Abstract
The aim of the study was to demonstrate the superiority of docetaxel and epirubicin vs docetaxel alone as first-line therapy in metastatic breast cancer patients pretreated with adjuvant or neoadjuvant epirubicin. We compared single agent docetaxel 100 mg m−2 (D) with the combination of docetaxel 80 mg m−2 and epirubicin 75 mg m−2 (ED). The response rate (72 vs 79%), the progression-free survival (median 9 vs 11 months) and the overall survival (median 18 vs 21 months) were not significantly different between the ED (n=26) and D arms (n=25), respectively. Leucopaenia, nausea and stomatitis were significantly worse with ED. In conclusion, epirubicin should not be administered in combination with taxanes in metastatic breast cancer patients relapsed after an anthracycline-based adjuvant or neoadjuvant therapy.
Similar content being viewed by others
Main
Anthracyclines are among the most active agents in the treatment of metastatic and adjuvant breast cancer (Fossati et al, 1998; EBCTCG, 2004). Docetaxel is the only agent that has demonstrated survival benefits in anthracycline-resistant patients (Nabholtz et al, 1999) and superior activity over doxorubicin as first-line chemotherapy in patients previously treated with alkylating agents (Chan et al, 1999). Owing to its activity and to the lack of cross-resistance with anthracyclines, there is a strong rationale for combining docetaxel with anthracyclines. The anthracycline-taxane regimens can now be considered the most effective regimens in metastatic breast cancer (MBC) and a first-line therapy of choice in this set of patients (Valero and Hortobagyi, 2003). In particular, many reports have described the combined use of docetaxel and epirubicin, an anthracycline less cardiotoxic than doxorubicin, with the objective to find the safest and most efficient way to integrate these classes of drugs (Mavroudis et al, 2000; Pagani et al, 2000). However, whether an anthracycline-taxane regimen is worthy as first-line treatment for MBC patients pretreated with adjuvant or neoadjuvant anthracyclines is an open question, not definitely assessed by appropriate prospective trials. Therefore, we planned a randomised phase III trial to compare epirubicin and docetaxel vs docetaxel alone for efficacy and safety as first-line chemotherapy of MBC patients pretreated with epirubicin in adjuvant or neoadjuvant setting.
Materials and methods
Eligibility criteria were: women with MBC⩽65 years; no previous chemotherapy for metastatic disease; measurable disease; Eastern Cooperative Oncology Group (ECOG) performance status of 0–2; previous adjuvant or neoadjuvant chemotherapy with anthracyclines, up to a total dose of doxorubicin ⩽250 mg m−2 or epirubicin ⩽500 mg m−2, completed at least 12 months before enrollment; absence of brain metastases; adequate bone marrow, renal and liver function; left ventricular ejection fraction (LVEF) ⩾50%. Previous adjuvant endocrine therapy as well as endocrine therapy for metastatic disease were allowed. Patients were excluded if they had received taxanes as adjuvant chemotherapy or had history of serious medical conditions potentially compromising study participation. Pregnant or lactating women were ineligible. All patients were required to provide written informed consent and the protocol was approved by the Independent Ethical Committee of the National Cancer Institute of Naples.
Patients were randomly assigned to docetaxel 100 mg m−2 (Arm D) or to epirubicin 75 mg m−2 and docetaxel 80 mg m−2 (Arm ED) on day 1, every 3 weeks for six cycles of chemotherapy, unless disease progression or unacceptable toxicity. Prednisone and a prophylactic antiemetic regimen with 5-HT3 antagonists were given from the first infusion. No dose reduction of chemotherapy was planned by protocol. Treatment was delayed for 1 week for grade ⩾2 neutropenia and/or grade ⩾1 thrombocytopenia. Granulocyte colony-stimulating factor (G-CSF) was administered at 5 mcg kg day−1 subcutaneously in case of grade 4 neutropenia until neutrophil count >2000 mm−3.
Pretreatment evaluation, performed within 1 month before randomisation, included physical examination, laboratory studies, ECG, echocardiography with LVEF, brain, chest and abdomen computed tomography, bone scan, skeletal radiographs (if required). Echocardiography and evaluation of tumour response, according to Response evaluation criteria in solid tumor (RECIST) guidelines, were performed every three cycles.
