Abstract
The trimodality approach represented by concurrent chemoradiotherapy followed by surgical resection is a highly effective, but potentially toxic therapy for locally advanced non-small-cell lung cancer (NSCLC). In this review, we discuss the current status of this therapy in patients with mediastinal node-positive (N2) stage III NSCLC or superior sulcus tumor, and present an overview of the principles for optimisation of the risk/benefit. Numerous clinical questions remain, and enrolment of patients into well-designed clinical trials should be encouraged.
Similar content being viewed by others
Main
Lung cancer is the leading cause of death from cancer in Japan as well as in other industrialised nations. Non-small-cell lung cancer (NSCLC) accounts for about 80% of all cases.
About one-third of all cases of NSCLC present with locally advanced, stage IIIA/IIIB disease, most frequently with mediastinal node involvement (N2). Surgical resection was employed as ‘standard’ therapy for relatively less advanced ‘resectable’ cases with N2 NSCLC; however, the prognosis was not favourable (Suzuki et al, 1999). For more advanced, ‘bulky’ unresectable N2 disease, neither satisfactory local control nor satisfactory suppression of micrometastases was achieved with definitive thoracic radiotherapy (Schaake-Koning et al, 1992; Dillman et al, 1996).
Systemic chemotherapy was introduced two decades ago for cases with stage III N2 NSCLC (Le Chevalier et al, 1991; Schaake-Koning et al, 1992; Sause et al, 1995; Dillman et al, 1996), aimed at both eradication of micrometastases and improvement of local control. A multimodality approach to treatment, for example, systemic chemotherapy combined with definitive local therapy, is now the most preferred approach in the battle against stage III NSCLC. In particular, trimodality therapy, combining surgery, radiotherapy and chemotherapy, has been intensively investigated often with promising results. The sequence of ‘trimodality’ therapy that has most often been employed is induction chemoradiotherapy, followed by surgical resection, with or without consolidation chemotherapy. Although such therapy has sometimes been shown to be highly effective, it is also highly toxic, with a reported treatment-related death rate of as high as 10%. Careful evaluation of the risk/benefit ratio of such therapy is thus indispensable.
On the other hand, a small subset of NSCLC called superior sulcus tumour (SST) or Pancoast's tumour, in which the tumor is located in the superior sulcus and involves structures at the thoracic inlet, has posed a challenging problem for surgeons, radiation oncologists and medical oncologists alike, ever since it was first discovered (Rusch et al, 2001). However, the trimodality approach mentioned above has been shown to be associated with a relatively more favourable risk/benefit ratio in this subset of patients, for whom it currently appears to be the treatment of first choice (Rusch et al, 2001; Kunitoh et al, 2003).
In this study, we review the current data on the use of the trimodality approach in the treatment of patients with locally advanced NSCLC, and also discuss means to optimise the treatment using this approach.
Rationales for trimodality therapy
Although the strongest rationale for the use of the trimodality therapy stems from the promising results of clinical phase II data, upfront systemic chemotherapy offers several practical as well as theoretical advantages (Pisters et al, 2000). Early introduction of systemic therapy may be expected to lead to early control of micrometastases. Response to the therapy can be easily assessed by radiographic imaging, which can help physicians avoid unnecessary, ineffective therapy. Visualisation of the response could motivate the patients to accept additional potentially toxic therapy, which cannot be said for postoperative chemotherapy. In addition, as compared to the postoperative status, pre-operative patients are usually in a much fitter state for chemotherapy.
Addition of radiotherapy to preoperative chemotherapy should mainly be considered for local control (Furuse et al, 1999). It has been observed that at the time of surgery, clinical N2 NSCLCs and SSTs are often even more advanced in stage than was expected preoperatively, and the complete resection rates are not sufficiently satisfactory. With the addition of radiotherapy, a greater tumour response can be expected, with the hope of better local control. Hypothetical dissemination of tumour cells during surgery may also be prevented.
Toxicity of the chemoradiotherapy
Concurrent chemoradiotherapy is often employed as induction therapy in the trimodality approach. As compared with chemotherapy alone or sequential chemoradiotherapy, concurrent chemoradiotherapy has been associated with a higher incidence of haematologic and oesophageal toxicities (Furuse et al, 1999). However, the toxicity has generally been reported to be manageable, with few deaths related to treatment toxicity.
