Abstract
We performed a prospectively randomised clinical trial to compare the efficacy of four subcutaneous interleukin-2-(sc-IL-2) and sc interferon-α2a (sc-IFN-α2a)-based outpatient regimens in 379 patients with progressive metastatic renal cell carcinoma. Patients with lung metastases, an erythrocyte sedimentation rate ⩽70 mm h−1 and neutrophil counts ⩽6000 μl−1 (group I) were randomised to arm A: sc-IL-2, sc-IFN-α2a, peroral 13-cis-retinoic acid (po-13cRA) (n=78), or arm B: arm A plus inhaled-IL-2 (n=65). All others (group II) were randomised to arm C: arm A plus intravenous 5-fluorouracil (iv-5-FU) (n=116), or arm D: arm A plus po-Capecitabine (n=120). Median overall survival (OS) was 22 months (arm A; 3-year OS: 29.7%) and 18 months (arm B; 3-year OS: 29.2%) in group I, and 18 months (arm C; 3-year OS: 25.7%) and 16 months (arm D; 3-year OS: 32.6%) in group II. There were no statistically significant differences in OS, progression-free survival, and objective response between arms A and B, and between arms C and D, respectively. Given the known therapeutic efficacy of sc-IL-2/sc-INF-α2a/po-13cRA-based outpatient chemoimmunotherapies, our results did not establish survival advantages in favour of po-Capecitabine vs iv-5-FU, and in favour of short-term inhaled-IL-2 in patients with advanced renal cell carcinoma receiving systemic cytokines.
Similar content being viewed by others
Main
The prognosis of metastatic renal carcinoma remains poor. Although this tumour is highly resistant to chemotherapy and hormone therapy, promising results have been reported with the use of molecular agents that is, recombinant cytokines, notably recombinant interleukin-2 (IL-2) and interferon-α (IFN-α), given intravenously, subcutanously alone or in combination in outpatient regimens with objective response rates between 6 and 31% (Rosenberg et al, 1987; Atzpodien et al, 1990; Sleijfer et al, 1992; Jayson et al, 1998; Tourani et al, 2003).
When the present trial was planned, various studies focused on the combination of immunmodulator substances and chemotherapeutic agents to increase antitumour activity. In preliminary reports on oral 13-cis-retinoic acid (po-13cRA), a cell differentiation regulator, po-13cRA could enhance antitumour efficacy in IL-2/IFN-α- or chemoimmunotherapy-treated metastatic renal cell carcinoma patients, with objective response rates between 17 and 42% (Atzpodien et al, 1995; Stadler et al, 1998). In the presence of pulmonary metastases, locoregional administration of inhaled-IL-2 was reported to yield low toxicity combined with objective response rates of pulmonary disease of 2.5–21% (Lorenz et al, 1996; Merimsky et al, 2004). Other reports showed that the combination of cytokines with intravenous 5-fluorouracil (iv-5-FU) could increase objective response rates to between 12 and 39% (van Herpen et al, 2000; Atzpodien et al, 2001, 2004). Preliminary results of a phase II study combining IL-2/IFN-α with oral Capecitabine, which is converted to 5-FU in vivo, reported objective response rates of 34% (Oevermann et al, 2000).
Here, we prospectively compared the long-term therapeutic efficacy of four outpatient combination regimens: arm A (sc-IL-2, sc-IFN-α2a, po-13cRA) and arm B (arm A plus inhaled-IL-2) in patients with pulmonary disease, and arm C (arm A plus iv-5-FU) and arm D (arm A plus po-Capecitabine) in all others.
Patients and methods
Patients
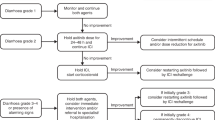
Three hundred and seventy-nine patients with metastastic renal cell carcinoma were stratified into two groups (Figure 1). Group I patients (n=143) were subsequently randomised to arm A (sc-IL-2, sc-IFN-α2a, po-13-cRA) or arm B (arm A plus inhaled-IL-2), whereas group II patients (all others; n=236) were randomised to arm C (arm A plus iv-5-FU) or arm D (arm A plus po-Capecitabine). Median follow-up of these patients was 18 months (range 0–83 months). Patient pretreatment included radical tumour nephrectomy (n=343), radiotherapy (n=51), chemotherapy (n=11), immunotherapy (n=18), chemoimmunotherapy (n=19), naturopathic therapy (n=2), and others (n=7) (Table 1).
