Abstract
Objective To evaluate the effects of diabetes mellitus, diabetic retinopathy and degree of blood glucose (BG) regulation on retinal nerve fiber layer (RNFL) thickness by using a scanning laser polarimeter (NFA-GDx).
Methods We prospectively assessed RNFL thickness in four groups of patients, who were all age matched. Diabetic patients without diabetic retinopathy were grouped according to their BG regulation level into two, as: BG-regulated group (BG <140 mg/dl, HbA1c <8%, fructosamine <285 μmol/l, TG <200 mg/dl, n = 50), and BG-non-regulated group (BG = 140–250 mg/dl, HbA1c >8%, fructosamine >285 μmol/l, TG >200 mg/dl, n = 44). A group of patients with nonproliferative diabetic retinopathy (NPDR) formed the 3rd group (n = 41). The 4th group consisted of healthy subjects and acted as a control group (n = 50). Symmetry, superior maximum, ellipse modulation and the average thickness variables of NFA-GDx were used for the assessment. ANOVA test was used for the statistical analysis of variables between groups.
Results The mean superior maximum and ellipse modulation values were statistically significantly lower than the control group in BG-non-regulated and NPDR groups (P < 0.05). The average thickness value was also statistically significantly lower than the control group in NPDR group. These values in the BG-regulated group were not statistically significantly different from the control group (P > 0.05).
Conclusions This is the first clinical study demonstrating the effects of diabetic glucose regulation level on RNFL by using NFA-GDx. RNFL thickness was seen to decrease with development of diabetic retinopathy and with impairment of metabolic regulation. This issue should be taken into account while assessing RNFL in diabetic glaucomatous patients.
Similar content being viewed by others
Main
Diabetic retinopathy (DR) is the most common ocular complication of diabetes mellitus (DM) and is one of the leading causes of blindness in developed countries. Although the long-term effects of DM on vascular tissues are very well known, its effect on retinal neurons is not very clear. Previous studies have demonstrated that DM causes an optic neuropathy, which was different from glaucomatous optic nerve damage,1,2 and the retinal nerve fiber layer (RNFL) defects were more prevalent in patients with DM.3 The effects of metabolic control level of DM on RNFL or optic nerve have not been demonstrated yet.
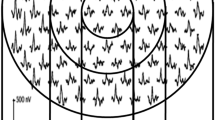
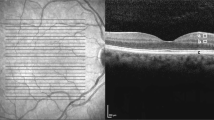
Scanning laser polarimeter (NFA-GDx; Laser Diagnostic Technologies, San Diego, CA, USA) is one of the first clinical devices for quantitative assessment of the retinal nerve fiber layer (RNFL) thickness in the living human eye. It measures the amount of retardation that is caused by specific arrangement of the microtubules of the retinal ganglion cells. When a polarized light beam passes through the microtubules in the RNFL, the light is shifted from phase. The amount of phase shift is called retardation and is correlated linearly with the thickness of the RNFL.4,5
In this study, we have evaluated the effects of DM, degree of metabolic control of DM and the presence of DR on RNFL thickness by using NFA-GDx.
Patients and methods
Consecutive diabetic patients who had been referred to ophthalmology clinics for retinal examination were included in the study. An informed consent was obtained from all of the patients. They all had an ophthalmologic examination with best-corrected visual acuity and intraocular pressure (IOP) measurements, slit lamp and fundus examinations. Patients with best-corrected visual acuity of less than 20/25, IOP >22 mmHg, C/D ratio >3/10, and any retinal disease other than DR and known glaucoma were excluded from the study. BG level, glycosylated hemoglobin (HbA1c) level, fructosamine level and triglyceride (TG) level were obtained for all of the patients with DM. HbA1c and TG levels are indicators of BG regulation within the last 3 months and the normal values are less than 8% for HbA1c and less than 200 mg/dl for TG. Blood fructosamine level, on the other hand, is an indicator of BG regulation within the last 2 weeks (normal value <285 μmol/l).