In some trials, patients undergoing definitive surgery have received a couple of courses of consolidation chemotherapy after operation. However, the compliance rate for this strategy was reported to be poor (Pisters et al, 2000; Rusch et al, 2001). In addition, some deaths related to drug toxicity have also been reported during the consolidation phase (Albain et al, 2005), prompting further questioning of its benefits. The role of consolidation therapy after surgery, therefore, still remains to be established.
Surgical problems in the trimodality approach and their management
Surgical resection adopted in the trimodal treatment approach is limited exclusively to a major lung resection such as lobectomy or pneumonectomy. As trimodality treatment is usually indicated for stage IIIA or IIIB disease, hilar and mediastinal lymph node dissection is also mandatory. Although preoperative chemoradiotherapy could yield better locoregional control, it would also result in a ‘frozen’ hilum and/or mediastinum. Sometimes very effective induction treatment may make it that much more difficult for the thoracic surgeon to dissect the hilum and mediastinum. Prior evaluation of the mediastinal lymph nodes by mediastinoscopy is often necessary, and this procedure also leads to a local fibrosis, which makes surgical dissection difficult. The surgical mortality associated with pneumonectomy and lobectomy without prior induction treatment has been reported to vary from 3.1 to 17.0, and 0.3 to 10.1%, respectively (Watanabe et al, 2004). On the other hand, when they are performed after induction chemoradiotherapy, the surgical mortality is markedly increased for both procedures (Table 1).
The ability to safely perform major lung resection following induction chemoradiotherapy would depend on several factors. Among the most important is to secure the major vessels intraoperatively. Preoperative induction treatment would melt hilar and/or mediastinal lymph nodes. As a result, these lymph nodes often become adherent to major vessels, making dissection difficult. Dissection of such lymph nodes adhering to vessels without the utmost care could lead to massive intraoperative bleeding. In such a situation, the major vessels, such as the pulmonary artery and vein, should be clamped proximally and distally to prepare for an unforeseen massive bleeding. Thoracic surgeons must not hasten to dissect such nodes. Martin et al (2001) reported three significant predictors of the postoperative complications: intraoperative blood loss, forced expiratory volume in the first second (percent predicted), and right pneumonectomy. Thus, thoracic surgeon must attempt their utmost to control and minimise intraoperative bleeding.
Second, the risk of bronchopleural fistula, one of the fatal complications, should be borne in mind. To prepare for minimising the risk of development of bronchopleural fistula, Stamatis et al (2002) recommended a reinforcement of the bronchial stump (Eberhardt et al, 1998). They have used thymus/mediastinal fat (89%) to cover the bronchial stump, and reported favourable results. Other materials for covering the stump include an intercostal muscle flap or diaphragmatic flap. They reported that none of their patients developed bronchopleural fistula ever since they adopted routine coverage of the bronchial stump with a vital flap. Bronchopleural fistula has been reported to develop in 0–15% of surgical patients receiving trimodality treatment. This fatal complication occurs more frequently in cases undergoing pneumonectomy, especially right pneumonectomy. Thus, coverage of the bronchial stump is strongly recommended in cases undergoing right pneumonectomy. Omentopexy may sometimes be indicated.
Finally, avoidance of postoperative pulmonary oedema is important. We usually restrict fluid administration and institute aggressive diuretic therapy postoperatively for at least first 3 days. Some recommend the use of a steroid postoperatively to avoid pulmonary oedema (Eberhardt et al, 1998; Stamatis et al, 2002).
Right pneumonectomy has been reported from various studies to be associated with very high morbidity/mortality (Table 1). Therefore, when preoperative evaluation suggests the necessity for right pneumonectomy to accomplish R0 surgery, for example, for a tumour located in the lower lobe with bulky hilar nodes, the indications for surgery must be evaluated very cautiously. Careful assessment of pulmonary function, diffusion capacity, and a quantitative ventilation scan would be necessary. Surgery should be offered only to highly selected cases, and switching to another treatment option, such as definitive chemoradiotherapy, must be seriously considered and discussed with the patient.
Bronchovascular sleeve resection has been established as one of the standard surgical procedures to spare the lung parenchyma (Deslauriers et al, 2004). Although highly attractive in the trimodality approach for lung cancer treatment, the feasibility of this procedure after induction chemoradiotherapy, as well as its efficacy, has yet to be confirmed.
Finally, it should be noted that surgical safety tends to be better in single-institution reports (Table 1). Therefore, methods for surgical quality control should be established for multi-institutional settings.
