Abstract
Quality of colorectal cancer pathology reports is related to individual patient prognosis and future treatment options. This study sought to validate the prognostic utility of the Royal College of Pathologists minimum pathology dataset (MPD), regarded as the ‘gold standard’, within a population. Retrospective study of the survival of 5947 surgically resected colorectal cancer patients for whom an MPD had been collected. Variables were related to survival. The study population was representative of the Yorkshire colorectal cancer population. Survival was poorer in older patients and colonic tumours and improved over the study period. Local invasion, total number of lymph nodes retrieved, nodal stage, extramural vascular invasion, peritoneal involvement, distance of invasion beyond the muscularis propria, and in rectal cancers, circumferential resection margin involvement and distance to this margin were all validated as of prognostic significance within a population. Failure to report extramural vascular invasion, peritoneal involvement or circumferential resection margin status was associated with a worse survival than absence of the factor. All variables within the Royal College of Pathologists MPD are of prognostic significance. High-quality pathology reports are essential in providing accurate prognostic information and guiding optimal patient management.
Similar content being viewed by others
Main
High quality histopathological reporting is vital in the management of colorectal cancer. Assessment of the surgical specimen determines the stage of disease, the completeness of the surgical excision and, hence, the prognosis and future treatment options for the patient. It is crucial, therefore, that pathology reports contain all the accurate information required to fulfil these functions.
Many pathological features have been identified as being of prognostic value and therapeutic significance and, as a consequence, there are numerous guidelines stating which pathological features should be reported for colorectal cancer (Henson et al, 1994). In 1998 the Royal College of Pathologists synthesised, through the available literature and expert consensus, the features they deemed as being most important for determining the prognosis of colorectal cancer into a minimum pathology dataset (MPD) (Quirke and Williams, 1998). The document is a proforma detailing the minimum data items a pathologist should record when reporting colorectal cancer tumours. Much of the evidence through which it was formulated, however, originated from small single-centre studies or specialised trial environments and its validity has never been tested in a population-based setting.
The Northern and Yorkshire Cancer Registry (NYCRIS), in collaboration with Yorkshire's pathologists, first published a proforma for the pathological reporting of colorectal cancer resections in 1995 following a decision to standardise the collection of pathology data for registry use. The NYCRIS proforma was largely adopted by the Royal College of Pathologists as their MPD in 1998 and so the Northern and Yorkshire region is in the unique position of having access to identical data to that on this MPD from 1995. The NYCRIS proforma includes all MPD items and a few additional data points. NYCRIS also collects basic demographic and survival information about all patients diagnosed with cancer in the region. It is, therefore, possible to link the MPD to the survival data and, hence, assess the prognostic ability of the minimum dataset items. This study sought to determine the prognostic value of the contents of the Royal College of Pathologists MPD in a population of 3.6 million.
Materials and methods
All colorectal cancer patients for whom a MPD was completed, therefore having received a surgical resection of their tumour, and submitted to NYCRIS between 1995 and 2000 were identified. Routinely recorded information about these patients’ disease and its management were then downloaded from the main registry database and the two datasets merged. Any discrepancies were resolved by review of the original pathology report. Patients with multiple colorectal cancers were excluded. Cases without an MPD were also identified and their overall survival compared to exclude bias due to a failure to return forms.
The survival time for each patient was calculated from date of surgery to date of death from all causes or when censored (9 February 2006). Kaplan–Meier curves were created to compare univariate survival and log–rank tests were used to test for statistical significance. Cox-proportional hazards models were used to determine the impact of sex and age on the survival estimates for each prognostic factor.
Variables assessed were extent of local invasion, number of nodes retrieved, nodal stage, extramural vascular invasion (EMVI) and peritoneal involvement for all patients and circumferential margin involvement (CRM) and distance to the CRM for rectal tumours only. Distance of invasion beyond the muscularis propria was an additional item included on the Yorkshire form but omitted from the Royal College MPD and the prognostic significance of this variable was also investigated to support its inclusion in any future revision. Tumour grade was not investigated as poor correlation was found between colorectal cancer and main registry databases due to changes in the coding system over time, meaning accurate allocation to present groupings of well, moderate and poor differentiation was impossible.
