Abstract
Testicular germ cell tumours (TGCTs) are the most common cause of cancer in men between the ages of 15 and 40 years, and, overall, the majority of patients should expect to be cured. The European Germ Cell Cancer Consensus Group has provided clear guidelines for the primary treatment of both seminoma and nonseminomatous germ cell tumours. There is, however, no international consensus on how best to follow patients after their initial management. This must promptly and reliably identify relapses without causing further harm. The standardising of follow-up would result in optimising risk-benefit ratios for individual patients, while ensuring economic use of resources. We have identified the seven common scenarios in managing seminomas and nonseminomas of the various stages and discuss the pertinent issues around relapse and follow-up. We review the available literature and present our comprehensive TGCT follow-up guidelines. Our protocols provide a pragmatic, easily accessible user-friendly basis for other centres to use or to adapt to suit their needs. Furthermore, this should enable future trials to address specific issues around follow-up giving meaningful and useful results.
Similar content being viewed by others
Background
Testicular germ cell tumours (TGCTs) are uncommon malignancies but the most common cause of cancer in men between the ages of 15 and 40 years. The peak incidence for nonseminomatous germ cell tumour (NSGCT) is between 20 and 30 years of age, and for seminoma between 30 and 40 years. In the United Kingdom, the incidence rate is only 1 : 100 000 men per year with a lifetime risk of developing a TGCT of 1 in 400 and 1900 new cases per year (Horwich, 2002). There has, however, been a steady increase in the incidence of TGCTs in European countries in the last two decades (Bergstrom et al, 1996). The reasons for this increasing incidence and the aetiology of TGCTs remain unknown. The European Germ Cell Cancer Consensus Group has provided clear guidelines for the primary treatment of both seminoma tumour and NSGCT (Schmoll et al, 2004). There is, however, a lack of clear consensus on how to follow patients after primary treatment, and a number of issues dictate that follow-up should be carefully thought out and rigorously adhered to. Here, we discuss these factors as they pertain to male germ cell tumour (GCT) practice and describe our recently developed protocols.
Rational for follow-up
Detecting relapse
In general, detecting relapse is the major reason for maintaining follow-up and is the main focus of this review. The management of testicular cancer has been a major oncological success story, and provides a model for the management of curative solid tumours (Horwich et al, 2006). The use of platinum-based chemotherapy schedules has resulted in high cure rates for all stages of the disease (International Germ Cell Cancer Collaborative Group, 1997). The fact that the majority of young men treated for testicular cancer have a durable response to primary treatment has resulted in the accumulation of significant data on both the patterns of relapse and the late effects of treatment. Lifelong cure rates are high but there remains a tangible risk of relapse. These relapses may be salvageable with a combination of further chemotherapy and surgery; recent studies suggest that around 50% of patients who relapse after primary treatment will be cured, depending on the pattern of relapse and the stage at detection (Fossa et al, 1999b; Huddart and Birtle, 2005). It is also recognised that late relapses (occurring greater than 2 years after complete remission) have a greater propensity for chemoresistance and confer a worse prognosis (Shahidi et al, 2002; Ronnen et al, 2005). The fact that relapses are discernable through the use of serum tumour markers and/or radiological imaging confers a responsibility for their prompt detection. However, false-negative computerised tomography (CT) examinations can occur owing to the inability of this modality to detect foci of disease in normal-sized nodes or to differentiate benign and malignant enlargement. It has been shown that by using 10–15 mm as the upper limit of normal, up to 44% of scans were false negative (Thomas et al, 1981; Richie et al, 1982; Rowland et al, 1982). For practical purposes then, a cutoff of 10 mm is used treating those measuring between 8 and 10 mm as suspicious. These measurements should be taken in the overall context of the patient (risk of disease, markers and tumour laterality) (Dalal et al, 2006). Tumour markers (βHCG and/or AFP) are elevated at relapse in about 2/3 of NSGCT and approximately 1/3 of seminomas. While LDH is vital in prognostication of metastatic disease and thus should be routinely included, its use in detecting relapse is questionable (Ackers and Rustin, 2006; Venkitaraman et al, 2007). Although markers may act as useful flags for relapse, they do not remove the need for clinical and imaging assessment in view of the rate of marker-negative relapse.
Detection of second primary cancer
A separate issue is that of metachronous, contralateral primary testicular tumours. Although a number of studies have reported an increased incidence, in the absence of specific risk factors (testicular maldescent, infertility, atrophy, young age at first presentation and microlithiasis; Harland et al, 1998; Holm et al, 2003) this risk is still low with a 15-year cumulative incidence of just 1.9% (Fossa et al, 2005). Apart from being encouraged to perform routine self-examination, we would not, therefore, routinely perform contralateral biopsies as part of our follow-up. The major risk factor for second primary cancer is thought to be testicular atrophy (Harland et al, 1998). Thus, in patients with a testicular volume of <12 ml, we would discuss the role of testicular biopsy to detect carcinoma in situ (before or at least 2 years post chemotherapy). If detected, carcinoma in situ is managed appropriately (Hoei-Hansen et al, 2004).
Late effects: physical
A third potential reason for undertaking follow-up is to assess, monitor and manage late toxicity of treatment. In addition to the well-recognised acute side effects of chemotherapy the significance of late side effects have become increasingly appreciated. Long-term survivors of testicular cancer may display an increased risk of cardiovascular disease (Huddart et al, 2003; Huddart and Birtle, 2005; van den Belt-Dusebout et al, 2006) and second malignancy (Travis et al, 2005; Raghavan et al, 2006). Other problems identified include long-term sensory neuropathy, Raynaud's phenomenon (Fossa, 2004) and effects on fertility (Brydoy et al, 2005; Huddart et al, 2005). Development of ‘metabolic syndrome’ and other long-term endocrine disturbance is also recognised (Nuver et al, 2005; Horwich et al, 2006). To date, detection and management of toxicity have been a minor component of most oncologists practice, and, in the main, this aspect has, by default, been delegated to primary care. Raghavan has made some recommendations but the evidence base for making recommendations in this area is limited. Detailed discussion of these issues is beyond the scope of this review, although we have made some rudimentary suggestions for late effect monitoring.
Late effects: psychological
A proportion of testicular cancer patients are psychologically vulnerable and find the diagnosis of testicular cancer traumatic. Subsequent treatment may significantly affect sexual function, cause anxiety, disrupt ability to work and reduce overall quality of life (Fleer et al, 2006; Dahl et al, 2007; Tuinman et al, 2007). Follow-up can help support such patients and help to rehabilitate so that they return to normal life.