Type 2 diabetic patients without DR were assessed in two different groups according to degree of metabolic control of BG. Patients with minimal to moderate background DR (non-proliferative DR; NPDR) formed another group without paying attention to metabolic regulation of DM. The groups were determined as follows:
Group 1 comprised diabetic patients without DR and with fasting BG level less than 140 mg/dl, HbA1c level less than 8%, fructosamine level less than 285 μmol/l and TG level less than 200 mg/dl at the day of RNFL examination and were called ‘BG-Regulated group’.
Group 2 was composed of diabetic patients without DR and with fasting BG level between 140 and 250 mg/dl, HbA1c level ≥8%, fructosamine level ≥285 μmol/l and TG level ≥200 mg/dl at the day of RNFL examination and, were called ‘BG-Non-regulated group’.
Group 3 comprised diabetic patients with NPDR and they were not classified according to fasting BG, HbA1c, fructosamine or TG levels. They were called ‘NPDR group’. Patients with clinically apparent retinal edema and severe NPDR were not included in the study.
An age-matched control group (Group 4) was extracted randomly from our previous study on normal subjects.6
We measured the RNFL thickness in one eye of the patients by using a scanning laser polarimeter (NFA-GDx) which uses a light source consisting of a near infrared diode laser (wavelength: 780 nm). The field of view was 15°. The operator placed an ellipse corresponding to the rim of the optic disc and the machine’s software generated the measuring ellipse at 1.75 disc diameters. Multiple images were obtained for each eye and the best three images were selected to form the mean image, which was used for measurements. Our criteria for a good image were a sharply focused image, centrally located optic disc and equal illumination in all segments of the image. All of the measurements were performed by the same two experienced operators (SCO, YL) without pupil dilatation. We have used the four most popularized variables named: symmetry, superior maximum, ellipse modulation, and average thickness values of NFA-GDx for the analysis.7
ANOVA test was used for the statistical analysis of these variables between groups.
Results
A total of 135 diabetic patients out of 217 were enrolled in this prospective study. Patients were under treatment with either diet (14.8%), oral anti-diabetics (50.9%) or insulin (34.3%) for BG regulation. Some of the patient characteristics are presented in Table 1. Fifty patients with a mean age of 50.8 years (ranging between 34–72 years) were included in group 1 (regulated group). The second group (non-regulated group) involved 44 patients with a mean age of 49.8 (ranging between 25–80) years. Forty-one NPDR patients (mean age: 51.2 years) and 50 healthy subjects formed the group 3 (NPDR) and group 4 (control group) respectively. Measurements were performed in a total of 102 right eyes and 83 left eyes.
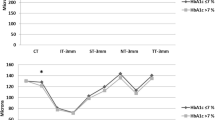
There was no significant difference with respect to age between groups (P > 0.05). Mean values of GDx variables for each group were presented in Table 2. There was no statistically significant difference between groups with respect to symmetry values (P > 0.214, ANOVA). Superior maximum values, on the other hand, were statistically significantly different between groups (P = 0.000 ANOVA). The mean superior maximum value was highest in the control group, followed by the regulated group, non-regulated group and NPDR groups in a decreasing order. Post hoc tests were used to find out the causative group for this significant difference. The difference was significant between control group and all the others except group 1 (regulated group) (P > 0.05 for regulated group and P = 0.000 for the other three groups, Dunnett).
Ellipse modulation values were also statistically significantly different between groups, being highest in the control group followed by group 1, 2 and 3 in a decreasing order (P = 0.008, ANOVA) (Table 2). Post hoc tests revealed that there was no significant difference between control group and group 1 (regulated group) (P > 0.05), while group 2 and 3 were significantly lower than the control group (P < 0.05, P < 0.05 and P < 0.01 respectively).
Average thickness values were also statistically significantly different between groups, being highest in the control group (P = 0.000 ANOVA) (Table 2). Post hoc tests revealed that the difference was not significant between control group and group 1 and 2 (P > 0.05), but significant difference was detected between control group and group 3 (P = 0.001).
Discussion
Optic neuropathy is a well-known problem limiting visual acuity in diabetic patients. There are, however, only a few papers reporting the changes in RNFL or optic disc in this patient group.1,2,3 Moreover, the papers reporting the effect of BG regulation on RNFL are even less.