Specific diseases
Stage III N2 disease
Standard treatment for N2 NSCLC
Until the 1970s, the standard treatment for N2 NSCLC had been surgery for ‘resectable’, and definitive radiotherapy for ‘unresectable’ disease, although the treatment results remained very poor, with few long-term survivors. Neither preoperative nor postoperative radiotherapy improved the outcome.
A series of small phase III trials showed that preoperative platinum-based chemotherapy improved the survival in patients with ‘resectable’ N2 disease (Rosell et al, 1994; Roth et al, 1994). Although the results could not be reproduced in a larger randomised trial (Depierre et al, 2002) in the same subset of N2 patients, the role of systemic chemotherapy remains unequivocal, given the very high systemic relapse rate with local therapy alone. More recent trials have shown that postoperative adjuvant chemotherapy may improve the outcome in pathologically staged N2 patients (The International Adjuvant Lung Cancer Trial Collaborative Group, 2004; Douillard et al, 2006).
Platinum-based chemotherapy was also shown to improve the survival of NSCLC patients with ‘unresectable’ N2 disease, when it was added to definitive thoracic radiotherapy (Le Chevalier et al, 1991; Schaake-Koning et al, 1992; Sause et al, 1995; Dillman et al, 1996). Concurrent chemoradiotherapy was demonstrated to be superior to sequential chemoradiotherapy (Furuse et al, 1999). However, the optimal treatment strategy, including the roles of induction/consolidation therapy as well as the most suitable chemotherapy regimen remains undetermined.
With reports of the favourable outcome of concurrent chemoradiotherapy in stage III NSCLC cases with N2 disease, for which, therefore, this strategy now represents the standard treatment, the definition of ‘resectable’ N2 disease has become even more nebulous. In fact, surgery may not be indicated at all for clinically suspected and pathologically confirmed (via mediastinoscopy) N2 disease, even when the disease is technically ‘resectable’ (Albain et al, 2005).
Trimodality treatment for N2 NSCLC
Most of the reports of the usefulness of the trimodality approach for N2 NSCLC are based on the results of phase II or retrospective trials of preoperative chemoradiotherapy (Faber et al, 1989; Rusch et al, 1993; Deutsch et al, 1994; Albain et al, 1995; Choi et al, 1997; Eberhardt et al, 1998; Katakami et al, 1998; Thomas et al, 1999; Doddoli et al, 2001; Martin et al, 2001; Stamatis et al, 2002; Sonett et al, 2004; Cerfolio et al, 2005; Daly et al, 2006). There are some highly promising and encouraging reports of long-term survival rates of around 30%, however, the toxicity is also substantial, usually exceeding that observed with other multimodality therapy.
In view of the promising but controversial data, a few phase III trials were conducted; the ‘control’ arms of the studies were variable, reflecting the heterogeneity of N2 NSCLC, and consequently, so were the ‘concepts’ of trimodality.
In some studies, the trimodality approach appeared to derive from efforts to intensify preoperative induction chemotherapy. Before 2001, two small-scale randomised trials reported the results of trimodality vs induction chemotherapy for N2 NSCLC. The results of neither trial, the one showing a positive (Fleck et al, 1993) and the other showing a negative (Sauvaget et al, 2000) effect, have been published as full articles. More recently, another larger trial from Germany compared preoperative chemoradiotherapy with preoperative chemotherapy and postoperative radiotherapy, and reported no significant differences in the results (Semik et al, 2004). However, the actual issue should be viewed as an evaluation of the timing or sequence of the therapy, rather than as an investigation of the usefulness of the trimodality approach itself. The ‘induction chemotherapy with or without radiotherapy’ concept has now been introduced in recently initiated trials in North America and Europe.
The trimodality approach could be viewed as chemoradiotherapy followed by salvage surgery of the residual tumour. A large-scale US trial, INT0139, compared surgical resection and boost radiotherapy, in patients with N2 NSCLC receiving induction chemoradiotherapy (Albain et al, 2005). Although the progression-free survival (PFS) rate favoured the surgery (trimodality) arm, the overall survival rate was not statistically significantly different between the two arms, with only a marginally larger number of long-term survivors in the surgery arm.
