level was associated with ARMD as a new possible risk factor and, if so, whether it was correlated with disease severity.
Research design and methods
Study population
Consecutive ARMD patients were selected from the outpatient clinic at the research hospital. These patients were asked whether they were willing to participate in the study. Healthy subjects without ARMD from a similar ethnic background were enrolled as controls. Smoking status, detailed family history of ARMD, medical and ocular history, and dietary intake were elicited by a questionnaire in both groups. The patients and controls had to fulfil the following criteria: age over 60 years, stable weight, body mass index (BMI) within normal range (20–25), sedentary lifestyle, and normal caloric intake. Exclusion criteria were smokers, eating disorders, medication with lipid-lowering drugs or agents affecting metabolism, antioxidant drugs, diabetes, cardiovascular disease, and acute or chronic neurological disorder.20,21,22 Blood screening parameters (white and red blood cell count, platelet count, sodium, potassium, creatinine, aspartate, and alanine aminotransferase) and urine analyses had to be within normal limits. None had malignant or chronic inflammatory diseases. In addition, a thorough physical examination was performed and groups were carefully matched for age, sex, and BMI. All subjects in both groups gave informed consent before participating in the study. Height was recorded to the nearest 0.5 cm and weight to the nearest 0.1 kg for BMI calculation at study enrolment. Although some studies showed no relationship between age and leptin concentration,23 we still matched the patients with maculopathy and controls for age.
Definitions and grading of ARMD
All patients had fundus photography and fluorescein angiography. The Wisconsin Age-Related Maculopathy Grading System, developed by Klein et al24 and incorporated in an international classification system,2 was used to grade individual ARM lesions. A grid with a radius of 3000 μm, centred on the fovea of stereo-colour fundus photographs, was used. Two experienced graders graded all photographs and the group of the patient was determined in a masked manner. Early-ARM was defined as the presence of either soft indistinct or regular drusen within the area of the macula covered by the grid, or the presence of both distinct, soft drusen within the grid and RPE abnormalities in the absence of late-ARMD in either eye. Advanced (late)-ARMD included the presence of subretinal fibrous scar, signs of choroidal neovascularisation ‘wet-ARMD’ (serous detachment of the neuroepithelium, subretinal haemorrhages, and/or exudates), RPE detachment, or confluent patches of RPE atrophy ‘dry-ARMD/geographic atrophy’ in at least one eye. If both eyes were graded, participants were categorised according to the findings in the field of the worse eye. Finally, 16 patients were classified as having early-ARM and the remaining 16 as late-ARMD.
Blood samples
This double-blind study both masked the physician taking the blood and the analyser to the group of the subject. Whole blood samples (total 5 ml) were drawn using a 25-gauge needle from an antecubital vein, avoiding haemolysis, into plain tubes in the morning hours (08.30–10.30) after an overnight fast and 30 min of supine rest. Following centrifugation of half of the blood samples at 800g for 10 min at 4°C, serum was collected and kept at −70°C until the time of analysis.
Serum leptin analysis
Duplicate serum samples from each subject were assayed for leptin by a commercially available enzyme-linked immunosorbent assay (Leptin Enzyme Immunoassay Kit, Cayman Chem., Ann Arbor, MI, USA). It is an immunometric sandwich enzyme immunoassay that permits leptin measurements within a range of 1–50 ng/ml with a detection limit of 1 ng/ml. Inter- and intra-assay coefficients of variances were both less than 9%. The assay allows sensitive and specific analysis of leptin in serum.
Calculations and statistics
BMI was calculated in both groups as weight (kg) divided by height (m2).25 The Mann–Whitney U test or χ2 was used for the statistics as indicated, test and results were expressed as mean±SD. P values below 0.05 were considered to indicate statistical significance. Statistical analysis was performed with the Statistical Package for the Social Sciences for Windows (version 8.0, SPSS Inc., Chicago, IL, USA).