Research
Research is rarely the major goal of follow-up, but the long-term follow-up of patients and collection of data within prospective trials and cohort-based databases have undoubtedly contributed significantly to understanding testicular cancer and treatment outcomes.
Risks of radiological intervention
Repeated use of imaging techniques that utilise ionising radiation (specifically chest radiographs and CT scanning of the thorax, abdomen and pelvis) is associated with a measurable risk of causing second malignancies. These risks must be outweighed by demonstrable benefit to patients (Hoffman et al, 1989; Boice et al, 1991; Brenner, 2004; Ronckers et al, 2005). Thoracic CT requires a radiation dose equivalent to 400 chest radiographs (8 vs 0.02 mSv), increasing the exposure to 20 mSv if the abdomen is included. It has been suggested that this results in a 1 : 1000 lifetime risk of second cancer/leukaemia over the subsequent 40 years (Dalal et al, 2006). A chest X-ray is a low-cost low-risk procedure, which is likely to pick up nodules of 1 cm or greater in the lungs, pleurally based lesions or mediastinal masses (Dalal et al, 2006).
General principles
Throughout these recommendations, we have considered the following data on imaging. The chest can be imaged both by chest X-ray and CT of the chest but thoracic relapse in nonseminomatous (NS) will for the most part be marker positive, and the great majority of GCTs that relapse will have significant disease burden outside the chest (Gietema et al, 2002; Oldenburg et al, 2006; Martin et al, 2007). Computerised tomography chest may pick up small marker-negative lesions not visible on chest X-ray, but unless the detection of such small lesions is likely to have prognostic significance, we omit chest CT from our follow-up schedules due to the significant additional radiation exposure. Although one study suggests no additional benefit to using chest X-ray, we feel that if CT of the chest is omitted it is worth performing a chest X-ray (Gietema et al, 2002). While pelvic CT forms an integral part of initial staging, there is minimal value in routinely scanning the pelvis as part of the follow-up. While there is no firm evidence base, there is a perceived increased risk of pelvic lymph node disease following scrotal interference, and, for this reason, we include a pelvic CT in this setting (White et al, 1997).
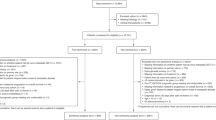
For each clinical scenario, we have reviewed the frequency and time to relapse both from the published literature and our own experience, and defined the frequency and nature of the follow-up according to principles previously outlined (Appendix A). We have graded the evidence and recommendations according to the guidelines set out by the American Society of Clinical Oncology (Appendix B) and these are given in square brackets. Recommendations without grading were based on the extensive clinical experience of clinicians from the Royal Marsden Hospital.
Seminoma
Stage I
Approximately, 75% of men who are diagnosed with seminoma have stage I disease, for which management options following orchidectomy consist of surveillance or adjuvant treatment in the form of either radiotherapy or, more recently, a single cycle of carboplatin chemotherapy (Oliver et al, 2005). The disease-specific survival for stage I disease approaches 99% independent of the management strategy used (Oldenburg et al, 2006).
Seminoma stage I surveillance
Eighty per cent of patients with stage I seminoma will be cured with orchidectomy alone, suggesting that only 20% of patients might benefit from adjuvant treatment. The identification of tumour size greater than 4 cm and rete-testis invasion as prognostic factors, has allowed further risk stratification of this group of patients. If neither risk factor is present, then the risk of relapse is less than 12%, this increases to 15% if one factor is present and over 30% if both are present (Warde et al, 2002). We consider patients with none or one risk factor as ideal candidates for surveillance, and, in those with both risk factors, we feel that there is a stronger argument for adjuvant treatment. However, as patients who relapse on surveillance are routinely cured with subsequent treatment, surveillance can be considered as an option for all patients with stage I disease. The overall crude relapse rate for patients managed with surveillance is 15.2–19.3% (Chung et al, 2002; Warde et al, 2002; Choo et al, 2005; Oldenburg et al, 2006). Most relapses occur in the first 2 years with a >5% annual hazard rate (AHR); relapses after 2 years are rare but are reported to occur up to 6 years after initial diagnosis (Warde et al, 2002; Oldenburg et al, 2006). The majority of relapses are in the para-aortic nodes, followed by mediastinal, supraclavicular nodes and lung metastasis (Dieckmann et al, 2005; Oldenburg et al, 2006). Note that only 30% of seminoma relapses will be marker positive. No studies have addressed the optimal scanning or follow-up frequency with widely differing policies reported (Huddart and Joffe, 2006). We suggest 3 monthly clinic visits and markers with 6 monthly CT scans of the abdomen and a chest X-ray for the first 2 years, based on need for regular cross-sectional imaging in the highest risk period [III, B]. The pelvis should only be scanned if there has been scrotal interference or previous pelvic surgery [III, B]. Follow-up should reduce to 4 monthly in year 3 and then 6 monthly until year 5. Computerised tomography scans and chest X-rays are performed annually until year 5 [III, B]. Annual follow-up with clinical examination and markers should continue for a further 5 years prior to discharge [III, B].
Seminoma stage I adjuvant radiotherapy follow-up
Historically, adjuvant treatment has taken the form of radiotherapy resulting in cure rates of 97–100%. Following two MRC trials investigating field and dose (Fossa et al, 1999a; Jones et al, 2005), the current European recommended schedule for adjuvant radiotherapy is 20 Gy in 10 fractions to the para-aortic nodes. Relapses in the treatment field are extremely uncommon; however, when the pelvic field is omitted, there is a small but statistically higher rate of pelvic relapse (Fossa et al, 1999a). In a combined review of 1535 patients treated with para-aortic radiotherapy, the relapse rate at 5 years was 3.6%, with 0.3% of relapses occurring in the abdomen (Martin et al, 2007). Most relapses occur in the first 2 years. The annual hazard ratio from the largest reported series for relapse between 2 to 6 years is 0.25–1% (Martin et al, 2007). For patients treated with para-aortic radiotherapy, we suggest 3 monthly clinical examination and markers for the first year and 4 monthly for the second year, and then 6 monthly until 5 years [III, B]. Computerised tomography scans of the pelvis only (unless a clinical reason exists to scan abdomen) performed annually for the first 2 years and then at 5 years prior to discharge [IV, C]. The value of pelvic CT is unclear. One publication on omitting pelvic CT reported satisfactory overall outcomes, but a number of patients presented with large symptomatic pelvic masses (Livsey et al, 2001). A chest X-ray should be performed at 3 and 6 months and then annually until discharge. The extremely low risk of relapse after 5 years (approaching 0%), makes follow-up beyond 5 years unnecessary (Shahidi et al, 2002) [III, B].