Toxicity was evaluated according to National Cancer Institute Common Toxicity Criteria version 2.0. For each type of toxicity, the worst degree experienced throughout the treatment was computed for each patient.
The study was designed as a single centre randomised phase III study with response rate as primary end point. Stratification factors were: performance status (0 vs 1 vs 2), disease-free survival (<24 months vs >24 months) and type of dominant metastatic site (soft tissue vs bone vs viscera). Primary objective was to evaluate the objective response rate (ORR) of docetaxel and epirubicin compared with docetaxel alone. Secondary end points included toxicity, progression-free survival (PFS) and overall survival. Calculation of sample size was based on a 40% expected response rate with docetaxel alone, a 60% auspicated response rate with the combination of docetaxel and doxorubicin, a 20% of risk of false negative and a 5% of risk of false positive result, and a one-tailed χ2 test. With these requirements, planned sample size was 77 patients for each arm of treatment. Continuous and ordinal categorical data were compared by exact Wilcoxon rank sum test. Dichotomous data were compared by Fisher's exact test. Progression-free and overall survival curves were drawn according to Kaplan–Meier and statistical significance of differences was tested by the log-rank test. As the study was interrupted earlier than planned, the Bayesian predictive probability that the response rate of the ED group would be statistically better than that of the D group, if the trial were continued to the planned end, was calculated to corroborate the meaning of findings (Johns and Andersen, 1999).
Results
From May 2000 to October 2003, 51 patients were enrolled. The recruitment was slower than expected, due to the restrictive inclusion criteria of the protocol and prompted us to stop the study, after 3.5 years, because time needed to reach the planned sample size would have been too long. Baseline characteristics of the patients were well balanced between the two arms (Table 1).
The median number of administered cycles was six (range 2–6); 81 and 76% of patients received all the planned therapy (six cycles) in the ED and D treatment arms, respectively. Median average relative dose intensity of treatment was similar in the two groups, while G-CSF was used far more frequently in ED group; 77% of ED subjects, indeed, used G-CSF in at least one cycle compared with 56% of D patients (P=0.0582).
All the responses were independently validated. Both therapeutic regimens showed similar antitumour activity (Table 2). The ORR was 72% (18 patients; 95% exact CI: 51–88) in the ED arm and 79% (19 patients; 95% exact CI: 58–93) in the D arm (one-tailed P=0.8196). Based on these results, the probability that the response rate of the ED group would be significantly better than that of the D group, if the trial were brought to its completion, is equal to 0.0334.
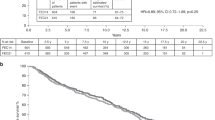
After 45 (88%) events, the median progression-free survival was 9 months in the ED and 11 months in the D arm (one-tailed P=0.6998). With regard to overall survival, 30 events (15 in each arm) were reported after a 30 months median follow-up of alive patients. The median overall survival was 18 months in the ED and 21 months in the D arm (one-tailed P=0.6406). Progression-free and overall survival curves are reported in Figure 1.
Haematological and nonhaematological toxicities are summarised in Table 3. Leucopaenia, the most frequent haematological toxicity, was significantly more severe in the ED arm (P=0.0290). Among nonhaematological toxicities, nausea and stomatitis were significantly worse in the ED arm (P=0.0210 and P=0.0499, respectively). No significant differences between the arms were found in other nonhaematological toxicities. Grade 1 cardiac toxicity was reported in 19 and 16% of patients, with ED and D, respectively (P=0.9999).
