Abstract
Purpose To establish the efficacy and safety of botulinum toxin in the treatment of Crocodile Tear Syndrome and record any possible complications.
Methods Four patients with unilateral aberrant VII cranial nerve regeneration following an episode of facial paralysis consented to be included in this study after a comprehensive explanation of the procedure and possible complications was given. On average, an injection of 20 units of botulinum toxin type A (Dysport®) was given to the affected lacrimal gland. The effect was assessed with a Schirmer’s test during taste stimulation. Careful recording of the duration of the effect and the presence of any local or systemic complications was made.
Results All patients reported a partial or complete disappearance of the reflex hyperlacrimation following treatment. Schirmer’s tests during taste stimulation documented a significant decrease in tear secretion. The onset of effect of the botulinum toxin was typically 24–48 h after the initial injection and lasted 4–5 months. One patient had a mild increase in his preexisting upper lid ptosis, but no other local or systemic side effects were experienced.
Conclusions The injection of botulinum toxin type A into the affected lacrimal glands of patients with gusto-lacrimal reflex is a simple, effective and safe treatment.
Similar content being viewed by others
Introduction
Crocodile tear syndrome (CTS) or gusto-lacrimal reflex consists of unilateral lacrimation which occurs when a patient eats or drinks.1,2,3 It was first described in 1913 and since then many cases have been reported in the medical literature. This rare phenomenon usually follows a Bell’s palsy or a traumatic facial paralysis. It may occur congenitally with Duane’s retraction syndrome.4 The most commonly accepted mechanism for the pathogenesis of this abnormal reflex appears to be the misdirection of regenerating gustatory fibers from either the facial or glossopharyngeal nerves. After being injured the nerves may redirect themselves through the greater superficial petrosal nerve to reach the lacrimal gland, and cause ipsilateral tearing when the patient eats1,2,3 (Figure 1). An alternative hypothesis is that the nerve fibres do not actually regenerate, but rather form an artificial synapse at the site of the injury which allows the crossover of impulses from one fibre to another and interaction between afferent and efferent axons.5
Many attempts have been made to abolish the annoying manifestations of this reflex. These include intraorbital injection of alcohol or cocaine to destroy postganglionic fibers of the sphenopalatine ganglion, subtotal resection of the lacrimal gland, sectioning of the glossopharyngeal and facial nerves at different levels and the use of anticholinergic drugs.2,3 The results have been extremely variable. Some of these treatments have resulted in total ablation of lacrimal secretion and some of threatened sight. Recent reports6,7,8 suggest that injection of botulinum toxin type A (BTX-A) into the lacrimal gland of patients with CTS may effectively and safely abolish the reflex by chemodenervating the cholinergic neurons of the parasympathetic nervous system to the affected gland.
The purpose of this paper is to describe our initial experience with botulinum toxin to treat crocodile tear syndrome, to establish the efficacy and safety of the treatment and record possible complications.
Methods
Four patients with CTS were identified and included in the study after informed consent was obtained. Their ages ranged from 35 to 75 (mean of 57 years). Three had developed symptoms of gustatory hyperlacrimation following an episode of idiopathic facial paralysis more than a year earlier (range 1–4 years). The fourth developed symptoms following an ear infection 8 years previously. None of the patients was affected by involuntary synkinesia of the facial muscles or gustatory sweating. The demographic data of the patients, including the main clinical features, are shown in Table 1.
Patients were asked to complete a questionnaire with numeric analog scales to assess the frequency and severity of the symptoms. A complete ophthalmic examination was performed which included measurements and description of the lid position, blink reflex, corneal sensation, quality of the corneal epithelial surface and tear break-up time. Tear secretion was documented by Schirmer’s test. The patients were then given a sweet-sour candy to stimulate the gustatory reflex (Sherbet Lemons, Bassett’s Fundays) and Schirmer’s test was repeated.
Treatment initially consisted of injecting 10 U of BTX-A into the lacrimal gland of the affected side via a transcutaneous route. Five hundred units of lyophilised botulinum toxin type A (Dysport®, Ipsen Ltd, Berks, UK) were reconstituted in 2.5 ml of 0.9% NaCl. The patients were asked to look inferonasally away from the affected lacrimal gland. The injection site was identified inferior to the superior orbital rim, at the junction between the lateral and medial third of the orbital rim. Ten units of botulinum toxin were injected slowly to a depth of 4–5 mm with a 30-gauge needle, bevel pointing away from the levator muscle (Figure 2).
