Abstract
Purpose To investigate the effectiveness of aspiration of expired air by a suction system on peripheral oxygen saturation (SpO2) and end tidal carbon dioxide (EtCO2) during cataract surgery.
Materials and methods In total, 160 pre-medicated patients aged between 40 and 70 years (ASA I–III, classification of patients according to the American Society of Anesthesiologists) scheduled for cataract surgery under retrobulbar or peribulbar block were examined in a randomised, single-blind manner. The patients were sedated with 3 mg midazolam i.v. 15 min before operation and were monitored with an anaesthesia monitor. Heart rate (HR), non-invasive mean arterial pressure (MAP), SpO2 and EtCO2 were continuously measured using a standardised monitor. The first group (non-suction group, n=80) received 4 L min−1 O2 with nasal cannule while the second group (suction group, n=80) received 4 L min−1 O2 with nasal cannule, and the expired air was aspired with a Y-piece suction system. EtCO2 was measured with the line of the sampling tube in the anaesthesia monitor. Respiratory rate (RR) was counted for a period of 1 min at each measurement time with thoracic excursions. The results were evaluated by unpaired t-test and analysis of variance.
Results Severe reduction of SpO2 and raising of EtCO2 were observed significantly in the first group during the operation. RR, HR and MAP increased due to hypoxaemia. In the second group, SpO2 was stabilised at high levels and EtCO2 did not increase. RR, HR and MAP levels remained within the normal limits. Differences between the two groups were statistically significant (P<0.05).
Conclusion During cataract surgery with local anaesthesia, SpO2 decreases and RR, HR and MAP increase because of reinspiration of expired air under the drape. Insufflation of O2 and aspiration of expired air with a suction system have prevented severe reduction of SpO2 and raising of EtCO2. It was suggested that O2 delivery and use of an aspiration system decreased the risk of hypoxaemia significantly in the patients undergoing the cataract surgery.
Similar content being viewed by others
Introduction
Patients undergoing cataract surgery represent a high-risk group because of their age and frequently coexisting cardiac, pulmonary or neurological diseases.1 During local anaesthesia and throughout the surgery all patients should be carefully monitored, because pre-medication, surgical draping, the use of intra-operative sedatives and the local anaesthetic agent itself may predispose the patients to the risk of hypoxaemia.1,2,3
Surgical draping causes rebreathing of carbon dioxide. A decrease in the fraction of inspired oxygen rate (FiO2) causes a decrease in the peripheral oxygen saturation (SpO2) and an increase in end tidal carbon dioxide (EtCO2).2,3,4 The entrance of oxygen (5–10 L min−1) and the suction system under the drape reduces the rate of expired carbon dioxide.5,6,7,8,9 The use of a nasal cannule and a Y-shaped suction system may provide more effective ventilation.4
The aim of the present study was to investigate the effectiveness of aspiration of expired air by a suction system on SpO2 and EtCO2 during cataract surgery.
Materials and methods
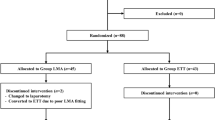
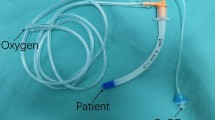
After receiving informed consent, 160 pre-medicated patients aged between 40 and 70 years scheduled for cataract surgery under retrobulbar or peribulbar block were examined in a randomised, single-blind manner. The patients included in ASA I–III (Table 1) were enrolled into the study. Patients with pre-existing severe cardiovascular disease, severe renal or hepatic dysfunction, non-regulated diabetes mellitus, non-stable chronic obstructive lung disease, and non-regulated hypertension were not included in the study. All consecutive suitable patients who met the inclusion criteria were randomly allocated to one of the two groups. In the first group 80 patients (non-suction) received only oxygen insufflation, while in the second group 80 patients (suction, n=80) were provided with suction and oxygen supply. All patients were given isolyte-S solution with venous cannule. The patients were sedated with 3 mg midazolam i.v. 15 min before operation and were monitored with an anaesthesia monitor (Datex-Ohmeda ADU AS/3, Finland or Cicero EM, Germany). Heart rate (HR), respiratory rate (RR), non-invasive mean arterial pressure (MAP), SpO2 and EtCO2 were continuously measured using a standardised monitor. SpO2 was measured with a finger probe and EtCO2 was measured using the line of the sampling tube in the anaesthesia monitor. RR was counted for a period of 1 min at each measurement time with thoracic excursions. All measurements were taken at baseline, block, 10, 20, 30, 40, 50 and 60 mins after starting monitoring. Both groups received 4 L min−1 O2 with nasal cannule. In the suction group, the expired air under the drape was aspired with a Y-piece suction system (Y TUR package, Biçakçilar, Turkey). In both groups, a maximal monitoring time of 60 min was taken for analysis. The patients monitored for more than 60 min were not included in the study. An SpO2 value under 85 mmHg was the exclusion criterion.