Results
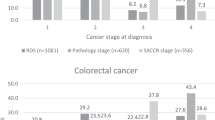
Between 1995 and 2000, 5947 colorectal pathology forms were submitted to NYCRIS. This represents 55.5% of the entire surgically managed colorectal cancer population in Yorkshire over that time period. There was no significant difference between the observed five-year survival of our study population (48.5%: 95% CI 47.2–49.8%) and the entire Yorkshire cohort of surgically treated colorectal cancer patients identified within the main cancer registry database (46.7%: 95% CI 45.8–47.6%).
The characteristics and five-year survival of our study population is presented in Table 1. There was a significant difference in survival observed across cancer sites, with colon cancers having a survival of 45.9% (95% CI 44.2–47.5%) and rectal cancers 53.4% (95% CI 51.0–55.7%). Survival was poorer in the older age groups and improved over the study period from 44.1% (95% CI 39.6–48.4%) in 1995 to 51.8% (95% CI 48.9–54.7%) in 2000.
Local invasion
Figure 1 shows the five-year survival curves of patients in each of the pathological T stages. Patients with T1 (74.6%: 95% CI 69.1–79.3%) and T2 tumours (70.7%: 95% CI 67.5–73.6%) had significantly better survival than those with T3 (50.6%: 95% CI 48.9–52.2%) or T4 tumours (25.1%: 95% CI 22.9–27.3%). Patients in whom the extent of local invasion was not recorded had an intermediate five-year survival of 58.3% (95% CI 43.2–70.8%). The effect remained after adjustment for patient age and gender (Table 2).
Total number of lymph nodes retrieved
Patients from whom greater than 12 nodes were retrieved had significantly higher survival (53.0%: 95% CI 50.7–55.2%) compared to those with the lowest nodal yield (45.4%: 95% CI 43.1–47.7%) (P<0.01). Patients in whom the number of nodes retrieved failed to be reported, had the worst survival (38.2%: 95% CI 27.8–48.7%). Age and gender did not influence the results (Table 2)
N stage
The greater the number of positive nodes identified the worse the survival of the patients (Figure 2). Those falling into the N2 category (i.e., four or more positive nodes identified) had the lowest five-year survival (22.2%: 95% CI 19.7–24.9%) compared to those with one to three (39.8%: 95% CI 37.4–42.2%) or those who were node negative (61.0%: 95% CI 59.3–62.7%). Those patients in whom the number of positive nodes was not reported had an intermediate five-year survival of 46.8% (95% CI 39.9–53.5%). The effects remained statistically significant after adjusting for age and gender (Table 2).
Extramural vascular invasion
Figure 3 shows the presence of EMVI was also prognostic. Patients in who vascular invasion was present had a poorer five-year survival (25.0%: 95% CI 22.4–27.6%) than those in whom it was absent (57.4%: 95% CI 55.7–59.2%). Again, those in whom the feature was not reported had an intermediate survival between the two reported groups of 46.8% (95% CI 44.4–49.1%) and adjustment for age and gender did not influence the results (Table 2).
Peritoneal involvement
A very similar effect, presented in Figure 4, was observed in relation to peritoneal involvement. Those possessing peritoneal involvement had a five-year survival of 24.3% (95% CI 21.9–26.8%) compared to 55.4% (95% CI 53.9–56.9%) in those in whom it was absent. Patients for whom the factor was not reported again had an intermediate survival between the two other groups (48.1%: 95% CI 44.3–51.8%). Again, there was no influence of patient age or gender on the results.
Tumour perforation
In pT4 tumours those with perforation through the tumour had a worse survival (26.4%: 95% CI 19.9–33.2%) than those with no perforation (32.3%: 95% CI 26.0–38.9%) although this did not reach statistical significance due to low reporting rates of just 25.8% of this factor in pT4 tumours. Adjustment for age and gender had no impact on the results (Table 2).
Distance of invasion beyond muscularis propria
Increasing distance of invasion beyond the muscularis propria in pT3 tumours was associated with decreasing survival (Figure 5) independently of the age and gender structure of the population (Table 2). Patients who had a distance of invasion of less than 1 mm had a five-year survival of 60.8% (95% CI 57.0–64.3%) compared to 36.9% (95% CI 30.5–43.4%) for those who had a depth of invasion greater than 15 mm. Patients in whom this feature was not reported had intermediate survival at 47.5% (95% CI 43.8–51.2%).