Criteria for entry into the trial were as follows: histologically confirmed progressive and irresectable metastatic renal cell carcinoma; an expected survival duration of more than 3 months; Karnofsky performance status >80%; age between 18 and 80 years; white blood cell count >3500 μl−1; platelet count >100 000 μl−1; haematocrit >30%; serum bilirubin, and creatinine <1.25 of the upper normal limit; no evidence of congestive heart failure, no severe coronary artery disease, no cardiac arrhythmias, no clinically symptomatic CNS disease or seizure disorders, no human immunodeficiency virus infection, no evidence of chronic active hepatitis, no concomitant corticosteroid therapy. In all patients treated, no chemotherapy or immunomodulatory treatment had been performed during the previous 4 weeks. Also, pregnant and lactating women were excluded.
Treatment was approved by the institutional review board, written informed consent was obtained from all patients before entry into the trial. Fifty-four participating centres entered a total of 379 eligible patients into this trial.
Treatment design
Patients were stratified into two groups according to the clinical characteristics adapted from Lopez-Hänninen et al (1996). Group I consisted of patients with lung metastases, an erythrocyte sedimentation rate ⩽70 mm h−1, and neutrophil counts ⩽6000 μl−1; group II included all other patients. As all treatment regimens were designed to be administered in the outpatient setting, this required selection of patients with good or fair performance status. Upon written receipt of patient pre-treatment evaluation, per centre block randomisation was performed to rule out centre-related statistical bias. Patients stratified to group I or II were randomised according to a per centre 1 : 1 randomisation. Group I patients received arm A (sc-IL2, sc-IFN-α2a, po-13-cRA) or arm B (arm A plus inhaled-IL-2), whereas group II patients received either arm C (arm A plus iv-5-FU) or arm D (arm A plus po-Capecitabine).
Regimens
Treatment arm A consisted of sc-IFN-α2a (Roferon, Hoffmann-La Roche, Grenzach-Wyhlen, Germany) (5 × 106 IU m−2, day 1, weeks 1+4; days 1, 3, 5, weeks 2–3; 10 × 106 IU m−2, days 1, 3, 5, weeks 5–8), sc-IL-2 (Proleukin, Chiron, Emeryville) (10 × 106 IU m−2, twice daily, days 3–5, weeks 1+4; 5 × 106 IU m−2, days 1, 3, 5, weeks 2+3), and po-13cRA (20 mg 3 × daily) over 8 weeks. Treatment arm B consisted of treatment arm A combined with inhaled-IL-2 (Proleukin, Chiron, Emeryville) (9 × 106 IU/2.5 ml basic solution, four times a day, days 1–5, weeks 2+3 and weeks 5–8); the IL-2 (2 × 18 × 106 IU) was dissolved in 10 ml 5% glucose solution, out of which 2.5 ml (9 × 106 IU IL-2 in solution) was taken for each of the four daily administrations; IL-2 was inhaled using a Salvia Lifetec Jetair inhalator (Kronberg, Germany) constantly providing 3 μm particles. Treatment arm C consisted of arm A plus iv-5-FU (1000 mg m−2, day 1, weeks 5–8). Treatment arm D consisted of treatment arm A combined with po-Capecitabine (1000 mg m−2 twice daily, days 1–5, weeks 5–8).
Eight-week treatment cycles were repeated for up to three courses unless progression of disease occurred. Patients with an unchanged tumour response in cycle two did not receive a subsequent third treatment cycle.