Seminoma stage I follow-up after single-agent carboplatin
An alternative adjuvant treatment to radiotherapy is a single cycle of carboplatin chemotherapy. The use of a single cycle of carboplatin has been investigated by a number of groups (Dieckmann et al, 2000; Oliver et al, 2005). Most notably, Oliver et al reported a randomised trial of 1477 patients demonstrating no inferiority of a single cycle of carboplatin as compared with para-aortic radiotherapy with respect to disease-free and overall survival. The trial has only reported 4-year follow-up data and although there are limited data on risk of late relapse and on long-term toxicity, in many UK centres the use of carboplatin for stage I seminoma now exceeds the use of radiotherapy. Five-year relapse rates for a single cycle of carboplatin are 6.1% with more than 80% of relapses occurring in the abdomen (Martin et al, 2007) (in contrast to patients treated with para-aortic radiotherapy where abdominal relapses are extremely uncommon). We, therefore, recommend CT scan of the abdomen and a chest X-ray yearly, for the first 2 years and again at 5 years; the pelvis should only be scanned if there has been scrotal interference or previous pelvic surgery [III, B]. Patients should have a clinical examination and markers at 1 month after chemotherapy, and then 3 monthly for the first year, 4 monthly for the second year and then 6 monthly until year 5. Data on late relapses in the carboplatin-treated patients are not yet available, and, for this reason, it is recommended that these patients should also be followed for 10 years.
Stages IIa/b
Stage IIa seminoma includes patients with para-aortic lymph nodes up to 2 cm in size. Stage IIb disease includes those with nodes 2–5 cm. There is considerable variability on how stage IIa/b seminomas are treated. The treatment options for stage IIa/b seminomas include, para-aortic and iliac node radiotherapy (Schmidberger et al, 1997; Warde et al, 1998; Classen et al, 2003; Chung et al, 2004), three cycles of BEP (bleomycin, etoposide and cisplatin) or four cycles of EP (etoposide and cisplatin) chemotherapy or a combination of carboplatin chemotherapy and para-aortic radiotherapy (Warde et al, 1998; Arranz Arija et al, 2001; Patterson et al, 2001). All three of the above options provide high rates of cure, but with differing toxicity profiles. Patients treated with chemotherapy alone should be followed according to Stage IIc–IV Guidelines, but we present our protocol for follow-up post-combination carboplatin radiotherapy.
Stage IIa/b (post chemoradiotherapy) follow-up
Data obtained from the trials of a single cycle of carboplatin in stage I seminoma suggest that this treatment is sufficient to eradicate microscopic disease in the great majority of patients. We know that radiotherapy is highly effective in eradicating disease with up to 5 cm in size in the para-aortic nodes (Classen et al, 2003; Chung et al, 2004). Our current protocol for treating patients with stage IIa/b disease, is to give one cycle of carboplatin (AUC 7) followed 4 weeks later by para-aortic radiotherapy to a dose of 30 Gy in 15 fractions based on 5-year relapse-free survival probability of 96.9% (Patterson et al, 2001) achieved at our institution. We suggest 3-monthly clinic examinations and markers for the first year, 4 monthly for the second year, 6 monthly until year 5 and then annual review. Computerised tomography scan of the pelvis and chest X-ray should be done at 3 months and again at 1, 2 and 5 years [III, B]. The follow-up schedule is specific to this protocol.
Stages IIc–IV
There is general agreement that best treatment for stage IIc–IV seminomas involves multiagent platinum-containing chemotherapy (usually BEP). There is evidence from a large prospective randomised trial that three cycles of BEP is equivalent to four cycles for good prognosis GCTs (de Wit et al, 2001).
Seminoma stage IIc+ follow-up
With large volume seminoma, it is not uncommon for there to be a residual mass following chemotherapy. In most cases, this represents fibrotic scar tissue. Attempted surgical removal can be difficult. In most cases, the masses will resolve in time, but if larger than 3 cm the chance of active malignancy is higher (Puc et al, 1996). If PET scanning is available, then data from De Santis et al (2004) suggests that 80% of patients with active disease can be identified and should be undertaken for masses >3 cm. Following PET, we suggest performing CT scans at regular intervals (6 monthly to annually) until complete response or a stable calcified mass is the only residuum. When this is achieved, the low rate of relapse makes further scanning unnecessary [III, B]. The follow-up schedule for advanced seminoma is the same as for NSGCT, but patients can be discharged after 5 years if free of relapse (Shahidi et al, 2002).
Nonseminoma
Stage I
The options for men with stage I NSGCTs (post orchidectomy) are close surveillance or adjuvant chemotherapy (in the form of two cycles of BEP chemotherapy). Adjuvant primary retroperitoneal lymph node dissection (RPLND) is rarely performed within the United Kingdom, but we present a discussion of the pertinent issues.
NS stage I surveillance
Retrospective series identified the histological presence of vascular invasion as the strongest predictor of relapse in stage I NSGCTs (Freedman et al, 1987; Vergouwe et al, 2003). Surveillance as a strategy for the management of stage I tumours was prospectively studied by the Medical Research Council and their results were published in 1992 (Read et al, 1992). In the absence of high-risk features where relapse rates approach 50%, among the usual population undergoing surveillance a relapse rate of around 20% is to be expected. Surveillance protocols should, therefore, be directed at promptly detecting these relapses, as with treatment at this stage disease-free survival rates of 98% should be achieved.
It is clear from a number of series that the vast majority of relapses will occur within 2 years, most in the first year of surveillance. In the original prospective study, 80% (of 100 relapses) occurred within the first year (54 of these in the first 6 months) and 92% by 2 years (Read et al, 1992). A number of subsequent studies have demonstrated similar results and are summarised in Table 1. A series of 478 patients (stage I NSGCT) undergoing surveillance at the Royal Marsden Hospitals (Royal Marsden, unpublished data) with a relapse rate of 24% showed almost identical results with 80% of relapses occurring within 1 year, 90% within 2 years, 94% by 3 years and 97% by 4 years. The subsequent relapses occurred at 6 years (one patient) and 7 years (two patients).