Circumferential resection margin involvement
The survival of rectal cancer patients with an involved CRM, as defined by the tumour lying less than one mm from the CRM, was significantly worse (26.9%: 95% CI 21.7–32.4%) than patients in whom this margin was clear (59.2%: 95% CI 56.4–61.9%)(P<0.01). Patients for whom this feature was not reported again had an intermediate survival of 52.7% (95% CI 46.2–58.9%). These data are presented in Figure 6. Age and gender had no effect on the trends seen (Table 2).
Distance to circumferential resection margin
Patients in whom the distance of the tumour from the circumferential resection margin was less than 1 mm had significantly poorer survival (33.3%: 95% CI 27.1–39.6%) than those in whom the distance was greater than a millimetre (P<0.01). Survival at 2 mm was 52.4% (95% CI 44.0–60.0%). There was no strong trend from improved survival when patients were grouped according to increasing millimetre increments of distance to the circumferential resection margin (Table 1).
Quality of reporting
As the total number of lymph nodes retrieved had been found to relate to survival the relationship of this factor to reporting rates of other factors was investigated (Table 3). Increasing total numbers of lymph nodes retrieved from 0 to 6 to over 12 was found to be positively correlated with detection of peritoneal involvement (P<0.01) and EMVI (P<0.01) in all cases and CRM involvement in rectal cases (P<0.01).
Discussion
This study provides the first evidence from a population-based setting to demonstrate that all the variables within the Royal College of Pathologists colorectal cancer minimum dataset have prognostic significance. Other variables currently not included within the minimum dataset, such as increasing distance of invasion beyond the muscularis propria in pT3 and pT4 tumours were also found to be related to decreasing survival.
Local invasion, lymph node status, peritoneal involvement and vascular invasion
The prognostic significance of local invasion, lymph node status and lymph node yields (Pocard et al, 1998; Wong et al, 1999; Tepper et al, 2001; Cserni et al, 2002; Goldstein, 2002; Johnson et al, 2002; Prandi et al, 2002; Joseph et al, 2003; Pheby et al, 2004; Baxter et al, 2005; Jestin et al, 2005; Sarli et al, 2005), peritoneal involvement, tumour perforation and vascular invasion (Talbot et al, 1980; Shepherd et al, 1989; Shepherd et al, 1995; Shepherd et al, 1997; Petersen et al, 2002) have all previously been documented. The results of this study confirm these findings in a large population-based setting.
Circumferential resection margins
The negative survival impact of CRM involvement has also been widely documented and our results support this previous work (Quirke et al, 1986; Adam et al, 1994; Birbeck et al, 2002; Wibe et al, 2002), but, the survival analyses looking at the distance to the circumferential resection margin in millimetre intervals indicated that there was a small and steady decrease in survival as this distance narrows. The most pronounced fall was at the one millimetre or less mark, with tumours lying between one and two millimetres from the CRM behaving similarly to those lying two to three millimetres away. This supports the work of Quirke et al (1986) and subsequent studies (Birbeck et al, 2002) but appears to contradict the more recent evidence and recommendations from the Dutch TME trial by Nagtegaal et al (2002).
Distance of invasion beyond the muscularis propria
This study also validates the prognostic significance of distance of invasion of tumour beyond the muscularis propria, supporting its inclusion in the revised sixth edition of TNM classification (American Joint Committee on Cancer, 2002). This data item is not currently included in the Royal College's minimum dataset but the results of our work indicate it should be included in any future revisions.