Re-evaluation of the patients tumour status was performed between treatment cycles. Arm A, B, C, and D patients received a mean of 1.6, 1.6, 1.5, and 1.6 8-week cycles, respectively (range 1–6). Concomitant medication was given as needed to control adverse effects of chemoimmunotherapy. Sixty patients (15.8%) (arm A: 14%; arm B: 9.2%; arm C: 21.6%; arm D: 15%) did not complete cycle one owing to early disease progression before the first evaluation (2.9%), intolerance (8.7%), death during therapy (1.6%), patients’ wish (2.1%), and non-compliance (0.5%), respectively. Less than 4% of patients required in-patient care throughout treatment. All patients were seen at regular weekly or bi-weekly intervals by oncologic specialists; additional care was provided whenever needed.
Assessment of response, survival, and toxicity
Response to therapy was evaluated according to World Health Organization (WHO) criteria on an intent-to-treat basis. All responses were reviewed by Board-certified expert radiologists. In case of progression upon first re-evaluation after 8 weeks of treatment, progression-free survival (PFS) was calculated at 0 months. Survival was measured from start of therapy to date of death or to the last known date to be alive. All patients had to be followed up for survival for at least 3 years as cutoff.
Systemic maximum toxicity was evaluated using a grading system adapted from the WHO.
Statistical analysis
The statistical end points in our analysis were (1) OS, (2) PFS, and (3) objective response of patients. The probability of OS and PFS was plotted over time according to the method of Kaplan and Meier (1958). Statistical significance was assessed using the log-rank test.
The 3-year survival rates were hypothesised to show a 20% advantage of arm B over arm A (40 vs 20%), and a 15% advantage of arm D over arm C (30 vs 15%). Using an α of 0.05 (one-sided), a sample size of 64 patients each (arm A and arm B) and 95 patients each (arm C and arm D) was needed to have 80% power to statistically establish the assumed difference in 3-year survival rates. To meet these statistical end points, randomisation was performed 1 : 1 for groups I and II, respectively.
Results
A total of 379 metastatic renal carcinoma patients were treated: 143 group I patients with pulmonary metastases (median OS: 21 months) were randomised to receive sc-IL-2, sc-IFN-α2a, and po-13cRA (arm A); or arm A plus inhaled-IL-2 (arm B); 236 group II patients (median OS: 17 months) were randomised to receive arm A plus iv-5-FU (arm C); or arm A plus po-Capecitabine (arm D).
Treatment response
Eight arm A (sc-IL-2/sc-IFN-α2a/po-13cRA) treated patients (10%) achieved a complete response and 15 patients (19%) had a partial remission (Table 2). The overall objective response rate was 29% (95% CI 19, 40). Twenty-eight patients (36%) showed disease stabilisation and 27 patients (35%) exhibited continuous disease progression despite therapy.
In arm B (arm A plus inhaled-IL-2), there were eight complete responders (12%) and 12 partial responders (19%), with an overall objective response rate of 31% (95% CI 20, 44). Seventeen patients (26%) had disease stabilisation, and in 28 patients (43%) a continuous disease progression was observed.
In arm C (arm A plus iv-5-FU), four patients (3%) achieved a complete response and 18 patients (16%) had a partial remission. The overall objective response rate was 19% (95% CI 13, 27). Thirty patients (26%) showed disease stabilisation and 64 patients (55%) exhibited continuous disease progression despite therapy.
Nine arm D (arm A plus po-Capecitabine) treated patients (7%) achieved a complete response and 23 patients (19%) had a partial remission. The overall objective response rate was 26% (95% CI 19, 35). Thirty-two patients (27%) showed disease stabilisation, and in 56 patients (47%) a continuous disease progression was observed.
Progression-free survival
Seven patients (9%) in arm A (sc-IL-2/IFN-α2a/po-13cRA), six patients (9%) in arm B (arm A plus inhaled-IL-2), five patients (4%) in arm C (arm A plus iv-5-FU), and nine patients (8%) in arm D (arm A plus po-Capecitabine) remained progression-free at last follow-up. Patients reached a median PFS of 5 months in arm A (3-year PFS: 8.8%) and 4 months in arm B (3-year PFS: 10.8%). Median PFS was 0 months in arm C (3-year PFS: 7.8%) and 4 months in arm D (3-year PFS: 9.3%) (Figure 2). There was no statistically significant difference in PFS between arms A and B (P=0.9837), and between arms C and D (P=0.3265).