During the interval between monitoring and draping, the patient was prepared for surgery. After retrobulbar or peribulbar anaesthesia was performed, the study equipment was placed over the chin of the patient. A large sterile drape that did not contain rubber latex (ophthalmic drape 120×170 cm, with pouch, custom sterile, Allegiance/Allergan) was placed over each patient's head, including the eye to be operated. After draping the patient's head, 4 L min−1 O2 was continuously insufflated through the oxygen tube in each group. In the suction group the ambient air was also suctioned off during the entire course of the operation. Expected surgery time was estimated to be between 25 and 45 mins. A phacoemulsification procedure was performed (Diplomax, Allergan). The patients whose surgery took longer than the expected time were excluded. As soon as the operation was completed, the drapes were removed from the head and the suction equipment withdrawn.
Demographic data were compared by using the unpaired t-test. The effects within the groups were evaluated by analysis of variance (ANOVA). The effects between the groups at the same points were evaluated by unpaired t-test. P<0.05 was considered statistically significant. Results were expressed as mean (SD).
Results
Three patients in the non-suction group and two patients in the suction group were excluded from the study because of intraoperative unexpected sudden movement. Thirteen patients in the non-suction group developed undesired systemic events. All systemic events were detected in a timely manner and resulted in rapid intervention and full recovery. Among these patients, four developed cardiac arrhythmia. These patients were managed with β1 selective blocker metaprolol tartrate IV (below 1 mg mL−1). The same dose was repeated in poorly responsive patients. Nine patients developed hypoxia and systemic hypertension and were treated with anti-hypertensive drugs (enalapril 10 mg/i.v.). Three patients showed uneasiness and received additional sedation (midazolam 3 mg/i.v.). SpO2 did not decrease to under 85 mmHg in any of the patients.
The systemic monitoring data of 77 patients in the non-suction group and 78 in the suction group were analysed. Mean surgery time was 37.8±7.05 in the non-suction group and 41.2±6.28 in the suction group. Demographic data, mean surgery time and baseline measurement of SpO2 and EtCO2 were similar in both groups (Table 2). RR, HR and MAP increased significantly when compared with the suction group (Figure 1). Reduction of SpO2 and raising of EtCO2 was observed significantly in the non-suction group during the operation. In the suction group, SpO2 was stabilised at high levels and EtCO2 did not increase (Figures 2 and 3). RR, HR and MAP levels remained within the normal limits. Differences within the two groups were statistically significant (P<0.05).
Values of MAP, HR and RR in both groups. The upper two line values represent mean MAP measurement, the middle two lines represent mean HR values and the lower two lines represent RR values. The lines with symbols indicate the non-suction group. (P<0.05, comparing the suction group and the non-suction group except baseline, block and 10 min.)
Discussion
Systemic complications such as cardiac arrhythmia, respiratory arrest and hypertension are rarely seen during cataract surgery under local anaesthesia. Development of any systemic complication can lead to significant mortality and morbidity.10 The complications observed in cataract surgery are usually due to local anaesthesia. Systemic undesired events such as tachycardia and hypertension may develop during the surgical procedure resulting from hypoxaemia and hypercapnia. Hypoxaemia may occur due to concomitant systemic disease, surgical draping, medication and local anaesthetics.10 Surgical draping is important for sterile working in a surgical area. After draping the face, patients rebreathe the expirated air under the drape. Therefore, most patients complain of uneasiness resulting from difficulty in breathing. SpO2 and EtCO2 are measured to investigate a patient's situation regarding hypoxia and hypercapnia. SpO2 shows tissue oxygenation and perfusion by measuring transcutaneous oxyhaemoglobin (infrared light, 990 nm) and deoxyhaemoglobin (red light, 660 nm). The normal value of SpO2 is 100% and a value under 90% means that the arterial oxygen pressure (PaO2, range 60–80 mmHg) is under 65 mmHg. A decrease in FiO2 and an increase in FiCO2 cause a decrease in SpO2 and an increase in EtCO2.2,3,4 Hypoxia and hypercapnia owing to a decrease in SpO2 give rise to uneasiness and agitation.