Results
A total of 46 patients gave their consent, but nine had exclusion criteria that are mentioned in the text. In addition, two patients with poor dilation, one patient with corneal opacity, and two patients with cataract were not included in the present study for clinical ungradeability. Therefore, 32 patients with maculopathy (17 men, 15 women) were included in the present study, in which clinical and photographic grading were available in all subjects. Altogether, 20 age- and sex-matched hospital-based healthy control subjects without maculopathy (11 men, nine women) from a similar ethnic background served as control. The mean BMI was similar (P>0.05) between patients with maculopathy (22.35±0.66) and control subjects (22.61±0.77). The age and sex ratios were not substantially different (for each, P>0.05) among patients (68.18±4.33 years) and control subjects (67.60±3.92 years). Across all patients with maculopathy, serum leptin concentrations were significantly (P<0.001) lower (6.01±2.55 ng/ml) when compared with those in control subjects (13.21±2.27 ng/ml). In addition, patients with late-ARMD (n=16; BMI: 22.44±0.67) had significantly (P<0.001) lower leptin levels (3.81±0.58 ng/ml) than early-ARM patients (n=16; BMI: 22.26±0.65; 8.21±1.68 ng/ml) and control subjects (P<0.001) (Figure 1).
Discussion
The causes of ARMD are not known, but there are many hypothesised risk factors including smoking, systemic hypertension, past diagnosis of vascular disease, high cholesterol and fibrinogen levels, and higher or lower BMI.4,7,8,9,26 Although ARMD is the leading cause of irreversible blindness in the elderly population, some interventions have proven effective in prevention of the disease. Observational and experimental data suggest that antioxidant and zinc supplements may delay progression of ARMD and vision loss.27 Indeed, in the ARMD trial studies, those at high risk of developing advanced ARMD have lowered their risk by about 25% when treated with mega dosages of the combination of antioxidants and minerals.28 The micronutrients studied were the antioxidants, vitamins E, C, beta-carotene and zinc with copper. In addition, laser photocoagulation has been known to be an effective treatment, but its benefits are limited. On the other hand, despite several studies on the morphology of the disease, the mechanism contributing to the pathogenesis of ARMD remains unclear. Therefore, identifying the risk factor(s) associated with ARMD are of great interest.
Our recent study clearly demonstrated that nitric oxide, the most abundant free radical in the body, might be implicated in the pathophysiology of ARMD in association with decreased superoxide dismutase and glutathione peroxidase enzyme activities both in plasma and erythrocytes, stimulating lipid peroxidation.29 The results of this preliminary study clearly demonstrated that serum leptin levels were lower in patients with maculopathy than age-, sex-, and BMI-matched control subjects, and the difference was significant. Furthermore, decreased leptin levels were negatively correlated with disease severity, which was lower in late-ARMD patients than in early-ARM subjects. Therefore, from the evidence stated above, decreased leptin levels might result in the loss of its lipidostatic function in cellular level and could cause an increased intracellular fatty acid accumulation within the lesions found in ARM or ARMD patients.
It has been reported that BMI is significantly associated with ARM, with both underweight and overweight subjects having a significantly increased risk of maculopathy. Hirvela et al30 found a higher risk of ARM with the increase in BMI, whereas Klein et al1 demonstrated no associations between BMI and ARMD. Therefore, having a BMI either lower or higher than the accepted normal range (20–25) was associated with a significantly increased risk of maculopathy. In addition, comparable increases in risk were apparent for late-ARMD.1,30 These reported opposite associations are difficult to explain, as a low BMI conferred an increased risk for maculopathy almost equal to that of obesity. Interesting in this respect is the protective association between ARM and the frequency of fish consumption and the higher polyunsaturated fat intake,9 although the Beaver Dam Eye Study has reported no associations between ARM and seafood consumption.31 These results are also confusing and the exact mechanisms or factors remain to be characterised. None of these studies and other previous reports have investigated serum leptin concentrations in their ARM subjects, which is the major determinant of lipid compositions. Our subjects with or without maculopathy were comparable for BMI. Therefore, it is highly plausible that leptin may be an additional contributing or associating factor during the course of ARMD. The exact mechanism by which leptin may mediate or modulate the formation of ARMD lesions is intriguing. Leptin may act directly, indirectly or in conjunction with the possible other metabolic signals for lipid transportation into the lesions.