Relapse pattern and its implications
Local relapse as well as emergence of distant metastases remains a big problem in N2 NSCLC patients treated by chemoradiotherapy. Concurrent chemoradiotherapy was reported to be better for local control as compared to sequential therapy (Furuse et al, 1999); however, the locoregional relapse rate remained high. One of the aims of the trimodality approach is to obtain better local control with surgical resection. In fact, the local relapse rate appeared to have decreased, especially in R0-surgery cases. In an intention-to-treat analysis, ‘local relapse only’ accounted for 10% of the cases showing disease progression in the trimodality arm of INT0139 (Albain et al, 2005), whereas it accounted for 22% of the cases showing disease progression in the chemoradiotherapy arm (P=0.002). However, these figures might have been biased by competitive risks; as the trimodality approach was associated with a larger number of treatment-related deaths, and as it is plausible that cases at a higher risk of postoperative morbidity/mortality were more likely suffer from uncontrollable local tumours, the local control rate with the trimodality approach could have been exaggerated by the exclusion of these high-risk patients. In addition, clinical diagnosis of failure of local control with chemoradiotherapy is often difficult because of the confounding effect of radiation fibrosis, the radiological appearance of which sometimes mimics recurrent tumours. It may not be worthwhile placing much emphasis on the difference in relapse patterns among different modalities.
One of the major problems with the use of combined modality treatment for locally advanced NSCLC is the high risk of brain metastasis (Stuschke et al, 1999; Thomas et al, 1999). A substantial proportion of patients undergoing successful R0 resection suffer from brain-only relapse. A non-randomised observational study suggested that prophylactic cranial irradiation (PCI) might reduce the risk of brain metastasis in these patients (Stuschke et al, 1999). Whether or not PCI would benefit optimally treated patients with locally advanced NCLC is now under investigation in randomised trials.
Prognostic and predictive factors
Not surprisingly, complete resection (R0 operation), which should be the aim of induction chemoradiotherapy, is associated with a better prognosis. Besides, eradication of tumour cells in the mediastinal nodes has also been reported to be a favourable prognostic factor (Choi et al, 1997; Albain et al, 2005). However, the problem is that the clinical response to induction therapy as judged by CT imaging, seems to be a poor predictor of the pathologic ‘downstaging’. There are some reports that suggest that repeated mediastinoscopy should be conducted to evaluate the status of the mediastinal nodes after induction therapy and predict the postoperative outcomes (Mateu-Navarro et al, 2000); however, this is not widely employed because of the technical difficulties involved. FDG-PET is currently being investigated as a promising tool for reliable assessment of the response to treatment (Pottgen et al, 2006).
Pathological complete response (pCR), defined as absence of viable cells in the resected specimen, has been reported to be a good prognostic factor by some, but not others. Although pCR is an established prognostic factor in patients receiving induction chemotherapy, inclusion of radiotherapy is likely to modify the information based on the locoregional response status on the effect of systemic chemotherapy against micrometastases.
Evidently, these prognostic factors, which are associated with a good response to induction therapy, would be associated with a better outcome even without subsequent surgery. Therefore, these are not necessarily predictive factors of the response to trimodality treatment, that is, it is still unclear whether surgery might be more beneficial in these patients. The only known ‘predictive’ factor of the outcome of surgical resection, which is actually a negative factor, is the necessity for pneumonectomy (Albain et al, 2005). An exploratory subset analysis in INT0139 revealed that patients undergoing pneumonectomy did poorly as compared to matched controls. This is clearly due to excessive early toxic deaths after pneumonectomy, in particular, right pneumonectomy or complex left pneumonectomy (see surgical problems section above). This surgical morbidity and mortality might well offset the advantage of PFS in the trimodality arm.
Superior sulcus tumours
Superior sulcus tumours have long been treated by preoperative radiation and resection, but both the curative resection (R0) rate (50%) and the long-term survival rate (30%) have remained poor and unchanged over the last 40 years (Rusch et al, 2001). Two large-scale phase II trials from the US and Japan (Rusch et al, 2001; Kunitoh et al, 2003) suggested that preoperative concurrent chemoradiotherapy could improve the outcome in these patients. In both series, the R0 rate was approximately 70%, with a 5-year survival rate of 40–50%. The treatment-related death rate was acceptably low at 4%.
Because of the infrequent occurrence of this tumour subtype, a randomised trial would be extremely difficult. Therefore, given the reproducibility of the favourable results as described above, the trimodality approach may be accepted as the standard treatment strategy for SSTs.
