Abstract
Purpose To report four cases of cranial nerve palsy, which presented to the ophthalmologist as the only or one of the earliest manifestations of prostatic carcinoma. This is an infrequent complication of metastatic prostatic carcinoma usually only occurring late in the disease process in those with a history of prostatic carcinoma.
Methods The case records of four patients with a history of a cranial nerve palsy who attended the ophthalmology department and who had a recent or subsequent diagnosis of prostatic carcinoma were reviewed.
Results Diplopia caused by lesions affecting the third and sixth nerves sometimes in association with sensory symptoms may be a manifestation of metastatic prostatic carcinoma. These findings are consistent with base of the skull metastases from the condition.
Two patients are still alive 54 months and 12 months after the diagnosis. One of the patients died 13 months after the diagnosis of prostatic carcinoma was made and the other died 21 months after the diagnosis from an unrelated hypertensive brain haemorrhage.
Conclusion Any patient presenting with diplopia must have an adequate past medical history taken and in an elderly gentleman this should include symptoms of prostatic disease. If indicated urological referral and measurement of prostate specific antigen may be performed.
In patients whose cranial nerve palsy is complicated by other sensory signs or those in whom no sign of recovery occurs in 2 months, a contrast CT scan asking for bone windows to be included may be helpful in delineating any pathology.
Radiotherapy may be useful for the treatment of metastatic prostatic carcinoma causing cranial nerve palsies with some patients experiencing either complete or partial resolution of their symptoms. The effect of newer hormonal agents or chemotherapy on this aspect of the disease is not well documented in current literature.
Similar content being viewed by others
Main
Base of the skull metastases are a rare but documented late complication of metastatic prostatic carcinoma, which can give rise to cranial nerve palsies.1 We report four cases, which were unusual in that the nerve palsy was the presenting feature of the disease in two cases and a recent diagnosis of prostatic carcinoma had been made in the other two.
Case reports
Case 1
A 66-year-old male presented with facial tingling, which resolved and was followed by the onset of diplopia.
Extraocular movements revealed limitation of upgaze, adduction and depression in both eyes with full abduction. Slight bilateral ptosis was noted. The right pupil was dilated and unreactive to light and accommodation but the left pupil was normal. The remainder of the physical and neurological examinations were unremarkable. Investigations (blood pressure, full blood picture, ESR, blood sugar, liver function tests, calcium and phosphate) were normal apart from a raised alkaline phosphatase at 912 IU/l (normal >120 IU/l). Iso-enzyme analysis of alkaline phosphatase was not performed. However in retrospect considering the liver function tests were otherwise normal the raised alkaline phosphatase was most likely bony in origin.
CT scans of abdomen and chest as well as ultrasound examination of the liver were normal. Several old lacunar infarcts in both parietal lobes were noted on a non-contrast CT of brain. A MRI scan of the brain was arranged.
Three months later the patient complained of the insidious development of bilateral ptosis. Ophthalmological examination now showed an almost complete 3rd nerve palsy on the right as well as on the left side (Figure 1a). Fourth and sixth nerves were intact. Both pupils were now dilated and unreactive to light.
(a) Eye movements showing an almost complete third nerve palsy on the right as well as on the left side. (b) Contrast enhanced CT scan showing extensive bony thickening and sclerosis centred in the bony margins of the sphenoid sinus with encroachment on the sinus cavity and extending laterally along the sphenoid wing into the upper part of the clivus.
A contrast CT scan including bone windows arranged to investigate the sphenoid sinus changes noted on a recent MRI showed significant bony overgrowth consistent with sclerotic metastases (Figure 1b). This encroached into the sinus cavity resulting in compression of the third and fifth nerves in the lateral wall of the cavernous sinus. Prostate specific antigen (PSA) was markedly elevated at 2768 ng/ml (normal range 0–6.5 ng/ml) and subsequent prostate gland biopsy confirmed the diagnosis of prostatic carcinoma. Plain X-ray of the lumbosacral spine showed bony sclerosis in keeping with metastatic prostatic carcinoma. The patient was commenced on cyproterone acetate and goserelin injections. The third nerve palsies improved slightly with better lid opening being the most beneficial factor noted by the patient.