Topographic features of eyes with diabetic optic neuropathy were reported to be very different from those with glaucomatous optic neuropathy in spite of the similar appearance of RNFL defects. The cup of the disc was not enlarged in diabetic eyes in spite of discrete signs of RNFL defects.2 The reduced visibility of the RNFL, the increased optic disc pallor and the unchanged size of the neuroretinal rim and parapapillary atrophy suggest that diabetes mellitus may be associated with nonglaucomatous optic nerve atrophy.1 Chihara reported the risk factors for RNFL defect as a higher level of diabetic retinopathy, systemic hypertension, and advanced age, but visual acuity, disc size, axial length, and HbA1c level at the time of examination were reported to be not correlated with these defects.3
The present study has confirmed the RNFL defects associated with DM, which was independent of retinopathy as determined by scanning laser polarimetry. We have found that there was a reduction of up to 15% in polarimetric measurements of diabetic patients as compared with control group. Scanning laser polarimeter is a widely used clinical device for the measurement of the RNFL thickness especially in glaucoma patients, however, it is an indirect measure. It measures the amount of retardation caused by birefringent structures in the eye, mainly the RNFL. Although the scanning laser polarimeter has a polarization compensator for the birefringent structures in the anterior segment, like cornea and lens, we do not know whether these changes exceed the capacity of the compensator or not. Additionally, the changes in crystalline lens related to fluctuations in blood glucose levels in diabetic patients may also affect the polarization and retardation measurements with NFA-GDx. Lastly, although we have excluded the patients with clinically apparent retinal edema, a possible subclinical retinal edema present in diabetic patients may interfere with the polarization effect. This issue should also be kept in mind, which may affect the reliability of measurements with scanning laser polarimeter in diabetic patients.
The mechanism for the development of optic neuropathy in diabetic patients is very complex. Several abnormalities in visual pathway functions in diabetic humans and animals have been reported. Amano et al reported that accumulation of advanced glycation end products in cribriform plates and around vessels in the optic nerve may contribute to the development of optic neuropathy in diabetic patients.8 Animal studies have demonstrated that diabetes affects retrograde axonal transport progressively through selective impairment of retinal ganglion cells and this impairment of retrograde axonal transport in large- and medium-sized retinal ganglion cells preceded optic nerve involvement.9,10
The effect of metabolic control of diabetes on optic nerve functions and RNFL seems positive. In a study on newly diagnosed young diabetics, the P100 latency in visual evoked potentials was significantly delayed as compared with the control group, which was seen to be normalized following good metabolic control.11 On the other hand, there are case reports reporting acute bilateral visual loss caused by diabetic ketoacidosis.12 This implies that optic neural tissue is vulnerable to hemodynamic and metabolic complications of diabetes. In the present study, polarimetric measurements in the group of good metabolic control (group 1) were very close to that of the control group (the difference was statistically insignificant), which implies the positive effect of good metabolic control on RNFL.
We have demonstrated that all of the studied NFA-GDx variables except symmetry were statistically significantly lower in diabetic patients with poor metabolic control as compared with the healthy control group (group 4) and the group of good metabolic control (group 1). The values were even lower in the group with diabetic retinopathy (group 3) independent of metabolic control. The symmetry was not affected in diabetic cases, which may be explained by a possibly symmetric loss of RNFL from the inferior and superior poles.
Hammes et al demonstrated that diabetes induces apoptosis in retinal ganglion cells and Müller cells in an experimental diabetes model.13 This study supports our findings in that RNFL thickness was decreased even in cases without diabetic retinopathy.
We have used the HbA1c and TG levels, which are indicators of metabolic control within the last 3 months, and fructosamine level, which is an indicator of metabolic control within the last 2 weeks in addition to BG levels as an indicator of metabolic control of diabetes. We have avoided using only the BG levels as an indicator of metabolic control of diabetes, which may have fluctuations even within a day.
The main drawback of this study, however, is the use of a limited number (four) of GDx variables for the assessment of RNFL to simplify the data and to save time. These variables, named symmetry, superior maximum, ellipse modulation and the average thickness are the most popularized GDx variables.7 Especially ellipse modulation, which was designed to capture the difference between the thickest and thinnest areas of the RNFL, was used to reflect relatively early loss of retinal nerve fibers.