The relatively low morbidity/mortality of trimodality treatment in patients with SSTs would be ascribed to the small size of the irradiation field, which is a known predictive factor for radiation toxicity. Theoretically, it would allow escalation of the radiation dose, however, intensification of chemotherapy and not radiotherapy should be the next logical step for further improvement of the results, because the relapse pattern in these cases is predominantly represented by distant metastases (Rusch et al, 2001; Kunitoh et al, 2003). Brain metastasis is also a challenging problem in cases with SSTs, and PCI may have a role in the management of these patients.
T4 tumours (other than SSTs)
Induction chemoradiotherapy might be beneficial for patients with other T4 diseases, which invade the major vessels or organs. Clinical response to the induction therapy may allow the surgeons to resect the initially unresectable tumour. However, surgical resection of T4 lung cancer, involving the carina, atrium, and/or vena cava, is technically challenging, and surgical morbidity is still high even for surgery alone (Tsuchiya et al, 1994). Grunenwald et al (2001) reported a surgical mortality after chemoradiotherpy of 7% and 5-year survival rate of 19%. As mediastinal cleaning by induction therapy was reported to be prognostic, patients with T4N0-1 disease might be good candidates for an attempt of this approach. However, this remains to be confirmed in a prospective study.
Summary and conclusions
Optimal management of patients undergoing trimodality treatment
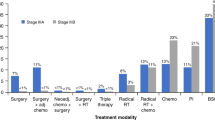
The trimodality approach, although it is sometimes highly effective, poses substantial risks to the patients. The risk/benefit ratio must be carefully evaluated on an individual basis (Figures 1 and 2).
As the candidates for this treatment approach have locally advanced disease, potential distant metastasis should be excluded by complete staging, preferably by methods including brain MRI and whole-body PET scans, before the initiation of therapy. After the induction therapy, in addition to re-staging of the local disease by CT imaging, brain MRI should be repeated, considering the high risk of brain metastasis.
Although downstaging of the tumour after induction chemoradiotherapy sometimes does occur, physicians should not enrol patients with technically unresectable disease at presentation, with the hope of conversion of unresectable to resectable disease after induction therapy. The exception, of course, is SST, in which apparently unresectable T4 disease at presentation does not represent a contraindication to trimodality treatment aimed at complete resection (Rusch et al, 2001; Kunitoh et al, 2003). There are no data on the results of trimodality treatment in cases of SSTs with N2 disease, therefore, this approach cannot yet be recommended for these patients at present.
Right pneumonectomy after induction chemoradiotherapy has been reported to be associated with unacceptably high surgical morbidity/mortality (Albain et al, 2005), and patients in whom a right pneumonectomy for R0 resection would be indicated should be very cautiously evaluated to determine whether or not they might be suitable candidates for the trimodality approach. Physicians should also be discouraged from considering the trimodality approach for such a patient in the hope of downstaging of the tumour with induction therapy.
Conclusions