The site and subsequent detection of relapse was assessed in our Royal Marsden series. 72/111 (67%) were marker positive and in 58 (51%) this was the flag. In 15 (14%) this was the only detectable abnormality. Sixty-two patients (56%) had evidence of retroperitoneal adenopathy, and in 55 (50%) this was the only anatomical site of relapse. Of these, 18 (16%) were marker negative, making cross-sectional abdominal imaging mandatory in surveillance protocols. Thoracic relapse rates of around 20% can be expected but methods of detection remain controversial, predominantly as drawing conclusions from small series is unreliable. From a series of 168 patients, 8/42 relapses (19%) occurred within the chest (Harvey et al, 2002), although 7 had other indicators of relapse (raised markers and abnormal abdominopelvic CT scans) and all 8 had abnormal chest radiographs, and the authors concluded that there is no requirement for thoracic CT. Some may go further – of 170 patients undergoing surveillance for stage I NS, all recurrences were detected with clinical history and examination, markers and abdominopelvic CT, and it was felt that the omission of chest radiographs would not have altered the outcome (Sharir et al, 1999). However, of the 111 Royal Marsden patients who experienced relapse, there were 8 (7%) in whom CT scans of the thorax, performed on the surveillance protocol, were the only detector of relapse.
Our suggested protocols then focus on the first year with investigations reducing in intensity in subsequent years. The patients have markers checked monthly for the first year, with 2-monthly chest X-rays and clinical examination [III, B] and CT scans (abdomen only unless pelvis deemed high risk) at 3 months and 1 year [I, A]. This is broadly similar to the recent NCCN Guidelines, although reduces the frequency of CT, as supported by data from the recently presented MRC TE08 trial, where a two-scan strategy was no less effective than performing five scans (Kondagunta et al, 2003; Rustin et al, 2007). From the above data, it is clear that relapse after 5 years is so infrequent as to merit discharge at this point. Given the increasing awareness of long-term side effects, we also advocate assessing cardiovascular risk factors in these untreated control patients at 2 and 5 years [III, B].
NS stage I post-adjuvant chemotherapy follow-up
Patients in whom the rate of relapse is expected to approach 50% (ie, possessing high-risk features, predominately vascular invasion) are also candidates for surveillance as treatment at relapse confers identical long-term survival outcomes, but may also be offered adjuvant chemotherapy, most commonly in the form of two cycles of BEP. This has been shown to reduce the rate of relapse to <5% (Cullen et al, 1996). The proven GCT relapses seen in this trial occurred after 7 months and were detected by raised markers, and a published review including 148 patients treated with adjuvant chemotherapy demonstrated six (4%) relapses, all within 2 years of treatment (Oliver et al, 2004).
Reflecting both this much reduced rate of relapse and the conserved tendency to early presentation of recurrence, our protocol reduces the frequency of investigation and follow-up visit at an earlier stage than the previously described for surveillance [III, B]. We suggest one scan of abdomen be performed at 6 months as occasionally a microscopically involved lymph node may increase in size due to the presence of teratoma differentiated [V, D]. As treatment has been administered, assessment of late effects is increasingly important, our protocols assess this at 2 and 5 years post treatment [III, B], but lifelong awareness of the risk of treatment-related effects is important.
NS stage I post-adjuvant retroperitoneal lymph node dissection follow-up
Adjuvant RPLND allows more accurate histopathological staging of patients with around 30% of patients deemed stage I by conventional radiological and marker evaluation having pathological evidence of nodal metastases (ie, stage II) at surgery. Such patients are typically offered ‘adjuvant’ chemotherapy in the form of two cycles of BEP with subsequent recurrences uncommon indeed (Donohue et al, 1993; Spermon et al, 2002; Albers et al, 2003). Patients without evidence of nodal metastases demonstrate relapse rates between 10 and 13%, the vast majority of which are pulmonary in nature and occur within the first year.
We would advocate following up patients treated with RPLND and two cycles of BEP (ie, node positive) as post-adjuvant chemotherapy (above). Around 30% node-positive patients not receiving further treatment relapse (Donohue et al, 1993) and as such should be followed up along the NS stage I surveillance protocol, as should node-negative patients, although abdominal relapse post-RPLND should be uncommon.
Stage II–IV NSGCT
Germ cell tumours are one of the rare instances where the majority of patients with disseminated disease can be cured, predominately with combination chemotherapy, although often requiring surgery (and less frequently radiotherapy) to eradicate residual disease. Overall, around 80% should achieve complete clinical +/− radiological response to treatment (depending upon IGCCCG prognostic factors) (Mead et al, 1992; Sonneveld et al, 2001; Horwich et al, 2006). Radiological assessment of response continues until residual disease has either been surgically resected or completely resolved, with a CT scan performed at this point as a baseline for follow-up.
Disseminated disease (NS/seminoma), post-curative treatment follow-up
Once curative treatment (CR) has been achieved and treatment completed, relapse rates of up to 10% might be expected. The majority of these will occur within the first year, although a late relapse rate (that occurring >2 years post completion of treatment) of around 3% is observed (Gietema et al, 2002; Ronnen et al, 2005). Of 353 patients treated in the Netherlands between 1977 and 1999, 290 (82%) achieved CR following cisplatin-based chemotherapy and surgery as required. Thirty-three of these (11%) subsequently relapsed, with a median time to relapse of 17 months (range: 6–179). In 27 (81%) of these, elevated markers ‘flagged’ the relapse, and a further 4 markers corresponded to recurrence found at physical examination. Two patients with brain metastasis presented with neurological symptoms. In no patients did the chest radiograph assist with detection of recurrence, and the authors point out that following ESMO Guidelines would have resulted in over 6000 X-rays in total for this period (Gietema et al, 1992).
Specifically regarding late recurrences (Ronnen et al, 2005), 17/551 patients relapsed after at least 2 years post chemotherapy, with a median time to relapse of 7.8 years (range: 2.7–18.7) and 9/17 presenting with clinical symptoms of recurrence. In all, 3 out of the 17 presented with raised markers (although a further 9 subsequently demonstrated raised markers), and, in this series, two relapses were detected by abnormal chest X-ray. From a retrospective review of 1263 patients with TGCT treated at the Royal Marsden Hospital (513 with metastatic NSGCT), 53 had recurrences after 2 years, 14 of which occurred later than 5 years (9/14 detected at routine annual follow-up and 5 presenting with interval symptoms). Twelve of these very late recurrences were in patients treated for metastatic NS (giving an annual risk of recurrence in these patients of 1% between 5 and 10 years) (Shahidi et al, 2002).