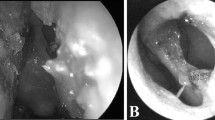
Patient 1 requested further treatment after 3.5 months when the effect of BTX-A wore off. He had initially developed a small ptosis after the first treatment and therefore to deliver the toxin more directly and reduce the chance of inducing further ptosis, this further injection of toxin was delivered transconjunctivally to the palpebral lobe of the lacrimal gland. Topical anaesthetic was applied, the lid double everted and gentle pressure applied at the lateral canthal area to expose the lacrimal gland. The gland was then injected under direct vision (Figure 3). The fourth patient, who was recruited into the study at a later date than the other patients, was also treated transconjunctivally as we felt that injection under direct vision was more accurate and potentially carried less risk of side effects.
All patients were reviewed at 1 week, 1 month, 3 months and 6 months after the initial injection. At each visit the severity and frequency of the symptoms, as well as a complete ophthalmic examination were recorded. Any complications were noted. Further injections were given at the request of the patient. Special care was taken to document the duration of the changes in the reflex lacrimation and any side effects.
Results
At 1 week follow-up none of the three patients who had 10 U of BTX-A injected subcutaneously reported an improvement in symptoms. Therefore all three were treated with a second injection of 10 U 1 week after the first treatment. Following this second injection, all patients reported an almost complete resolution of symptoms within 4 days. The fourth patient had relief of symptoms following injection of 10 U of BTX-A under direct vision using the transconjunctival method of injection. Table 2 summarizes the effect of treatment.
Prior to treatment a Schirmer’s test under taste stimulation showed an increase in tear production on the affected side as would be expected. Following treatment with BTX-A, tear production whilst eating decreased progressively and reached levels comparable to those produced without the gustatory stimulus. Figure 4 shows the Schirmer’s test results of the affected eye of the treated patients at the initial baseline visit and following treatment.
Patients 1 and 4 noticed a return of symptoms 3.5 months after the initial injections and were therefore given a further BTX-A injection transconjunctivally at this time. Patients 2 and 3 continued to be free of symptoms at the 6-month follow-up visit. There was no apparent relationship between the severity of symptoms, duration of symptoms or degree of facial weakness and the effect of the treatment. Figure 5 shows the change in severity of symptoms following the injection of BTX-A.
All patients experienced some minor side effects. Patient 1, who already had a 1 mm difference in the position of the upper lids prior to treatment, developed a 2 mm ptosis on the treated side. This presented 3 days after the second injection of 10 U of BTX-A and lasted for 2.5 months. The lid position remained unaltered in this patient after 20 U of BTX-A were injected transconjunctivally into the lacrimal gland. Patients 2 and 4 complained of mild stinging and dryness of the treated eye even though the pre-therapeutic Schirmer test was not suggestive of poor background tear production. These symptoms lasted approximately 2 months and were easily controlled with a supplement of artificial tears. Patient 3 did not develop any ocular complications apart from an occasional conscious awareness of the presence of the eye (‘that the eye was there’). None of the patients experienced diplopia or systemic side effects and the blink reflex, corneal sensation, tear break up time, and corneal epithelium remained unchanged during the follow-up period.
Discussion
BTX-A acts to block the release of acetycholine in the neuromuscular and cholinergic nerve junctions. Prior to its use in the treatment of CTS it has been used similarly in Frey’s syndrome (gustatory sweating) to stop transmission of impulses along aberrant autonomic nerve fibres to the sweat glands.10,11,12
The first reports describing the use of BTX-A in the treatment of gustatory hyperlacrimation appear in the literature in 1998. Boroojerdi et al6 initially published two cases of patients who had reflex lacrimation treated in this way. He also reported a further four patients who had BTX-A injection into the orbicularis oculi for involuntary synkinesia and coincidentally noted an improvement of their coexistent symptoms of reflex hyperlacrimation. Four months later Hofmann7 first presented two patients at the annual meeting of the ASOPRS who were successfully treated with injections of BTX-A. Reimann et al8 also reported a single case of CTS following idiopathic facial nerve palsy successfully treated with transconjunctival injection of BTX-A into the lacrimal gland. In our study all patients experienced a significant decrease in gustatory hyperlacrimation after BTX-A was injected into the lacrimal gland. This was demonstrated by a measured reduction in tearing in response to a taste stimulus as measured by the Schirmer test, and by a reduction in the frequency and severity of symptoms as reported by the patients. We found the duration of effect to be the same as reported in other studies and slightly longer than the recovery of orbicularis function following BTX-A injection for blepharospasm.13,14 The difference in duration of symptoms between the two patient groups may be due to a difference in time taken for axonal nerve sprouting following BTX-A injection at different sites, although there are no specific studies looking at this.