For locally advanced NSCLC patients with clinical N2 disease, the trimodality approach, although promising, should still be considered as investigational therapy. The suitability of a given patient for this therapy must be meticulously determined by surgeons, radiation oncologists, medical oncologists and chest physicians. For SSTs, the trimodality approach can now be considered as standard therapy, but it should be managed by an experienced multimodality team as the risk remains substantial, with a treatment-related death rate of 4%. Enrolment of patients into clinical trials is strongly encouraged as there still remain numerous unanswered questions.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Albain KS, Rusch VW, Crowley JJ, Rice TW, Turrisi III AT, Weick JK, Lonchyna VA, Presant CA, McKenna RJ, Gandara DR (1995) Concurrent cisplatin/etoposide plus chest radiotherapy followed by surgery for stages IIIA (N2) and IIIB non-small-cell lung cancer: mature results of Southwest Oncology Group phase II study 8805. J Clin Oncol 13: 1880–1892
Albain KS, Swann RS, Rusch VR, Turrisi AT, Shepherd FA, Smith CJ, Gandara DR, Johnson DH, Green MR, Miller RC (2005) Phase III study of concurrent chemotherapy and radiotherapy vs chemotherapy and radiotherapy followed by surgical resection for stageIIIA(pN2) non-small cell lung cancer: Outcomes update of North American Intergroup: Intergroup trial 0139. Proc Am Soc Clin Oncol 23: 624S (abstr 7014)
Cerfolio RJ, Bryant AS, Spencer SA, Bartolucci AA (2005) Pulmonary resection after high-dose and low-dose chest irradiation. Ann Thorac Surg 80: 1224–1230; discussion 1230
Choi NC, Carey RW, Daly W, Mathisen D, Wain J, Wright C, Lynch T, Grossbard M, Grillo H (1997) Potential impact on survival of improved tumour downstaging and resection rate by preoperative twice-daily radiation and concurrent chemotherapy in stage IIIA non-small-cell lung cancer. J Clin Oncol 15: 712–722
Daly BD, Fernando HC, Ketchedjian A, Dipetrillo TA, Kachnic LA, Morelli DM, Shemin RJ (2006) Pneumonectomy after high-dose radiation and concurrent chemotherapy for nonsmall cell lung cancer. Ann Thorac Surg 82: 227–231
Depierre A, Milleron B, Moro-Sibilot D, Chevret S, Quoix E, Lebeau B, Braun D, Breton JL, Lemarie E, Gouva S, Paillot N, Brechot JM, Janicot H, Lebas FX, Terrioux P, Clavier J, Foucher P, Monchatre M, Coetmeur D, Level MC, Leclerc P, Blanchon F, Rodier JM, Thiberville L, Villeneuve A, Westeel V, Chastang C (2002) Preoperative chemotherapy followed by surgery compared with primary surgery in resectable stage I (except T1N0), II, and IIIa non-small-cell lung cancer. J Clin Oncol 20: 247–253
Deslauriers J, Gregoire J, Jacques LF, Piraux M, Guojin L, Lacasse Y (2004) Sleeve lobectomy vs pneumonectomy for lung cancer: a comparative analysis of survival and sites or recurrences. Ann Thorac Surg 77: 1152–1156
Deutsch M, Crawford J, Leopold K, Wolfe W, Foster W, Herndon J, Blackwell S, Yost R (1994) Phase II study of neoadjuvant chemotherapy and radiation therapy with thoracotomy in the treatment of clinically staged IIIA non-small cell lung cancer. Cancer 74: 1243–1252
Dillman RO, Herndon J, Seagren SL, Eaton Jr WL, Green MR (1996) Improved survival in stage III non-small-cell lung cancer: seven-year follow-up of cancer and leukemia group B (CALGB) 8433 trial. J Natl Cancer Inst 88: 1210–1215
Doddoli C, Thomas P, Thirion X, Seree Y, Giudicelli R, Fuentes P (2001) Postoperative complications in relation with induction therapy for lung cancer. Eur J Cardiothorac Surg 20: 385–390
Douillard JY, Rosell R, De Lena M, Carpagnano F, Ramlau R, Gonzales-Larriba JL, Grodzki T, Pereira JR, Le Groumellec A, Lorusso V, Clary C, Torres AJ, Dahabreh J, Souquet PJ, Astudillo J, Fournel P, Artal-Cortes A, Jassem J, Koubkova L, His P, Riggi M, Hurteloup P (2006) Adjuvant vinorelbine plus cisplatin vs observation in patients with completely resected stage IB-IIIA non-small-cell lung cancer (Adjuvant Navelbine International Trialist Association (ANITA)): a randomised controlled trial. Lancet Oncol 7: 719–727
Eberhardt W, Wilke H, Stamatis G, Stuschke M, Harstrick A, Menker H, Krause B, Mueller MR, Stahl M, Flasshove M, Budach V, Greschuchna D, Konietzko N, Sack H, Seeber S (1998) Preoperative chemotherapy followed by concurrent chemoradiation therapy based on hyperfractionated accelerated radiotherapy and definitive surgery in locally advanced non-small-cell lung cancer: mature results of a phase II trial. J Clin Oncol 16: 622–634