Our protocols therefore utilise less imaging, although in the absence of randomised data we continue to recommend 4-monthly chest X-rays for the first 2 years, but annually after that [III, B]. Markers are checked 2 monthly for the first year, 4 monthly for the second and 6 monthly after that [III, B] for up to 5 years. The continued risk of late relapse in NS patients means that we recommend continuing to follow up these patients annually from 5 to 10 years and every 2 years subsequently [V, D]. Late relapse is rare (Shahidi et al, 2002) in metastatic seminoma so would routinely discharge seminoma patients at 5 years [III, B].
Assessing late toxicity
Although a thorough discussion regarding long-term side effects of treatment is beyond the scope of this article, a growing body of data demonstrates that survivors of TGCTs are at increased risk of hypogonadism, and a metabolic syndrome including obesity, hypertension, diabetes and hypercholesterolaemia (Vaughn et al, 2002). We, therefore, include in our protocols assessing patients for these features patients at 2, 5 and 10 years. We would assess BP, glucose, fasting cholesterol, LH and testosterone at these time points. Patients should be advised not to smoke and to be counselled regarding weight gain. A history of cardiac disease or other health problems should be sought particularly beyond 5 years of follow-up. It is not known if other screening tests for coronary artery disease or for secondary cancer would be advantageous, but patients should be encouraged to avail themselves of any relevant national screening programmes such as the one being developed for colorectal cancer.
Conclusions
Managing patients with TGCTs is a complex business requiring multidisciplinary teamwork and multiple clinical scenarios. While evidence for best practice in terms of treatment is widely available and continuously evolving, the important issues regarding follow-up schedule are for the most part left to individual preference. The standardising of follow-up would result in optimising risk/benefit ratios for individual patients, while ensuring economic use of resources. Furthermore, this should enable future trials to address specific issues around follow-up giving meaningful and useful results.
These guidelines have been adopted by the South East England Testicular Cancer supraregional network.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
International Germ Cell Cancer Collaborative Group (1997) International Germ Cell Consensus Classification: a prognostic factor-based staging system for metastatic germ cell cancers. International Germ Cell Cancer Collaborative Group. J Clin Oncol 15: 594–603
Ackers C, Rustin GJ (2006) Lactate dehydrogenase is not a useful marker for relapse in patients on surveillance for stage I germ cell tumours. Br J Cancer 94: 1231–1232
Albers P, Melchior D, Muller SC (2003) Surgery in metastatic testicular cancer. Eur Urol 44: 233–244
Arranz Arija JA, Garcia del Muro X, Guma J, Aparicio J, Salazar R, Saenz A, Carles J, Sanchez M, Germa-Lluch JR (2001) E400P in advanced seminoma of good prognosis according to the International Germ Cell Cancer Collaborative Group (IGCCCG) classification: the Spanish Germ Cell Cancer Group experience. Ann Oncol 12: 487–491
Atsu N, Eskicorapci S, Uner A, Ekici S, Gungen Y, Erkan I, Uygur MC, Ozen H (2003) A novel surveillance protocol for stage I nonseminomatous germ cell testicular tumours. BJU Int 92: 32–35
Bergstrom R, Adami HO, Mohner M, Zatonski W, Storm H, Ekbom A, Tretli S, Teppo L, Akre O, Hakulinen T (1996) Increase in testicular cancer incidence in six European countries: a birth cohort phenomenon. J Natl Cancer Inst 88: 727–733
Boice Jr JD, Preston D, Davis FG, Monson RR (1991) Frequent chest X-ray fluoroscopy and breast cancer incidence among tuberculosis patients in Massachusetts. Radiat Res 125: 214–222
Brenner DJ (2004) Radiation risks potentially associated with low-dose CT screening of adult smokers for lung cancer. Radiology 231: 440–445
Brydoy M, Fossa SD, Klepp O, Bremnes RM, Wist EA, Wentzel-Larsen T, Dahl O (2005) Paternity following treatment for testicular cancer. J Natl Cancer Inst 97: 1580–1588
Choo R, Thomas G, Woo T, Lee D, Kong B, Iscoe N, Danjoux C, Klotz L, Morton G, Chander S (2005) Long-term outcome of postorchiectomy surveillance for Stage I testicular seminoma. Int J Radiat Oncol Biol Phys 61: 736–740
Chung P, Parker C, Panzarella T, Gospodarowicz MK, Jewett S, Milosevic MF, Catton CN, Bayley AJ, Tew-George B, Moore M, Sturgeon JF, Warde P (2002) Surveillance in stage I testicular seminoma – risk of late relapse. Can J Urol 9: 1637–1640
Chung PW, Gospodarowicz MK, Panzarella T, Jewett MA, Sturgeon JF, Tew-George B, Bayley AJ, Catton CN, Milosevic MF, Moore M, Warde PR (2004) Stage II testicular seminoma: patterns of recurrence and outcome of treatment. Eur Urol 45: 754–759; discussion 759–760
Classen J, Schmidberger H, Meisner C, Souchon R, Sautter-Bihl ML, Sauer R, Weinknecht S, Kohrmann KU, Bamberg M (2003) Radiotherapy for stages IIA/B testicular seminoma: final report of a prospective multicenter clinical trial. J Clin Oncol 21: 1101–1106
Cullen MH, Stenning SP, Parkinson MC, Fossa SD, Kaye SB, Horwich AH, Harland SJ, Williams MV, Jakes R (1996) Short-course adjuvant chemotherapy in high-risk stage I nonseminomatous germ cell tumors of the testis: a Medical Research Council report. J Clin Oncol 14: 1106–1113
Dahl AA, Bremnes R, Dahl O, Klepp O, Wist E, Fossa SD (2007) Is the sexual function compromised in long-term testicular cancer survivors? Eur Urol 52: 1438–1447