To the best of our knowledge the present study is the first clinical study reporting the effect of metabolic control of diabetes on RNFL. We have demonstrated that the RNFL thickness tended to decrease with impairment of metabolic control in diabetic cases without retinopathy and with development of diabetic retinopathy. Since the association of glaucoma and DM is quite common, this issue should be taken into account while assessing RNFL in diabetic glaucomatous patients. When a decrease in RNFL thickness is detected in a diabetic glaucoma patient one should consider the metabolic state of diabetes and the presence of retinopathy which may cause RNFL loss themselves before considering progression of glaucomatous damage in these patients.
References
Konigsreuther KA, Jonas JB . Optic disc morphology in diabetes mellitus. Graefes Arch Clin Exp Ophthalmol 1995; 233: 200–204
Chihara E, Zhang S . Analysis of diabetic optic neuropathy with a topographic laser scanning system. Nippon Ganka Gakkas Zasshi 1998; 102: 431–435
Chihara E, Matsuoka T, Ogura Y, Matsumura M . Retinal nerve fiber layer defect as an early manifestation of diabetic retinopathy. Ophthalmology 1993; 100: 1147–1151
Weinreb RN, Dreher AW, Coleman A et al. Histopathologic validation of fourier-ellipsometry measurements of retinal nerve fibre layer thickness. Arch Ophthalmol 1990; 108: 557–560
Dreher AW, Reiter K, Weinreb RN . Spatially resolved birefringence of the retinal nerve fiber layer assessed with a retinal laser ellipsometer. Appl Opt 1992; 31: 3730–3735
Özdek SC, Önol M, Gürelik G, Hasanreisoğlu B . Scanning laser polarimetry in normal subjects and patients with myopia. Br J Ophthalmol 2000; 84: 264–267
Weinreb RN, Zangwill L, Berry CC, Bathija R, Sample PA . Detection of glaucoma with scanning laser polarimetry. Arch Ophthalmol 1998; 116: 1583–1589
Amano S, Kaji Y, Oshika T et al. Advanced glycation end products in human optic nerve head. Br J Ophthalmol 2001; 85: 52–55
Zhang L, Ino-ue M, Dong K, Yamamoto M . Retrograde axonal transport impairment of large- and medium-sized retinal ganglion cells in diabetic rat. Curr Eye Res 2000; 20: 131–136
Ino-Ue M, Zhang L, Naka H, Kuriyama H, Yamamoto M . Polyol metabolism of retrograde axonal transport in diabetic rat large optic nerve fiber. Invest Ophthalmol Vis Sci 2000; 41: 4055–4058
Verrotti A, Lobefalo L, Trotta D et al. Visual evoked potentials in young persons with newly diagnosed diabetes: a long-term follow-up. Dev Med Child Neurol 2000; 42: 240–244
Song SH, Mowbray A, O’Shea H, Campbell IW . Bilateral optic atrophy following diabetic ketoacidosis. Diabet Med 2000; 17: 394–396
Hammes HP, Federoff HJ, Brownlee M . Nerve growth factor prevents both neuroretinal programmed cell death and capillary pathology in experimental diabetes. Mol Med 1995; 1: 527–534
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was presented orally in XIII Congress of the European Society of Ophthalmology, Istanbul, Turkey (3–7 June 2001) None of the authors has a proprietary interest.
Rights and permissions
About this article
Cite this article
Özdek, S., Lonneville, Y., Önol, M. et al. Assessment of nerve fiber layer in diabetic patients with scanning laser polarimetry. Eye 16, 761–765 (2002). https://doi.org/10.1038/sj.eye.6700207
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6700207
Keywords
This article is cited by
-
Impacts of intravitreal anti-VEGF therapy on retinal anatomy and neurophysiology in diabetic macular edema
International Ophthalmology (2021)
-
Diabetic retinal neurodegeneration as a form of diabetic retinopathy
International Ophthalmology (2021)
-
The effect of fenofibrate on early retinal nerve fiber layer loss in type 2 diabetic patients: a case-control study
BMC Ophthalmology (2018)
-
Relationship between Systemic Vascular Characteristics and Retinal Nerve Fiber Layer Loss in Patients with Type 2 Diabetes
Scientific Reports (2018)
-
Caspases in retinal ganglion cell death and axon regeneration
Cell Death Discovery (2017)