Faber LP, Kittle CF, Warren WH, Bonomi PD, Taylor SGT, Reddy S, Lee MS (1989) Preoperative chemotherapy and irradiation for stage III non-small cell lung cancer. Ann Thorac Surg 47: 669–675; discussion; 676–677
Fleck J, Camargo J, Godoy D, Teixeira P, Braga-Filho A, Barietta A, Ferreira P (1993) Chemoradiation therapy vs chemotherapy alone as a neoadjuvant treatment for stage III non–small-cell lung cancer: preliminary report of a phase III prospective randomized trial. Proc Am Soc Clin Oncol 12: 333 (abstr 1108)
Furuse K, Fukuoka M, Kawahara M, Nishikawa H, Takada Y, Kudoh S, Katagami N, Ariyoshi Y (1999) Phase III study of concurrent vs sequential thoracic radiotherapy in combination with mitomycin, vindesine, and cisplatin in unresectable stage III non-small-cell lung cancer. J Clin Oncol 17: 2692–2699
Grunenwald DH, Andre F, Le Pechoux C, Girard P, Lamer C, Laplanche A, Tarayre M, Arriagada R, Le Chevalier T (2001) Benefit of surgery after chemoradiotherapy in stage IIIB (T4 and/or N3) non-small cell lung cancer. J Thorac Cardiovasc Surg 122: 796–802
Katakami N, Okazaki M, Nishiuchi S, Fukuda H, Horikawa T, Nishiyama H, Inui H, Bando K (1998) Induction chemoradiotherapy for advanced stage III non-small cell lung cancer: long-term follow-up in 42 patients. Lung Cancer 22: 127–137
Kunitoh H, Kato H, Tsuboi M, Ishizuka N, Tsuchiya R, Ichinose Y, Katakami N, Saijo N (2003) A phase II trial of pre-operative chemoradiotherapy followed by surgical resection in pancoast tumours: initial report of Japan Clinical Oncology Group trial (JCOG 9806). Proc Am Soc Clin Oncol 22: 634 (abstr 2549)
Le Chevalier T, Arriagada R, Quoix E, Ruffie P, Martin M, Tarayre M, Lacombe-Terrier MJ, Douillard JY, Laplanche A (1991) Radiotherapy alone vs combined chemotherapy and radiotherapy in nonresectable non-small-cell lung cancer: first analysis of a randomized trial in 353 patients. J Natl Cancer Inst 83: 417–423
Martin J, Ginsberg RJ, Abolhoda A, Bains MS, Downey RJ, Korst RJ, Weigel TL, Kris MG, Venkatraman ES, Rusch VW (2001) Morbidity and mortality after neoadjuvant therapy for lung cancer: the risks of right pneumonectomy. Ann Thorac Surg 72: 1149–1154
Mateu-Navarro M, Rami-Porta R, Bastus-Piulats R, Cirera-Nogueras L, Gonzalez-Pont G (2000) Remediastinoscopy after induction chemotherapy in non-small cell lung cancer. Ann Thorac Surg 70: 391–395
Pisters KM, Ginsberg RJ, Giroux DJ, Putnam Jr JB, Kris MG, Johnson DH, Roberts JR, Mault J, Crowley JJ, Bunn Jr PA (2000) Induction chemotherapy before surgery for early-stage lung cancer: a novel approach. Bimodality lung oncology team. J Thorac Cardiovasc Surg 119: 429–439
Pottgen C, Levegrun S, Theegarten D, Marnitz S, Grehl S, Pink R, Eberhardt W, Stamatis G, Gauler T, Antoch G, Bockisch A, Stuschke M (2006) Value of 18F-fluoro-2-deoxy-D-glucose-positron emission tomography/computed tomography in non-small-cell lung cancer for prediction of pathologic response and times to relapse after neoadjuvant chemoradiotherapy. Clin Cancer Res 12: 97–106
Rosell R, Gomez-Codina J, Camps C, Maestre J, Padille J, Canto A, Mate JL, Li S, Roig J, Olazabal A (1994) A randomized trial comparing preoperative chemotherapy plus surgery with surgery alone in patients with non-small-cell lung cancer. N Engl J Med 330: 153–158
Roth JA, Fossella F, Komaki R, Ryan MB, Putnam Jr JB, Lee JS, Dhingra H, De Caro L, Chasen M, McGavran M (1994) A randomized trial comparing perioperative chemotherapy and surgery with surgery alone in resectable stage IIIA non-small-cell lung cancer. J Natl Cancer Inst 86: 673–680
Rusch VW, Albain KS, Crowley JJ, Rice TW, Lonchyna V, McKenna Jr R, Livingston RB, Griffin BR, Benfield JR (1993) Surgical resection of stage IIIA and stage IIIB non-small-cell lung cancer after concurrent induction chemoradiotherapy. A Southwest Oncology Group trial. J Thorac Cardiovasc Surg 105: 97–104; discussion; 104–106