Quality of reporting
Patients in whom specific variables were not reported appear to have an intermediate survival between those who possessed the factor and those who did not. This suggests that absence of reporting does not necessarily mean absence of the factor. In addition, even where variables were definitely reported EMVI was only found in 17.8% of cases and peritoneal involvement in 19.5% of cases. Work from the CLASICC randomised controlled trial suggest that when reported by those with a specialist interest in gastro-intestinal pathology EMVI rates of 30% are seen. This is important as the presence of some of these pathological factors would influence an oncologist to offer adjuvant treatment. If an oncologist is not aware that a patient is potentially at risk then indicated treatment could be withheld with a concomitant increase in the risk of death. This emphasises the importance of comprehensive reporting of the minimum dataset. Previous work has highlighted problems of inadequate reporting (Bull et al, 1997) and our results demonstrate that failure to record key items is associated with poorer outcomes. The absence of a factor on a proforma does not equate with the prognosis of those in whom it was recorded as being absent, suggesting that in a proportion of patients it was indeed present. This was seen for EMVI, peritoneal and CRM involvement. Additionally poor rates of positive reporting of EMVI, peritoneal and CRM involvement are intimately linked to a lower number of nodes found within the NYCRIS data. Proforma reporting has been shown to improve the completeness of pathological reporting (Cross et al, 1998; Branston et al, 2002) but our results indicate significant amounts of key variables were still missing. We believe the use of computer proformas in which all data items had to be completed before a pathologist could finish a report and the careful auditing of pathology reporting against standards is essential. In addition, adequate time must be made available for pathologists to undertake thorough pathological examinations of all colorectal cancer specimens. This would improve the quality of pathological information, access of patients to adjuvant therapy and would be a good investment for cancer care.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Adam IJ, Mohamdee MO, Martin IG, Scott N, Finan PJ, Johnston D, Dixon MF, Quirke P (1994) Role of circumferential margin involvement in the local recurrence of rectal cancer. Lancet 344: 707–711
American Joint Committee on Cancer (2002) AJCC Cancer Staging Handbook: TNM Classification of Malignant Tumors. 6th edn, USA: Springer
Baxter NN, Virnig DJ, Rothenberger DA, Morris AM, Jessurun J, Virnig BA (2005) Lymph node evaluation in colorectal cancer patients: a population-based study. J Natl Cancer Inst 97: 219–225
Birbeck KF, Macklin CP, Tiffin NJ, Parsons W, Dixon MF, Mapstone NP, Abbott CR, Scott N, Finan PJ, Johnston D, Quirke P (2002) Rates of circumferential resection margin involvement vary between surgeons and predict outcomes in rectal cancer surgery. Ann Surg 235: 449–457
Branston LK, Greening S, Newcombe RG, Daoud R, Abraham JM, Wood F, Dallimore NS, Steward J, Rogers C, Williams GT (2002) The implementation of guidelines and computerised forms improves the completeness of cancer pathology reporting. The CROPS project: a randomised controlled trial in pathology. Eur J Cancer 38: 764–772
Bull AD, Biffin AH, Mella J, Radcliffe AG, Stamatakis JD, Steele RJ, Williams GT (1997) Colorectal cancer pathology reporting: a regional audit. J Clin Pathol 50: 138–142
Cross SS, Feeley KM, Angel CA (1998) The effect of four interventions on the informational content of histopathology reports of resected colorectal carcinomas. J Clin Pathol 51: 481–482
Cserni G, Vinh-Hung V, Burzykowski T (2002) Is there a minimum number of lymph nodes that should be histologically assessed for a reliable nodal staging of T3N0M0 colorectal carcinomas? J Surg Oncol 81: 63–69
Goldstein NS (2002) Lymph node recoveries from 2427 pT3 colorectal resection specimens spanning 45 years: recommendations for a minimum number of recovered lymph nodes based on predictive probabilities. Am J Surg Pathol 26: 179–189
Henson DE, Hutter RV, Sobin LH, Bowman HE (1994) Protocol for the examination of specimens removed from patients with colorectal carcinoma. a basis for checklists. Cancer committee, college of American pathologists. Task force for protocols on the examination of specimens from patients with colorectal cancer. Arch Pathol Lab Med 118: 122–125
Jestin P, Pahlman L, Glimelius B, Gunnarsson U (2005) Cancer staging and survival in colon cancer is dependent on the quality of the pathologists’ specimen examination. Eur J Cancer 41: 2071–2078
Johnson PM, Malatjalian D, Porter GA (2002) Adequacy of nodal harvest in colorectal cancer: a consecutive cohort study. J Gastrointest Surg 6: 883–888, discussion 889-890.