Progression-free survival: Kaplan–Meier estimates. Arm A, sc-IL-2, sc-IFN-α2a, po-13-cis-retinoic acid; n=78; median PFS, 5 months; 3-year PFS, 8.8%. Arm B, sc-IL-2, sc-IFN-α2a, po-13-cis-retinoic acid, inhaled-IL-2; n=65; median PFS, 4 months; 3-year PFS, 10.8%. Arm C, sc-IL-2, sc-IFN-α2a, po-13-cis-retinoic acid, iv-5-FU; n=116; median PFS, 0 months; 3-year PFS, 7.8%. Arm D, sc-IL-2, sc-IFN-α2a, po-13-cis-retinoic acid, po-Capecitabine; n=120; median PFS, 4 months; 3-year PFS, 9.3%.
Overall survival
Seventeen patients (22%) in arm A (sc-IL-2/sc-IFN-α2a/po-13cRA), 13 patients (20%) in arm B (arm A plus inhaled-IL-2), 16 patients (14%) in arm C (arm A plus iv-5-FU), and 22 patients (18%) in arm D (arm A plus po-Capecitabine) continued to be alive at last follow-up. Median OS was 22 months in arm A (3-year OS: 29.7%), 18 months in arm B (3-year OS: 29.2%), 18 months in arm C (3-year OS: 25.7%), and 16 months in arm D (3-year OS: 32.6%) (Figure 3). There was no statistically significant difference in OS between arms A and B (P=0.3387), and between arms C and D (P=0.5652).
Overall survival: Kaplan–Meier estimates. Arm A, sc-IL-2, sc-IFN-α2a, po-13-cis-retinoic acid; n=78; median OS, 22 months; 3-year OS, 29.7%. Arm B, sc-IL-2, sc-IFN-α2a, po-13-cis-retinoic acid, inhaled-IL-2; n=65; median OS, 18 months; 3-year OS, 29.2%. Arm C, sc-IL-2, sc-IFN-α2a, po-13-cis-retinoic acid, iv-5-FU; n=116; median OS, 18 months; 3-year OS, 25.7%. Arm D, sc-IL-2, sc-IFN-α2a, po-13-cis-retinoic acid, po-Capecitabine; n=120; median OS, 16 months; 3-year OS, 32.6%.
Treatment toxicity
All four sc-IL-2/sc-IFN-α2a/po-13-cRA-based therapies were moderately tolerated and could be administered in the outpatient setting. Most side effects were limited to WHO grades I and II, and no toxic deaths occurred. All toxicities reversed spontaneously following completion of chemoimmunotherapy.
Table 3 summarises all grade I/II and III/IV treatment-related adverse effects. More than 5% of patients experienced grade III or IV treatment-related anorexia (24% arm A, 26% arm B, 18% arm C, 26% arm D), malaise (19% arm A, 8% arm B, 11% arm C, 28% arm D), nausea/vomiting (10% arm B), chills (9% arm C, 7% arm D), fever (9% arm D), and respiratory distress (7% arm A, 7% arm C).
A total of 5% of arm A (sc-IL-2/IFN-α2a/po-13-cRA), 8% of arm B (arm A plus inhaled-IL-2), 12% of arm C (arm A plus iv-5-FU), and 8% of arm D (arm A plus po-Capecitabine) patients discontinued treatment owing to toxicity.
Discussion
In this prospectively randomised trial, we reported the results of 379 patients with progressive metastatic renal cell carcinoma who received (A) sc-IL-2, sc-IFN-α2a, po-13cRA, (B) arm A plus inhaled-IL-2, (C) arm A plus iv-5-FU, or (D) arm A plus po-Capecitabine.