Rusch VW, Giroux DJ, Kraut MJ, Crowley J, Hazuka M, Johnson D, Goldberg M, Detterbeck F, Shepherd F, Burkes R, Winton T, Deschamps C, Livingston R, Gandara D (2001) Induction chemoradiation and surgical resection for non-small cell lung carcinomas of the superior sulcus: initial results of Southwest Oncology Group Trial 9416 (Intergroup Trial 0160). J Thorac Cardiovasc Surg 121: 472–483
Sause WT, Scott C, Taylor S, Johnson D, Livingston R, Komaki R, Emami B, Curran WJ, Byhardt RW, Turrisi AT (1995) Radiation therapy oncology group (RTOG) 88-08 and eastern cooperative oncology group (ECOG) 4588: preliminary results of a phase III trial in regionally advanced, unresectable non-small-cell lung cancer. J Natl Cancer Inst 87: 198–205
Sauvaget J, Rebischung JL, Vannetzel JM (2000) Phase III study of neo-adjuvant MVP vs MVP plus chemo-radiotherapy in stage III NSCLC. Proc Am Soc Clin Oncol 19: 495a (abstr1935)
Schaake-Koning C, van den Bogaert W, Dalesio O, Festen J, Hoogenhout J, van Houtte P, Kiekpatrick A, Koolen M, Maat B, Nijs A (1992) Effects of concomitant cisplatin and radiotherapy on inoperable non-small-cell lung cancer. N Engl J Med 326: 524–530
Semik M, Riesenbeck D, Linder A, Schmid C, Hoffknecht P, Heinecke A, Scheld H, Thomas M (2004) Preoperative chemotherapy with and without additional radiochemotherapy: benefit and risk for surgery of stage III non-small cell lung cancer. Eur J Cardiothorac Surg 26: 1205–1210
Sonett JR, Suntharalingam M, Edelman MJ, Patel AB, Gamliel Z, Doyle A, Hausner P, Krasna M (2004) Pulmonary resection after curative intent radiotherapy (>59 Gy) and concurrent chemotherapy in non-small-cell lung cancer. Ann Thorac Surg 78: 1200–1205; discussion; 1206
Stamatis G, Djuric D, Eberhardt W, Pottken C, Zaboura G, Fechner S, Fujimoto T (2002) Postoperative morbidity and mortality after induction chemoradiotherapy for locally advanced lung cancer: an analysis of 350 operated patients. Eur J Cardiothorac Surg 22: 292–297
Stuschke M, Eberhardt W, Pöttgen C, Stamatis G, Wilke H, Stüben G, Stöblen F, Wilhelm HH, Menker H, Teschler H, Müller RD, Budach V, Seeber S, Sack H (1999) Prophylactic cranial irradiation in locally advanced non-small-cell lung cancer after multimodality treatment: long-term follow-up and investigations of late neuropsychologic effects. J Clin Oncol 17: 2700–2709
Suzuki K, Nagai K, Yoshida J, Nishimura M, Takahashi K, Nishiwaki Y (1999) The prognosis of surgically resected N2 non-small cell lung cancer: the importance of clinical N status. J Thorac Cardiovasc Surg 118: 145–153
The International Adjuvant Lung Cancer Trial Collaborative Group (2004) Cisplatin-based adjuvant chemotherapy in patients with completely resected non-small-cell lung cancer. N Engl J Med 350: 351–360
Thomas M, Rübe C, Semik M, von Eiff M, Freitag L, Macha HN, Wagner W, Klinke F, Scheld HH, Willich N, Berdel WE, Junker K (1999) Impact of preoperative bimodality induction including twice-daily radiation on tumour regression and survival in stage III non-small-cell lung cancer. J Clin Oncol 17: 1185–1193
Tsuchiya R, Asamura H, Kondo H, Goya T, Naruke T (1994) Extended resection of the left atrium, great vessels, or both for lung cancer. Ann Thorac Surg 57: 960–965
Watanabe S, Asamura H, Suzuki K, Tsuchiya R (2004) Recent results of postoperative mortality for surgical resections in lung cancer. Ann Thorac Surg 78: 999–1002; discussion 1002–1003
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Kunitoh, H., Suzuki, K. How to evaluate the risk/benefit of trimodality therapy in locally advanced non-small-cell lung cancer. Br J Cancer 96, 1498–1503 (2007). https://doi.org/10.1038/sj.bjc.6603751
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6603751
Keywords
This article is cited by
-
Pneumonectomy for node-positive non-small cell lung cancer: can it be a treatment option for N2 disease?
General Thoracic and Cardiovascular Surgery (2014)