Joseph NE, Sigurdson ER, Hanlon AL, Wang H, Mayer RJ, MacDonald JS, Catalano PJ, Haller DG (2003) Accuracy of determining nodal negativity in colorectal cancer on the basis of the number of nodes retrieved on resection. Ann Surg Oncol 10: 213–218
Nagtegaal ID, Marijnen CA, Kranenbarg EK, van de Velde CJ, van Krieken JH (2002) Circumferential margin involvement is still an important predictor of local recurrence in rectal carcinoma: not one millimeter but two millimeters is the limit. Am J Surg Pathol 26: 350–357
Petersen VC, Baxter KJ, Love SB, Shepherd NA (2002) Identification of objective pathological prognostic determinants and models of prognosis in Dukes’ B colon cancer. Gut 51: 65–69
Pheby DF, Levine DF, Pitcher RW, Shepherd NA (2004) Lymph node harvests directly influence the staging of colorectal cancer: evidence from a regional audit. J Clin Pathol 57: 43–47
Pocard M, Panis Y, Malassagne B, Nemeth J, Hautefeuille P, Valleur P (1998) Assessing the effectiveness of mesorectal excision in rectal cancer: prognostic value of the number of lymph nodes found in resected specimens. Dis Colon Rectum 41: 839–845
Prandi M, Lionetto R, Bini A, Francioni G, Accarpio G, Anfossi A, Ballario E, Becchi G, Bonilauri S, Carobbi A, Cavaliere P, Garcea D, Giuliani L, Morziani E, Mosca F, Mussa A, Pasqualini M, Poddie D, Tonetti F, Zardo L, Rosso R (2002) Prognostic evaluation of stage B colon cancer patients is improved by an adequate lymphadenectomy: results of a secondary analysis of a large scale adjuvant trial. Ann Surg 235: 458–463
Quirke P, Durdey P, Dixon MF, Williams NS (1986) Local recurrence of rectal adenocarcinoma due to inadequate surgical resection. Histopathological study of lateral tumour spread and surgical excision. Lancet 2: 996–999
Quirke P, Williams GT (1998) Minimum Dataset for Colorectal Cancer Histopathology Reports. London: Royal College of Pathologists
Sarli L, Bader G, Iusco D, Salvemini C, Mauro DD, Mazzeo A, Regina G, Roncoroni L (2005) Number of lymph nodes examined and prognosis of TNM stage II colorectal cancer. Eur J Cancer 41: 272–279
Shepherd NA, Baxter KJ, Love SB (1995) Influence of local peritoneal involvement on pelvic recurrence and prognosis in rectal cancer. J Clin Pathol 48: 849–855
Shepherd NA, Baxter KJ, Love SB (1997) The prognostic importance of peritoneal involvement in colonic cancer: a prospective evaluation. Gastroenterology 112: 1096–1102
Shepherd NA, Saraga EP, Love SB, Jass JR (1989) Prognostic factors in colonic cancer. Histopathology 14: 613–620
Talbot IC, Ritchie S, Leighton MH, Hughes AO, Bussey HJ, Morson BC (1980) The clinical significance of invasion of veins by rectal cancer. Br J Surg 67: 439–442
Tepper JE, O’Connell MJ, Niedzwiecki D, Hollis D, Compton C, Benson III AB, Cummings B, Gunderson L, Macdonald JS, Mayer RJ (2001) Impact of number of nodes retrieved on outcome in patients with rectal cancer. J Clin Oncol 19: 157–163
Wibe A, Rendedal PR, Svensson E, Norstein J, Eide TJ, Myrvold HE, Soreide O (2002) Prognostic significance of the circumferential resection margin following total mesorectal excision for rectal cancer. Br J Surg 89: 327–334
Wong JH, Severino R, Honnebier MB, Tom P, Namiki TS (1999) Number of nodes examined and staging accuracy in colorectal carcinoma. J Clin Oncol 17: 2896–2900
Acknowledgements
We thank the Yorkshire pathologists for completing the proformas and making this study possible. Dr Maughan was supported by a grant from the National Translational Research Cancer programme. Dr Morris is supported by a grant via the Pelican Centre from the NHS colorectal cancer multidisciplinary team training programme. Professor Quirke is supported by a programme grant from Yorkshire Cancer Research.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Maughan, N., Morris, E., Forman, D. et al. The validity of the Royal College of Pathologists’ colorectal cancer minimum dataset within a population. Br J Cancer 97, 1393–1398 (2007). https://doi.org/10.1038/sj.bjc.6604036
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6604036
Keywords
This article is cited by
-
The prognostic value of MRI-detected extramural vascular invasion (mrEMVI) for rectal cancer patients treated with neoadjuvant therapy: a meta-analysis
European Radiology (2021)
-
Extramural venous invasion in rectal cancer: overview of imaging, histopathology, and clinical implications
Abdominal Radiology (2019)
-
The rationale behind complete mesocolic excision (CME) and a central vascular ligation for colon cancer in open and laparoscopic surgery
International Journal of Colorectal Disease (2014)
-
Marges d’exérèse et qualité de prise en charge des cancers du rectum
Oncologie (2010)