The cases reported so far in the literature have not all used the same preparations of BTX-A, or used the same route of injection and it is important to appreciate this when reviewing the literature.Footnote 1 Hofmann7 treated his patients with a transcutaneous injection of 15 U of BOTOX® without direct visualisation of the gland. Reiman et al8 however obtained nearly a complete resolution of the CTS symptoms with only half that dose, using the transconjunctival route. Boroojerdi et al6 used Dysport® injected transcutaneously. We obtained improvement in reflex hyperlacrimation with 20 U injected into the lacrimal gland, initially via a transcutaneous route but later progressing to a transconjunctival route with direct visualisation of the gland. We would recommend that older patients receive an initial dose of only 15 U to avoid inducing dry eye syndrome. For a greater effect further toxin can be injected later in a stepwise manner.
We found the best method of injection to be transconjunctival, as did Reimann et al.8 With this approach one can be more confident that the entire amount of BTX-A is delivered directly into the lacrimal gland. This may explain why Reimann et al8 were able to treat their patients with half the dose of BOTOX® than that used by Hofmann.7
In summary we conclude from our initial experience with the use of BTX-A that it is effective in treating gustatory hyperlacrimation when injected into the lacrimal gland. CTS is however a rare condition and patients must be warned about possible side effects and followed closely during their course of treatment. Complications may be avoided by careful selection of dose of toxin and transconjunctival injection into the palpebral lobe of the lacrimal gland.
Notes
There are two commercially available preparations of BTX-A: BOTOX® which originated in the USA and Dysport® in the UK, both of which are available in the UK. There is no exact conversion factor between the two, but 1 U of BOTOX® is approximately equivalent to 3–6 U of Dysport®.
References
Chorobski J . The syndrome of crocodile tears. Arch Neurol Psych 1951; 65: 299–318
Axelsson A, Laage-Hellman J . The gusto-lachrymal reflex. Acta Otolaryngol 1962; 54: 239–254
McCoy FJ, Goodman RC . The crocodile tear syndrome. Plast Reconstr Surg 1979; 63: 58–62
Ramsay J, Taylor D . Congenital crocodile tears: a key to the aetiology of Duane’s syndrome. Br J Ophthalomol 1980; 64: 518–522
Sadjadpour K . Postfacial palsy phenomena: faulty nerve regeneration or ephaptic transmission?. Brain Res 1975; 95: 403–406
Boroojerdi B, Ferbert A, Schwarz M et al. Botulinum toxin treatment of synkinesia and hyperlacrimation after facial palsy. J Neurol Neurosurg Psychiatry 1998; 65: 111–114
Hofmann RJ . Treatment of Frey’s syndrome (gustatory sweating) and crocodile tears’ (gustatory epiphora) with purified botulinum toxin. Ophth Pl Recon Surg 2000; 4: 289–291
Reimann R, Pfennigsdorf S, Reimann E et al. Successful treatment of crocodile tears by injection of botulinum toxin into the lacrimal gland. Ophthalmology 1999; 106: 2322–2324
House JW, Brackmann DE . Facial nerve grading system. Otolaryngol Head Neck Surg 1985; 93: 146–147
Drobik C, Laskawi R . Frey’s syndrome: treatment with botulinum toxin. Acta Otolaryngol (Stockh) 1995; 115: 459–461
Schulze-Bonhage A, Schröeder M, Ferbert A . Botulinum toxin in the therapy of gustatory sweating. J Neurol 1996; 243: 143–146
Bjerkhoel A, Trobbe O . Frey’s syndrome: treatment with botulinum toxin. J Laryngol Otol 1997; 111: 839–844
Dutton JJ . Botulinum—a toxin in the treatment of craniocervical muscle spasms: short-and long-term, local and systemic effects. Surv Ophthalmol 1996; 41: 51–65
Borodic GE, Joseph M, Fay L et al. Botulinum toxin for thr treatment of spasmodic torticollis: dysphagia and regional toxin spread. Head and Neck 1990; 12: 392–398
Author information
Authors and Affiliations
Corresponding author
Additional information
Presented as a poster at the Royal College of Ophthalmologists Congress 2000. The authors received no funding for this work
Rights and permissions
About this article
Cite this article
Montoya, F., Riddell, C., Caesar, R. et al. Treatment of gustatory hyperlacrimation (crocodile tears) with injection of botulinum toxin into the lacrimal gland. Eye 16, 705–709 (2002). https://doi.org/10.1038/sj.eye.6700230
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6700230
Keywords
This article is cited by
-
Comparison of botulinum toxin-A injection in lacrimal gland and conjunctivodacryocystorhinostomy for treatment of epiphora due to proximal lacrimal system obstruction
Eye (2016)
-
Botulinum toxin therapy: its use for neurological disorders of the autonomic nervous system
Journal of Neurology (2013)
-
Botulinumtoxin für die Behandlung sekretorischer Störungen im Kopf-Hals-Bereich
HNO (2012)
-
Botulinumtoxin bei Überfunktion der Tränendrüse, spastischem Entropium und Oberlidretraktion bei endokriner Orbitopathie
Der Ophthalmologe (2007)