We showed that patients with lung metastases, an erythrocyte sedimentation rate ⩽70 mm h−1, and neutrophil counts ⩽6000 μl−1 (group I) achieved a median OS of 22 months (arm A) and 18 months (arm B), whereas all other patients (group II) reached a median OS of 18 months (arm C) and 16 months (arm D), with no statistically significant differences. Overall, other authors reported a median OS of 17 months (sc-IL-2/sc-IFN-α/po13-cRA) (Stadler et al, 1998), 19 months (sc-IL-2/sc-IFN-α/inhaled-IL-2) (Huland et al, 1994), and 11–27 months (sc-IL-2/sc-IFN-α/po-13cRA/iv-5-FU) (Soori et al, 2002; Atzpodien et al, 2004).
It should be noted that the primary end point of the current trial was not reached, given 3-year OS-rates of 29.7% (arm A) and 29.2% (arm B) in group I, and 25.7% (arm C) and 32.6% (arm D) in group II, with no statistically significant differences.
There were also no significant differences in PFS and objective response between arms A (sc-IL-2/sc-IFN-α/po-13cRA) and B (arm A plus inhaled-IL-2), and between arms C (arm A plus iv-5-FU) and D (arm A plus po-Capecitabine). Inhaled IL-2 in poor-risk patients unfit for systemic cytokine therapy has been reported to induce remarkable effects on lung metastases leading to objective responses between 2.5–21% (inhaled-IL-2) (Lorenz et al, 1996; Merimsky et al, 2004) and 47% (inhaled-IL-2/10% sc-IL-2/INFa) (Huland et al, 1994). In this multicentre trial, inhaled-IL-2 (arm B) at a dose 5.3-fold the subcutaneous (sc) dose did not significantly enhance treatment efficacy when compared to arm A. However, there are major differences compared with other reports using inhaled-IL-2 in patient selection, complementary therapy, dose distribution, and treatment time. In this trial, we treated patients with good performance status in addition to an effective systemic chemoimmunotherapy, where further improvement of objective responses may be unlikely. We used inhalation for a mean of 1.6 cycles or 64 inhalation days compared to mean treatment times of 260 inhalation days (301 days in total) reported in poor-risk patients earlier (Huland et al, 2003). Our results confirmed safety and tolerance of inhaled-IL-2 added to effective chemoimmunotherapy.
Although the use of po-Capecitabine (arm D), as 5-FU pro-drug, yielded objective response rates of 34% in preliminary studies (Oevermann et al, 2000), here, it did not significantly impact on objective response rates and survival when compared to arm C (sc-IL-2/sc-IFN-α2a/po-13cRA/iv-5-FU). However, with comparable safety and tolerance, the oral application of Capecitabine presented a potential treatment improvement in the palliative setting.
In the present trial, all four treatment arms were moderately tolerated; yet, more than 5% of patients experienced grade III or IV treatment-related side effects, notably, anorexia and malaise. It was previously suggested that grade III and IV toxicities and reduced quality of life may be more prevalent in a po-13cRA-based treatment (Motzer et al, 2000; Atzpodien et al, 2004; Aass et al, 2005). Here, the observed antitumour effects of po-13cRA must be weighed against the toxicity profile in patients with metastatic renal cell carcinoma.