EtCO2 is the rate of end expiration peak CO2. It shows sufficiency of inspiration/expiration via a non-invasive method. The normal value of EtCO2 is between 35 and 45 mmHg. With EtCO2 under 30 mmHg, vasoconstriction and a decrease in blood flow to the brain has been observed. If EtCO2 is above 45 mmHg, vasodilatation and an increase in blood flow occur. Sufficiency of ventilation provides a required brain blood flow through stable PaCO2.11 Hypoxia and hypercapnia cause an increase in HR, RR and MAP.11
Hypoxia and hypercapnia lead to impairment of cognitive functions. As a result, agitation and anxiety have been seen especially in geriatric patients. This agitation sometimes affects surgery. Furthermore, higher PaCO2 values result in raised choroidal blood flow and intra-ocular pressure. This in turn may complicate the operation.12 Effective and tolerable O2 can be given via a nasal cannule at a rate of 5–10 L min−1. O2 applied with a face mask causes drying of mucous membrane and decreasing of tolerance.13 An oxygen flow of 2−4 L min−1 is sufficient to keep SpO2 values within normal ranges. No high flow of oxygen is necessary to prevent hypercapnia and hypoxia when combined with suction.4
Schlager et al3,4 have designed new equipment to prevent carbon dioxide rebreathing during ocular surgery. They used a tube that has two free ends like a Y-shaped connector for suction. A similar suction system was used in the current study.
In our study, the suction system significantly decreased carbon dioxide accumulation under the drape. SpO2 remained high throughout the surgery. This prevented undesired systemic events and offered more comfortable surgery. The results suggested that the suction system is as important as giving oxygen in improving SpO2 and EtCO2 in patients undergoing cataract surgery under local anaesthesia.
References
Palve H, Melkkila TA . Oxygenation during local anaesthesia for cataract surgery. Acta Anaesthesiol Scand 1991; 35: 181–184.
Heinze J, Rohc M . General anesthesia vs retrobulbar anesthesia in cataract surgery. A randomised comparison of patient at risk. Anaesthesist 1992; 41: 481–488.
Schlager A, Loren IH, Luger TJ . Transcutaneous CO2/O2 and CO2/air suction in patients undergoing cataract surgery with retrobulbar anaesthesia. Anaesthesia 1998; 53: 1212–1218.
Schlager A, Staud H . New equipment to prevent carbon dioxide rebreathing during eye surgery under retrobulbar anaesthesia. Br J Ophthalmol 1999; 83: 1131–1134.
Kobel M, Rifat K, Roth A . Accumulation of carbon dioxide in the operative field in ophthalmic interventions under local anaesthesia. Ophthalmologica 1984; 188: 135–140.
Ramanathan S, Capan L, Chalon J, Rand PB, Klein GS, Turndorf H . Mini environmental control under the drapes during operation on the eyes of conscious patients. Anesthesiology 1978; 48: 286–288.
Sabo B, Smith RB, Gilbert TJ . Evaluation of rebreathing in patients undergoing cataract surgery. Ophthalmic Surg 1988; 19: 249–251.
Zeitlin GL, Hobin K, Platt J, Woitkoski N . Accumulation of carbon dioxide during eye surgery. J Clin Anesth 1989; 1: 262–267.
Michel AMJ, Stott SA, Sanders DJ . End-tidal oxygen concentrations produced by oxygen delivered through nasal cannule. Br J Anaesth 1995; 75: 2.
Jayamanne DGR, Gillie RF . The effectiveness of peri-operative cardiac monitoring and pulse oximetry. Eye 1996; 10: 130–132.
Morgan GE, Mikhail MS. Clinical Anesthesiology, 2nd ed, Chapter 6. A Lange Medical Book. Appleton & Lange A Simon & Schuster Company: New York, 1996, p 94.
Hvidberg A, Kessing SV, Fernandes A . Effects of changes in PCO2 and body position on intraocular pressure during general anaesthesia. Acta Ophthalmol 1981; 59: 465–475.
Crosby ET, Halpern SH . Supplemental maternal oxygen therapy during caesarean section under epidural anaesthesia; a comparison of nasal prongs and facemask. Can J Anaesth 1992; 39: 4.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Inan, Ü., Sivaci, R. & Öztürk, F. Effectiveness of oxygenation and suction in cataract surgery: is suction of CO2-enriched air under the drape during cataract surgery necessary?. Eye 17, 74–78 (2003). https://doi.org/10.1038/sj.eye.6700223
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6700223
Keywords
This article is cited by
-
Intravenous magnesium-fentanyl sedation versus midazolam-fentanyl sedation before local anesthesia for eye surgery: a comparative study
Ain-Shams Journal of Anesthesiology (2018)
-
Is suction of CO2-enriched air under the drape during cataract surgery necessary
Eye (2004)