Dalal PU, Sohaib SA, Huddart R (2006) Imaging of testicular germ cell tumours. Cancer Imaging 6: 124–134
Daugaard G, Petersen PM, Rorth M (2003) Surveillance in stage I testicular cancer. APMIS 111: 76–83; discussion 83–85
De Santis M, Becherer A, Bokemeyer C, Stoiber F, Oechsle K, Sellner F, Lang A, Kletter K, Dohmen BM, Dittrich C, Pont J (2004) 2-18fluoro-deoxy-D-glucose positron emission tomography is a reliable predictor for viable tumor in postchemotherapy seminoma: an update of the prospective multicentric SEMPET trial. J Clin Oncol 22: 1034–1039
de Wit R, Roberts JT, Wilkinson PM, de Mulder PH, Mead GM, Fossa SD, Cook P, de Prijck L, Stenning S, Collette L (2001) Equivalence of three or four cycles of bleomycin, etoposide, and cisplatin chemotherapy and of a 3- or 5-day schedule in good-prognosis germ cell cancer: a randomized study of the European Organization for Research and Treatment of Cancer Genitourinary Tract Cancer Cooperative Group and the Medical Research Council. J Clin Oncol 19: 1629–1640
Dieckmann KP, Albers P, Classen J, De Wit M, Pichlmeier U, Rick O, Mullerleile U, Kuczyk M (2005) Late relapse of testicular germ cell neoplasms: a descriptive analysis of 122 cases. J Urol 173: 824–829
Dieckmann KP, Bruggeboes B, Pichlmeier U, Kuster J, Mullerleile U, Bartels H (2000) Adjuvant treatment of clinical stage I seminoma: is a single course of carboplatin sufficient? Urology 55: 102–106
Divrik RT, Akdogan B, Ozen H, Zorlu F (2006) Outcomes of surveillance protocol of clinical stage I nonseminomatous germ cell tumors – is shift to risk adapted policy justified? J Urol 176: 1424–1429; discussion 1429–1430
Donohue JP, Thornhill JA, Foster RS, Rowland RG, Bihrle R (1993) Retroperitoneal lymphadenectomy for clinical stage A testis cancer (1965–1989): modifications of technique and impact on ejaculation. J Urol 149: 237–243
Fleer J, Hoekstra HJ, Sleijfer DT, Tuinman MA, Klip EC, Hoekstra-Weebers JE (2006) Quality of life of testicular cancer survivors and the relationship with sociodemographics, cancer-related variables, and life events. Support Care Cancer 14: 251–259
Fossa SD (2004) Long-term sequelae after cancer therapy – survivorship after treatment for testicular cancer. Acta Oncol 43: 134–141
Fossa SD, Chen J, Schonfeld SJ, McGlynn KA, McMaster ML, Gail MH, Travis LB (2005) Risk of contralateral testicular cancer: a population-based study of 29,515 U.S. men. J Natl Cancer Inst 97: 1056–1066
Fossa SD, Horwich A, Russell JM, Roberts JT, Cullen MH, Hodson NJ, Jones WG, Yosef H, Duchesne GM, Owen JR, Grosch EJ, Chetiyawardana AD, Reed NS, Widmer B, Stenning SP (1999a) Optimal planning target volume for stage I testicular seminoma: a Medical Research Council randomized trial. Medical Research Council Testicular Tumor Working Group. J Clin Oncol 17: 1146
Fossa SD, Stenning SP, Gerl A, Horwich A, Clark PI, Wilkinson PM, Jones WG, Williams MV, Oliver RT, Newlands ES, Mead GM, Cullen MH, Kaye SB, Rustin GJ, Cook PA (1999b) Prognostic factors in patients progressing after cisplatin-based chemotherapy for malignant non-seminomatous germ cell tumours. Br J Cancer 80: 1392–1399
Freedman LS, Parkinson MC, Jones WG, Oliver RT, Peckham MJ, Read G, Newlands ES, Williams CJ (1987) Histopathology in the prediction of relapse of patients with stage I testicular teratoma treated by orchidectomy alone. Lancet 2: 294–298
Gietema JA, Meinardi MT, Sleijfer DT, Hoekstra HJ, van der Graaf WT (2002) Routine chest X-rays have no additional value in the detection of relapse during routine follow-up of patients treated with chemotherapy for disseminated non-seminomatous testicular cancer. Ann Oncol 13: 1616–1620
Gietema JA, Sleijfer DT, Willemse PH, Schraffordt Koops H, van Ittersum E, Verschuren WM, Kromhout D, Sluiter WJ, Mulder NH, de Vries EG (1992) Long-term follow-up of cardiovascular risk factors in patients given chemotherapy for disseminated nonseminomatous testicular cancer. Ann Intern Med 116: 709–715
Harland SJ, Cook PA, Fossa SD, Horwich A, Mead GM, Parkinson MC, Roberts JT, Stenning SP (1998) Intratubular germ cell neoplasia of the contralateral testis in testicular cancer: defining a high risk group. J Urol 160: 1353–1357
Harvey ML, Geldart TR, Duell R, Mead GM, Tung K (2002) Routine computerised tomographic scans of the thorax in surveillance of stage I testicular non-seminomatous germ-cell cancer – a necessary risk? Ann Oncol 13: 237–242
Hoei-Hansen CE, Nielsen JE, Almstrup K, Hansen MA, Skakkebaek NE, Rajpert-DeMeyts E, Leffers H (2004) Identification of genes differentially expressed in testes containing carcinoma in situ. Mol Hum Reprod 10: 423–431
Hoffman DA, Lonstein JE, Morin MM, Visscher W, Harris III BS, Boice Jr JD (1989) Breast cancer in women with scoliosis exposed to multiple diagnostic x rays. J Natl Cancer Inst 81: 1307–1312
Holm M, Hoei-Hansen CE, Rajpert-De Meyts E, Skakkebaek NE (2003) Increased risk of carcinoma in situ in patients with testicular germ cell cancer with ultrasonic microlithiasis in the contralateral testicle. J Urol 170: 1163–1167
Horwich A (2002) Testicular Tumours, vol 2, Oxford Textbook of Oncology. Oxford University Press: Oxford
Horwich A, Shipley J, Huddart R (2006) Testicular germ-cell cancer. Lancet 367: 754–765
Huddart RA, Birtle AJ (2005) Recent advances in the treatment of testicular cancer. Expert Rev Anticancer Ther 5: 123–138
Huddart RA, Joffe JK (2006) Preferred treatment for stage I seminoma: a survey of Canadian radiation oncologists. Clin Oncol (R Coll Radiol) 18: 693–695
Huddart RA, Norman A, Moynihan C, Horwich A, Parker C, Nicholls E, Dearnaley DP (2005) Fertility, gonadal and sexual function in survivors of testicular cancer. Br J Cancer 93: 200–207