In summary, given the known therapeutic efficacy of sc-IL-2/sc-INF-α2a/po-13cRA-based outpatient chemoimmunotherapies, our results did not establish survival advantages in favour of po-Capecitabine vs iv-5-FU, and in favour of short-term inhaled-IL-2 in patients with advanced renal cell carcinoma receiving systemic cytokines.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Aass N, De Mulder PHM, Mickisch GH, van Oosterom AT, van Poppel H, Fossa SD, de Prijck L, Sylvester TJ (2005) Randomized phase II/III trial of interferon alfa-2a with and without 13-cis-retinoic acid in patients with progressive metastastic renal cell carcinoma: The European Organisation for Research and Treatment of Cancer Genito-Urinary Tract Cancer Group (EORTC 30951). J Clin Oncol 23: 4172–4278
Atzpodien J, Kirchner H, Duensing S, Lopez Hanninen E, Franzke A, Buer J, Probst M, Anton P, Poliwoda H (1995) Biochemotherapy of advanced metastatic renal-cell carcinoma: results of the combination of interleukin-2, alpha-interferon, 5-fluorouracil, vinblastine, and 13-cis-retinoic acid. World J Urol 13: 174–177
Atzpodien J, Kirchner H, Illiger HJ, Metzner B, Ukena D, Schott H, Funke PJ, Gramatzki M, von Jürgenson S, Wandert T, Patzelt T, Reitz M (2001) IL-2 in combination with IFN-α and 5-FU vs tamoxifen in metastatic renal cell carcinoma: Long-term results of a controlled randomized clinical trial. Br J Cancer 85 (8): 1130–1136
Atzpodien J, Kirchner H, Jonas U, Bergmann L, Schott H, Heynemann H, Fornara P, Loening SA, Roigas J, Müller SC, Bodenstein H, Pomer S, Metzner B, Rebmann U, Oberneder R, Siebels TI, Wandert T, Patzelt T, Reitz M, DGCIN-Group (2004) Interleukin-2- and interferon-alpha2a-based immunochemotherapy in advanced renal cell carcinoma: a prospectively randomized trial of The German Cooperative Renal Carcinoma Chemoimmunotherapy Group (DGCIN). J Clin Oncol 22 (7): 1188–1194
Atzpodien J, Korfer A, Franks CR, Knuver-Hopf J, Lopez-Hanninen E, Fischer M, Mohr H, Dallmann I, Hadam M (1990) Home therapy with recombinant interleukin-2 and interferon-alpha 2b in advanced human malignancies. Lancet 335: 1509–1512
Huland E, Burger A, Fleischer J, Fornara P, Hatzmann E, Heidenreich A, Heinzer H, Heynemann H, Hoffmann L, Hofmann R, Huland H, Kampfer I, Kindler M, Kirchner H, Mehlhorn G, Moniak TH, Rebmann U, Roigas J, Schneider TH, Schnorr D, Schmitz HJ, Wenisch R, Varga Z, Vinke J (2003) Efficacy and safety of inhaled recombinant interleukin-2 in high-risk renal cell cancer patients compared with systemic interleukin-2: an outcome study. Folia Biol 49 (5): 183–190
Huland E, Heinzer H, Huland H (1994) Inhaled interleukin-2 in combination with low-dose systemic interleukin-2 and interferon alpha in patients with pulonary metastatic renal-cell carcinoma: effectiveness and toxicity of mainly local treatment. J Cancer Res Clin Oncol 120 (4): 221–228
Jayson GC, Middleton M, Lee SM, Ashcroft L, Thatcher N (1998) A randomized phase II trial of interleukin 2 and interleukin 2-interferon alpha in advanced renal cancer. Br J Cancer 78: 366–369
Kaplan EL, Meier P (1958) Nonparametric estimation from incomplete observations. J Am Stat Ass 53: 457
Lopez-Hänninen EH, Kirchner H, Atzpodien J (1996) Interleukin-2 based home therapy of metastatic renal cell carcinoma: risks and benefits in 215 consecutive single institution patients. J Urol 155: 19–25
Lorenz J, Wilhelm K, Kessler M, Peschel C, Schwulera U, Lissner R, Struff WG, Huland E, Huber C, Aulitzky WE (1996) Phase I trial of inhaled natural interleukin 2 for treatment of pulmonary malignancy: toxicity, pharmacokinetics, and biological effects. Clin Cancer Res 2: 1115–1122