When discussing our findings, some limitations concerning the methodology of the present study should be mentioned. On the one hand, we did not measure vitreal leptin concentrations to assess whether it was correlated with serum levels, which awaits further investigation. On the other hand, because both high and low BMI have been found to be associated with maculopathy, one should therefore consider that this study include such patients for the comparison of the measured levels. However, ARMD obviously occurs in subjects with normal BMI as well. In other words, BMI is one of the many accused factors in the aetiopathogenesis of ARMD. Therefore, we have chosen normal BMI patients so that the study groups would methodologically be similar for the comparison of the leptin levels. Of course, the study can be performed in ARMD patients in a broader spectrum with high or low BMI, which is also open to further studies with possible correlation analysis. Finally, we did not measure serum VLDL and cholesterol levels to assess whether there was a correlation between the measured parameters and the severity of the disease. Although changes of leptin may be related to changes in total cholesterol, serum triglycerides, and VLDL, it has been demonstrated that leptin is associated with many other systemic diseases such as acute phase response, endotoxemia, sepsis and septic shock32,33 with no connection to the plasma VLDL and cholesterol status. Indeed, Thong et al21 studied plasma leptin levels in female athletes to relate it with body fat, nutritional, and endocrine factors, but did not measure plasma lipid status. Therefore, the present study is methodologically similar with the previous studies.
In conclusion, although this study showed no causal relationship between leptin levels and ARMD, it was correlative and there may be an association between leptin levels and the lipid composition of ARMD lesions. Because of its potential regulatory role in intracellular fatty acid and triglyceride levels, it is important to define the molecular mechanism underlying cell-tissue-specific gene expression in such patients with ARMD. In addition, we supposed that serum leptin might be related to the extent of disease state and, therefore, might serve as a marker of the severity and outcome of patients with ARMD. Evidences from other larger studies are required to confirm these findings. Identifying preventable risk factors as well as new treatment modalities for ARMD, now the most common cause of blindness in Western countries, by using leptin or leptinomimetic agents might be helpful in reducing the burden of this disease, as current treatments are not present. The observation of this preliminary study is new and certainly worthwhile to be examined by additional works in the future.
References
Klein R, Klein BE, Jensen SC, Meuer SM . The five-year incidence and progression of age-related maculopathy: the Beaver Dam Eye Study. Ophthalmology 1997; 104: 7–21.
Bird AC, Bressler NM, Bressler SB, Chisholm IH, Coscas G, Davis MD et al. An international classification and grading system for age-related maculopathy and age-related macular degeneration: the International ARM Epidemiological Study Group. Surv Ophthalmol 1995; 39: 367–374.
Allikmets R, Shroyer NF, Singh N, Seddon JM, Lewis RA, Bernstein PS et al. Mutation of the Stargardt disease gene (ABCR) in age-related macular degeneration. Science 1997; 277: 1805–1807.
Vingerling JR, Dielemans I, Bots ML, Hofman A, Grobbee DE, de Jong PT . Age-related macular degeneration is associated with atherosclerosis: the Rotterdam Study. Am J Epidemiol 1995; 142: 404–409.
Antioxidant status and neovascular age-related macular degeneration. Eye Disease Case–Control Study Group. Arch Ophthalmol 1993; 111: 104–109.
Christen WG, Glynn RJ, Hennekens CH . Antioxidants and age-related eye disease. Ann Epidemiol 1996; 6: 60–66.
Risk factors for neovascular age-related macular degeneration. The Eye Disease Case–Control Study Group. Arch Ophthalmol 1992; 110: 1701–1708.
Smith W, Mitchell P, Leeder SR, Wang JJ . Plasma fibrinogen levels, other cardiovascular risk factors, and age-related maculopathy: the Blue Mountains Eye Study. Arch Ophthalmol 1998; 116: 583–587.
Smith W, Mitchell P, Leeder SR . Dietary fat and fish intake and age-related maculopathy. Arch Ophthalmol 2000; 118: 401–404.
Zhang Y, Proenca R, Maffei M, Barone M, Leopold L, Friedman JM . Positional cloning of the mouse obese gene and its human homologue. Nature 1994; 372: 425–432.
Campfield LA, Smith FJ, Guisez Y, Devos R, Burn P . Recombinant mouse OB protein: evidence for a peripheral signal linking adiposity and central neural networks. Science 1995; 269: 546–549.
Shimabukuro M, Koyama K, Chen G, Wang MY, Trieu F, Lee Y et al. Direct antidiabetic effect of leptin through triglyceride depletion of tissues. Proc Natl Acad Sci USA 1997; 94: 4637–4641.
Auwerx I, Staels B . Leptin. Lancet 1998; 351: 737–742.
Gerster H . Review: antioxidant protection of the ageing macula. Age Ageing 1991; 20: 60–69.