Huddart RA, Norman A, Shahidi M, Horwich A, Coward D, Nicholls J, Dearnaley DP (2003) Cardiovascular disease as a long-term complication of treatment for testicular cancer. J Clin Oncol 21: 1513–1523
Jones WG, Fossa SD, Mead GM, Roberts JT, Sokal M, Horwich A, Stenning SP (2005) Randomized trial of 30 versus 20 Gy in the adjuvant treatment of stage I testicular seminoma: a report on Medical Research Council Trial TE18, European Organisation for the Research and Treatment of Cancer Trial 30942 (ISRCTN18525328). J Clin Oncol 23: 1200–1208
Kondagunta GV, Sheinfeld J, Motzer RJ (2003) Recommendations of follow-up after treatment of germ cell tumors. Semin Oncol 30: 382–389
Livsey JE, Taylor B, Mobarek N, Cooper RA, Carrington B, Logue JP (2001) Patterns of relapse following radiotherapy for stage I seminoma of the testis: implications for follow-up. Clin Oncol (R Coll Radiol) 13: 296–300
Martin JM, Panzarella T, Zwahlen DR, Chung P, Warde P (2007) Evidence-based guidelines for following stage 1 seminoma. Cancer 109: 2248–2256
Mead GM, Stenning SP, Parkinson MC, Horwich A, Fossa SD, Wilkinson PM, Kaye SB, Newlands ES, Cook PA (1992) The Second Medical Research Council study of prognostic factors in nonseminomatous germ cell tumors. Medical Research Council Testicular Tumour Working Party. J Clin Oncol 10: 85–94
Nuver J, Smit AJ, Wolffenbuttel BH, Sluiter WJ, Hoekstra HJ, Sleijfer DT, Gietema JA (2005) The metabolic syndrome and disturbances in hormone levels in long-term survivors of disseminated testicular cancer. J Clin Oncol 23: 3718–3725
Oldenburg J, Martin JM, Fossa SD (2006) Late relapses of germ cell malignancies: incidence, management, and prognosis. J Clin Oncol 24: 5503–5511
Oliver RT, Mason MD, Mead GM, von der Maase H, Rustin GJ, Joffe JK, de Wit R, Aass N, Graham JD, Coleman R, Kirk SJ, Stenning SP (2005) Radiotherapy versus single-dose carboplatin in adjuvant treatment of stage I seminoma: a randomised trial. Lancet 366: 293–300
Oliver RT, Ong J, Shamash J, Ravi R, Nagund V, Harper P, Ostrowski MJ, Sizer B, Levay J, Robinson A, Neal DE, Williams M (2004) Long-term follow-up of Anglian Germ Cell Cancer Group surveillance versus patients with Stage 1 nonseminoma treated with adjuvant chemotherapy. Urology 63: 556–561
Patterson H, Norman AR, Mitra SS, Nicholls J, Fisher C, Dearnaley DP, Horwich A, Mason MD, Huddart RA (2001) Combination carboplatin and radiotherapy in the management of stage II testicular seminoma: comparison with radiotherapy treatment alone. Radiother Oncol 59: 5–11
Puc HS, Heelan R, Mazumdar M, Herr H, Scheinfeld J, Vlamis V, Bajorin DF, Bosl GJ, Mencel P, Motzer RJ (1996) Management of residual mass in advanced seminoma: results and recommendations from the Memorial Sloan–Kettering Cancer Center. J Clin Oncol 14: 454–460
Raghavan D (2006) Increased late toxicity in 12–20 year survivors of germ cell tumours. 2006 Proceedings of ASCO Abstract No.4509
Read G, Stenning SP, Cullen MH, Parkinson MC, Horwich A, Kaye SB, Cook PA (1992) Medical Research Council prospective study of surveillance for stage I testicular teratoma. Medical Research Council Testicular Tumors Working Party. J Clin Oncol 10: 1762–1768
Richie JP, Garnick MB, Finberg H (1982) Computerized tomography: how accurate for abdominal staging of testis tumors? J Urol 127: 715–717
Ronckers CM, Erdmann CA, Land CE (2005) Radiation and breast cancer: a review of current evidence. Breast Cancer Res 7: 21–32
Ronnen EA, Kondagunta GV, Bacik J, Marion S, Bajorin DF, Sheinfeld J, Bosl GJ, Motzer RJ (2005) Incidence of late-relapse germ cell tumor and outcome to salvage chemotherapy. J Clin Oncol 23: 6999–7004
Rowland RG, Weisman D, Williams SD, Einhorn LH, Klatte EC, Donohue JP (1982) Accuracy of preoperative staging in stages A and B nonseminomatous germ cell testis tumors. J Urol 127: 718–720
Rustin GJS, Mead GM, Stenning SP et al (2007) A randomised trial of 2 versus 5 CT scans in the surveillance of patients with stage 1 non-seminomatous germ cell tumours of the testis: Medical Research Council Trial TE08, ISRCTN56475197. J Clin Oncol 25 (11): 1310–1315
Schmidberger H, Bamberg M, Meisner C, Classen J, Winkler C, Hartmann M, Templin R, Wiegel T, Dornoff W, Ross D, Thiel HJ, Martini C, Haase W (1997) Radiotherapy in stage IIA and IIB testicular seminoma with reduced portals: a prospective multicenter study. Int J Radiat Oncol Biol Phys 39: 321–326
Schmoll HJ, Souchon R, Krege S, Albers P, Beyer J, Kollmannsberger C, Fossa SD, Skakkebaek NE, de Wit R, Fizazi K, Droz JP, Pizzocaro G, Daugaard G, de Mulder PH, Horwich A, Oliver T, Huddart R, Rosti G, Paz Ares L, Pont O, Hartmann JT, Aass N, Algaba F, Bamberg M, Bodrogi I, Bokemeyer C, Classen J, Clemm S, Culine S, de Wit M, Derigs HG, Dieckmann KP, Flasshove M, Garcia del Muro X, Gerl A, Germa-Lluch JR, Hartmann M, Heidenreich A, Hoeltl W, Joffe J, Jones W, Kaiser G, Klepp O, Kliesch S, Kisbenedek L, Koehrmann KU, Kuczyk M, Laguna MP, Leiva O, Loy V, Mason MD, Mead GM, Mueller RP, Nicolai N, Oosterhof GO, Pottek T, Rick O, Schmidberger H, Sedlmayer F, Siegert W, Studer U, Tjulandin S, von der Maase H, Walz P, Weinknecht S, Weissbach L, Winter E, Wittekind C (2004) European consensus on diagnosis and treatment of germ cell cancer: a report of the European Germ Cell Cancer Consensus Group (EGCCCG). Ann Oncol 15: 1377–1399
Shahidi M, Norman AR, Dearnaley DP, Nicholls J, Horwich A, Huddart RA (2002) Late recurrence in 1263 men with testicular germ cell tumors. Multivariate analysis of risk factors and implications for management. Cancer 95: 520–530