Merimsky O, Gez E, Weitzen R, Nehushtan H, Rubinov R, Hayat H, Peretz T, Ben-Shahar M, Biran H, Katsenelson R, Mermershtein V, Loven D, Karminsky N, Neumann A, Matcejevsky D, Inbar M (2004) Targeting pulmonary metastases of renal cell carcinoma by inhalation of interleukin-2. Ann Oncol 15: 610–612
Motzer RJ, Murphy BA, Bacik J, Schwartz LH, Nanus DM, Mariani T, Loehrer P, Wilding G, Fairclough DL, Cella D, Mazumdar M (2000) Phase III trial of interferon alfa-2a with or without 13-cis-retinoic acid for patients with advanced renal cell carcinoma. J Clin Oncol 18 (16): 2972–2980
Oevermann K, Buer J, Hoffmann R, Franzke A, Schrader A, Patzelt T, Kirchner H, Atzpodien J (2000) Capecitabine in the treatment of metastatic renal cell carcinoma. Br J Cancer 83 (5): 583–587
Rosenberg SA, Lotze MT, Muul LM, Chang AE, Avis FP, Leitman S, Linehan WM, Robertson CN, Lee RE, Rubin JT (1987) A progress report on the treatment of 157 patients with advanced cancer using lymphokine activated killer cells and interleukin-2 or high-dose interleukin-2 alone. New Engl J Med 316: 889
Sleijfer DT, Janssen RA, Buter J, de Vries EG, Willemse PH, Mulder NH (1992) Phase II study of subcutaneous interleukin-2 in unselected patients with advanced renal cell cancer on an outpatient basis. J Clin Oncol 10: 1119–1123
Soori G, Dillman RO, Wiemann MC, Stark JJ, Tai F, DePriest CB, Church CK, Schulof R (2002) Phase II trial of subcutaneous interleukin-2, subcutaneous interferon-alpha, 5-fluorouracil and cis-retinoic acid in the treatment of renal cell carcinoma: final results of cancer biotherapy research group 94-10. Cancer Biother Radiopharm 17 (2): 165–173
Stadler WM, Kuzel T, Dumas M, Vogelzang NJ (1998) Multicenter phase II trial of interleukin-2, interferon-alpha, and 13-cis-retinoic acid in patients with metastatic renal-cell carcinoma. J Clin Oncol 6: 1820–1825
Tourani JM, Pfister C, Tubiana N, Ouldkaci M, Prevot G, Lucas V, Oudard S, Malet M, Cottu P, Ferrero JM, Mayeur D, Rixe O, Sun XS, Bernard O, Andre T, Tournigand C, Muracciole X, Guilhot J, Subcutaneous Administration Propeukin Program Cooperative Group (2003) Subcutaneous interleukin-2 and interferon alfa administration in patients with metastatic renal cell carcinoma: final results of SCAPP III, a large, multicenter, phase II, nonrandomized study with sequential analysis design – the Subcutaneous Administration Propeukin Program Cooperative Group. J Clin Oncol 21 (21): 3987–3994
van Herpen CM, Jansen RL, Kruit WH, Hoekman K, Groenewegen G, Osanto S, De Mulder PH (2000) Immunochemotherapy with interleukin-2, interferon-alpha and 5-fluorouracil for progressive metastatic renal cell carcinoma: a multicenter phase II study. Dutch Immunotherapy Working Party. Br J Cancer 82: 772–776
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Atzpodien, J., Kirchner, H., Rebmann, U. et al. Interleukin-2/interferon-α2a/13-retinoic acid-based chemoimmunotherapy in advanced renal cell carcinoma: results of a prospectively randomised trial of the German Cooperative Renal Carcinoma Chemoimmunotherapy Group (DGCIN). Br J Cancer 95, 463–469 (2006). https://doi.org/10.1038/sj.bjc.6603271
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6603271
Keywords
This article is cited by
-
Nivolumab induced encephalopathy in a man with metastatic renal cell cancer: a case report
Journal of Medical Case Reports (2018)
-
Engineering monocyte-derived dendritic cells to secrete interferon-α enhances their ability to promote adaptive and innate anti-tumor immune effector functions
Cancer Immunology, Immunotherapy (2015)
-
Association between treatment effects on disease progression end points and overall survival in clinical studies of patients with metastatic renal cell carcinoma
British Journal of Cancer (2012)
-
Sequenztherapie beim metastasierten Nierenzellkarzinom in Deutschland 2010
Der Urologe (2011)
-
Uro-Onkologie – Update 2009
Der Urologe (2009)