Twenty-one months after the start of symptoms he was admitted to hospital with right-sided weakness and decreased consciousness. Emergency CT scan of the brain showed a hypertensive haemorrhage in the region of the basal ganglia and thalamus with extension into the ventricles from which the patient subsequently died.
Case 2
A 76-year-old male presented with a 1-month history of binocular horizontal diplopia. Past medical history included a recent prostatectomy, which histologically showed the presence of a moderately differentiated prostatic adenocarcinoma. Prostate specific antigen was 414 ng/l.
An isolated right sixth nerve palsy was noted on extraocular movements. At follow-up 8 months later the sixth nerve palsy had almost completely resolved. However 2 months later he reattended with a recurrence of the right sixth nerve palsy. Isotope bone scan showed widespread bony metastases including tracer uptake involving the base of the skull vault. A CT scan brain was ordered and revealed a destructive lesion in the upper part of the right clivus (Figure 2). The patient was referred to Oncology for assessment for possible radiotherapy but declined any further intervention and died 3 months later.
Case 3
A 68-year-old male presented with a 2-week history of binocular horizontal diplopia and was found to have a right sixth nerve palsy.
After 8 months of continuous review there was only a slight improvement in the nerve palsy and in the interim it emerged that the patient had been diagnosed as having prostate cancer.
A CT scan was performed which revealed an enhancing mass lesion in the pituitary fossa, which had eroded into the right and left cavernous sinus (Figure 3). Pituitary function tests were normal but PSA was 619.5 ng/ml.
To confirm the possible diagnosis of metastatic prostatic carcinoma the lesion was biopsied and a transphenoidal decompression of the pituitary performed. Histology showed a tumour that was diffusely infiltrative and demonstrated glandular differentiation. Immunohistochemical staining was strongly positive for PSA. Four and a half years later the patient is still alive having been treated with flutamide and goserelin injections as well as radiotherapy to the pituitary region.
Case 4
A 64-year-old male presented with a 1-day history of binocular horizontal diplopia. Past medical history included a diagnosis of prostatic carcinoma confirmed on biopsy the previous week.
On examination he was found to have right sixth nerve palsy. Two months later he attended with numbness down the right side of his face and was also found to have impaired right corneal sensation.
A CT scan of the brain revealed bony destruction involving the right petrous apex. There was also a soft tissue mass extending anteriorly into the paracavernous region explaining fifth nerve involvement (Figure 4).
One year later he is under review by the oncologists and is currently on hormonal treatment.
Discussion
Prostatic carcinoma is the second most common cancer in men and is currently receiving much attention from both medical and public sources. It is infrequently associated with cranial nerve palsies, which usually occur many years after the initial diagnosis. The metastatic lesions either compress or infiltrate the affected nerves.1 Our cases demonstrate the importance of considering prostatic carcinoma as a possible cause of multiple, persistent or prolonged cranial nerve palsies in men over the age of 60 years even in those without a history of the disease.
Unilateral third nerve palsies have been associated with prostatic carcinoma.2 This is the first case report of bilateral pupil involving third nerve palsy and the second case report of an isolated sixth nerve palsy secondary to a destructive lesion in the clivus being the presenting features of prostatic carcinoma.3
Bilateral third nerve palsy is a rare occurrence. In a series by Richards et al looking at the causes and prognosis of 4278 cases of paralysis of the third, fourth and sixth nerves there were only nine bilateral third nerve palsies. Five were complete and four were a mixture of partial and complete. In this series three of the bilateral third nerve palsies were of undetermined cause, three were due to trauma and three were classified under ‘others’. The authors did not specify what these ‘others’ were.4
Reviewing the literature there are case reports of bilateral third nerve palsy as complications of Tolosa–Hunt syndrome, oligodendroglioma, head injury and pituitary apoplexy but none were found secondary to prostatic carcinoma. It is interesting to note that in Case 1 the initial non-contrast CT scan did not reveal the bony sclerosis. The radiologists therefore recommend ordering a contrast CT scan asking for bone windows to be included in those patients with a history of prostatic carcinoma.