Sharir S, Jewett MA, Sturgeon JF, Moore M, Warde PR, Catton CN, Gospodarowicz MK (1999) Progression detection of stage I nonseminomatous testis cancer on surveillance: implications for the followup protocol. J Urol 161: 472–475; discussion 475–476
Sonneveld DJ, Hoekstra HJ, van der Graaf WT, Sluiter WJ, Mulder NH, Willemse PH, Koops HS, Sleijfer DT (2001) Improved long term survival of patients with metastatic nonseminomatous testicular germ cell carcinoma in relation to prognostic classification systems during the cisplatin era. Cancer 91: 1304–1315
Spermon JR, Roeleveld TA, van der Poel HG, Hulsbergen-van de Kaa CA, Ten Bokkel Huinink WW, van de Vijver M, Witjes JA, Horenblas S (2002) Comparison of surveillance and retroperitoneal lymph node dissection in Stage I nonseminomatous germ cell tumors. Urology 59: 923–929
Thomas JL, Bernardino ME, Bracken RB (1981) Staging of testicular carcinoma: comparison of CT and lymphangiography. AJR Am J Roentgenol 137: 991–996
Travis LB, Fossa SD, Schonfeld SJ, McMaster ML, Lynch CF, Storm H, Hall P, Holowaty E, Andersen A, Pukkala E, Andersson M, Kaijser M, Gospodarowicz M, Joensuu T, Cohen RJ, Boice Jr JD, Dores GM, Gilbert ES . (2005) Second Cancers among 40,576 Testicular Cancer Patients Focus on long term survivors. J Natl Cancer Inst 97 (18): 1354–1365
Tuinman MA, Hoekstra HJ, Sleijfer DT, Fleer J, Vidrine DJ, Gritz ER, Hoekstra-Weebers JE (2007) Testicular cancer: a longitudinal pilot study on stress response symptoms and quality of life in couples before and after chemotherapy. Support Care Cancer 15: 279–286
van den Belt-Dusebout AW, Nuver J, de Wit R, Gietema JA, ten Bokkel Huinink WW, Rodrigus PT, Schimmel EC, Aleman BM, van Leeuwen FE (2006) Long-term risk of cardiovascular disease in 5-year survivors of testicular cancer. J Clin Oncol 24: 467–475
Vaughn DJ, Gignac GA, Meadows AT (2002) Long-term medical care of testicular cancer survivors. Ann Intern Med 136: 463–470
Venkitaraman R, Johnson B, Huddart RA, Parker CC, Horwich A, Dearnaley DP (2007) The utility of lactate dehydrogenase in the follow-up of testicular germ cell tumours. BJU Int 100: 30–32
Vergouwe Y, Steyerberg EW, Eijkemans MJ, Albers P, Habbema JD (2003) Predictors of occult metastasis in clinical stage I nonseminoma: a systematic review. J Clin Oncol 21: 4092–4099
Warde P, Gospodarowicz M, Panzarella T, Catton C, Sturgeon J, Moore M, Jewett M (1998) Management of stage II seminoma. J Clin Oncol 16: 290–294
Warde P, Specht L, Horwich A, Oliver T, Panzarella T, Gospodarowicz M, von der Maase H (2002) Prognostic factors for relapse in stage I seminoma managed by surveillance: a pooled analysis. J Clin Oncol 20: 4448–4452
White PM, Howard GC, Best JJ, Wright AR (1997) The role of computed tomographic examination of the pelvis in the management of testicular germ cell tumours. Clin Radiol 52: 124–129
Acknowledgements
This work was undertaken in the Royal Marsden NHS Trust who received a proportion of its funding from the NHS Executive; the views expressed in this publication are those of the authors and not necessarily those of the NHS Executive. This work was supported by the Institute of Cancer Research, the Bob Champion Cancer Trust, the Cancer Research UK Section of Radiotherapy (CRUK) Grant number C46/A2131.
Author information
Authors and Affiliations
Corresponding author
Appendices
APPENDIX A







APPENDIX B
Levels of evidence and grading of recommendation
- Level :
-
Type of evidence
- I:
-
Evidence is obtained from meta-analysis of multiple, well-designed, controlled studies. Randomised trials with low false-positive and low false-negative errors (high power).
- II:
-
Evidence is obtained from at least one well-designed experimental study. Randomised trials with high false-positive and/or negative errors (low power).
- III:
-
Evidence is obtained from well-designed, quasi-experimental studies such as nonrandomised, controlled single-group, pre–post, cohort, time or matched case–control series.
- IV:
-
Evidence is from well-designed, nonexperimental studies such as comparative and correlational descriptive and case studies.
- V:
-
Evidence is from case reports and clinical examples.
- Grade :
-
Grading of recommendation
- A:
-
There is evidence of type I or consistent findings from multiple studies of types II, III or IV.
- B:
-
There is evidence of types II, III or IV and findings are generally consistent.
- C:
-
There is evidence of types II, III or IV but findings are inconsistent.
- D:
-
There is little or no systematic empirical evidence.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
van As, N., Gilbert, D., Money-Kyrle, J. et al. Evidence-based pragmatic guidelines for the follow-up of testicular cancer: optimising the detection of relapse. Br J Cancer 98, 1894–1902 (2008). https://doi.org/10.1038/sj.bjc.6604280
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6604280
This article is cited by
-
Nachsorge von Hodentumoren in der urologischen Praxis – historische Entwicklung und aktuelle Aspekte
Der Urologe (2022)
-
Can magnetic resonance imaging replace conventional computerized tomography for follow-up of patients with testicular cancer? A systematic review
World Journal of Urology (2022)
-
Nachsorge von Hodentumoren in der urologischen Praxis – historische Entwicklung und aktuelle Aspekte
best practice onkologie (2022)
-
Actual frequency of imaging during follow-up of testicular cancer in Israel—a comparison with the guidelines
European Radiology (2019)
-
Prostatic relapse of an undifferentiated teratoma 24 years after orchidectomy
BMC Research Notes (2015)