Winkler BS, Boulton ME, Gottsch JD, Sternberg P . Oxidative damage and age-related macular degeneration. Mol Vis 1999; 5: 32.
Noske UM, Schmidt-Erfurth U, Meyer C, Diddens H . Lipid metabolism in retinal pigment epithelium. Possible significance of lipoprotein receptors. Ophthalmologe 1998; 95: 814–819.
Cho E, Hung S, Willett WC, Spiegelman D, Rimm EB, Seddon JM et al. Prospective study of dietary fat and the risk of age-related macular degeneration. Am J Clin Nutr 2001; 73: 209–218.
Spaide RF, Ho-Spaide WC, Browne RW, Armstrong D . Characterization of peroxidized lipids in Bruch's membrane. Retina 1999; 19: 141–147.
Haimovici R, Gantz DL, Rumelt S, Freddo TF, Small DM . The lipid composition of drusen, Bruch's membrane, and sclera by hot stage polarizing light microscopy. Invest Ophthalmol Vis Sci 2001; 42: 1592–1599.
Bornstein SR, Preas HL, Chrousos GP, Suffredini AF . Circulating leptin levels during acute experimental endotoxemia and antiinflammatory therapy in humans. J Infect Dis 1998; 178: 887–890.
Thong FS, McLean C, Graham TE . Plasma leptin in female athletes: relationship with body fat, reproductive, nutritional, and endocrine factors. J Appl Physiol 2000; 88: 2037–2044.
Segal KR, Landt M, Klein S . Relationship between insulin sensitivity and plasma leptin concentration in lean and obese men. Diabetes 1996; 45: 988–991.
Ostlund RE, Yang JW, Klein S, Gingerich R . Relation between plasma leptin concentration and body fat, gender, diet, age, and metabolic covariates. J Clin Endocrinol Metab 1996; 81: 3909–3913.
Klein R, Davis M, Magli YL, Segal P, Klein BE, Hubbard L . The Wisconsin age-related maculopathy grading system. Ophthalmology 1991; 98: 1128–1134.
Hannan WJ, Wrate RM, Cowen SJ, Freeman CP . Body mass index as an estimate of body fat. Int J Eat Disord 1995; 18: 91–97.
Goldberg J, Flowerdew G, Smith E, Brody J, Tso MO . Factors associated with age-related macular degeneration. An analysis of data from the first National Health and Nutrition Examination Survey. Am J Epidemiol 1988; 128: 700–710.
Age-Related Eye Disease Study Research Group. A randomized, placebo-controlled, clinical trial of high-dose supplementation with vitamins C and E, beta carotene, and zinc for age-related macular degeneration and vision loss. Arch Ophthalmol 2001; 119: 1417–1436.
Sackett CS, Schenning S . The age-related eye disease study: the results of the clinical trial. Insight 2002; 27: 5–7.
Evereklioglu C, Er H, Doganay S, Cekmen M, Turkoz Y, Otlu B et al. Nitric oxide and lipid peroxidation are increased and associated with decreased antioxidant enzyme activities in patients with age-related macular degeneration. Doc Ophthalmol 2002; in press.
Hirvela H, Luukinen H, Laara E, Sc L, Laatikainen L . Risk factors of age-related maculopathy in a population 70 years of age or older. Ophthalmology 1996; 103: 871–877.
Mares-Perlman JA, Brady WE, Klein R, VandenLangenberg GM, Klein BE, Palta M . Dietary fat and age-related maculopathy. Arch Ophthalmol 1995; 113: 743–748.
Landt M, Parvin CA, Wong M . Lepin in cerebrospinal fluid from children: correlation with plasma leptin, sexual dimorphism, and lack of protein binding. Clin Chem 2000; 46: 854–858.
Arnalich F, Lopez J, Codoceo R, Jim nez M, Madero R, Montiel C . Relationship of plasma leptin to plasma cytokines and human survival in sepsis and septic shock. J Infect Dis 1999; 180: 908–911.
Acknowledgements
The authors have no financial or proprietary interest in any instrument or products used in this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Evereklioglu, C., Doganay, S., Er, H. et al. Serum leptin concentrations are decreased and correlated with disease severity in age-related macular degeneration: a preliminary study. Eye 17, 350–355 (2003). https://doi.org/10.1038/sj.eye.6700345
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6700345