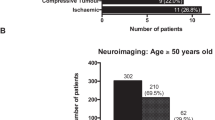
The prognosis 10 years ago from prostatic carcinoma was typically very poor when a cranial nerve palsy was present, survival being only a few months.4,5,6 In a case series by Ransom of 11 patients with base of the skull metastases from prostatic carcinoma, bony abnormalities similar to those in our patients were found in the clivus, parasellar and sphenoid regions affecting the 3rd, 5th and 6th nerves.5 In Ransom’s series the median survival time from the diagnosis of cranial nerve involvement was 4 months. Interestingly two of his patients presented with cranial nerve involvement and on subsequent investigation were found to have carcinoma of the prostate. These patients like our cases have a longer than expected survival and were still alive 42 and 84 months after the diagnosis.5
At the present time metastatic prostate carcinoma remains incurable. However the use of combined androgen blockade seems to improve survival and quality of life. For painful bone lesions, external beam radiotherapy, bisphosphonates, and strontium 89 or samarium 153 provide pain relief.7 The use of combination chemotherapy to improve survival in hormone refractory prostate cancer has also been receiving a lot of attention.8
If metastatic prostatic carcinoma is causing cranial nerve deficits, radiotherapy seems to result in a beneficial response with either complete or partial resolution of these deficits in most patients2,5,6 Therefore it is felt that radiotherapy does offer a palliative treatment with a short term of improved quality of life for these patients. Svare believes radiotherapy should be started as soon as possible after the diagnosis of cranial nerve dysfunction because the longer the symptom persists the poorer the result.1 It is not well documented if the newer hormonal treatments and chemotherapy for metastatic prostate carcinoma have any effect on the cranial nerve deficit. However the patient in Case 1 did show a slight improvement in signs with better opening of the eyelids since starting cyproterone acetate and goserelin injections.
In conclusion, the ophthalmologist should take a careful history including neurological symptoms from men with cranial nerve palsies. Those patients with multiple progressive or persistent cranial nerve palsies merit further investigation including PSA levels and possibly a contrast CT scan with bone windows to rule out sinister underlying causes of these symptoms.
References
Svare A, Fossa SD, Heier MS . Cranial nerve dysfunction in metastatic cancer of the prostate. Br J Urol 1988; 61: 441–444
Cullom ME, Savino PJ . Adenocarcinoma of the prostate presenting as a third nerve palsy. Neurology 1993; 43: 2146–2147
O’Boyle JE, Gardner TA, Olivia A et al. Sixth nerve palsy as the presenting sign of metastatic prostate cancer. A case report and review of the literature. J Clin Neuroophthalmol 1992; 12: 149–153
Richards BW, Jones RJ, Younge BR . Causes and prognosis in 4278 cases of paralysis of the oculomotor, trochlear, and abducens cranial nerves. Am J Ophthalmol 1992; 113: 489–496
Ransom DT, Dinapoli RP, Richardson RL . Cranial nerve lesions due to base of the skull metastases in prostate carcinoma. Cancer 1990; 65: 586–589
Seymore CH, Pepples WJ . Cranial nerve involvement with carcinoma of the prostate. Urology 1998; 31: 211–213
Auclerc G, Antoine EC, Cajfinger F, Brunet-Pommeyrol A, Agazia C, Khayat D . Management of advanced prostate cancer. Oncologist 2000; 5: 36–44
Milliken RE . Chemotherapy of advanced prostatic carcinoma. Semin Oncol 1999; 26: 185–191
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
McAvoy, C., Kamalarajab, S., Best, R. et al. Bilateral third and unilateral sixth nerve palsies as early presenting signs of metastatic prostatic carcinoma. Eye 16, 749–753 (2002). https://doi.org/10.1038/sj.eye.6700210
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6700210
Keywords
This article is cited by
-
Multiple cranial neuropathy as the initial presentation of metastatic prostate adenocarcinoma: case report and review of literature
Acta Neurochirurgica (2010)
-
Skull-base metastases
Journal of Neuro-Oncology (2005)