Discussion
Our phase III study indicates that the addition of epirubicin to docetaxel did not improve outcomes as compared to single-agent docetaxel, in the first-line treatment of metastatic breast cancer patients, who already had received adjuvant epirubicin. Both therapeutic regimens showed similar antitumour activity, and no significant differences were found between the two treatments in progression-free survival and overall survival. Of course, we are aware that the small sample size and the fact that enrollment was stopped before than planned are major limitations of our study. However, our results are strengthened by the finding that the Bayesian predictive probability that the study hypothesis (that ED could increase by a 20% the response rate as compared with D alone) could be eventually demonstrated if the study had reached the planned sample size is definitely low (only 3.3%). To the best of our knowledge, there is no randomised study addressing the role of anthracyclines in the treatment of patients relapsing after anthracycline-based adjuvant chemotherapy. Retrospective studies, indirectly addressing this issue, have produced conflicting results. Chauvin et al (1990) demonstrated a low activity of the CEF regimen in patients previously treated with anthracycline-based adjuvant chemotherapy. Other authors (Venturini et al, 1996; Pierga et al, 2001) found that previous adjuvant chemotherapy could adversely affect the prognosis of MBC patients treated with an anthracycline-based first-line chemotherapy, but this effect was independent of whether adjuvant chemotherapy was CMF- or anthracycline-based. On the contrary, other studies (Buzdar et al, 1981; Valagussa et al, 1986; Kardinal et al, 1988; Gennari et al, 2004) did not demonstrate a poorer outcome in metastatic breast cancer patients previously treated with adjuvant chemotherapy. Namely, Gennari et al (2004) did not find any negative influence of adjuvant anthracyclines on the activity of first-line epirubicin and paclitaxel, confirming that modern chemotherapy regimens, including anthracyclines and taxanes, provide satisfactory results in metastatic breast cancer patients, regardless of previous adjuvant chemotherapy.
In conclusion, the results of our trial support that epirubicin should not be included in taxanes-containing regimens for breast cancer patients relapsed after an anthracycline-based adjuvant or neoadjuvant therapy, also taking into account the availability for these patients of new active, non-cross-resistant drugs.
Conflict of interest
We declare no conflicts of interest.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Buzdar AU, Legha SS, Hortobagyi GN, Yap HY, Wiseman CL, Distefano A, Schell FC, Barnes BC, Campos LT, Blumenschein GR (1981) Management of breast cancer patients failing adjuvant chemotherapy with adriamycin-containing regimens. Cancer 47: 2798–2802
Chan S, Friedrichs K, Noel D, Pinter T, Van Belle S, Vorobiof D, Duarte R, Gil Gil M, Bodrogi I, Murray E, Yelle L, von Minckwitz G, Korec S, Simmonds P, Buzzi F, Gonzalez Mancha R, Richardson G, Walpole E, Ronzoni M, Murawsky M, Alakl M, Riva A, Crown J, 303 Study Group (1999) Prospective randomized trial of docetaxel vs doxorubicin in patients with metastatic breast cancer. J Clin Oncol 17: 2341–2354
Chauvin F, Magnet M, Lasset C, Catimel G, Mayer M, Chevarier P, Jacquin JP, Peaud P, Clavel M (1990) Prognostic factors in the response of a first line chemotherapy in advanced breast cancer. Bull Cancer 77: 941–947
Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) (2005) Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet 365: 1687–1717
Fossati R, Confalonieri C, Torri V, Ghislandi E, Penna A, Pistotti V, Tinazzi A, Liberati A (1998) Cytotoxic and hormonal treatment for metastatic breast cancer: a systematic review of published randomised trials involving 31 150 women. J Clin Oncol 16: 3439–3460
Gennari A, Bruzzi P, Orlandini C, Salvadori B, Donati S, Landucci E, Guarneri V, Rondini M, Ricci S, Conte P (2004) Activity of first-line epirubicin and paclitaxel in metastatic breast cancer is independent of type of adjuvant therapy. Br J Cancer 90: 962–967
Johns D, Andersen JS (1999) Use of predictive probabilities in phase II and phase III clinical trials. J Biopharm Stat 9: 67–79
Kardinal CG, Perry MC, Korzun AH, Rice MA, Ginsberg S, Wood WC (1988) Responses to chemotherapy or chemohormonal therapy in advanced breast cancer patients treated previously with adjuvant chemotherapy. Cancer 61: 415–419
Mavroudis D, Alexopoulos A, Ziras N, Malamos N, Kouroussis C, Kakolyris S, Agelaki S, Kalbakis K, Tsavaris N, Potamianou A, Rigatos G, Georgoulias V (2000) Front-line treatment of advanced breast cancer with docetaxel and epirubicin: a multicenter phase II study. Ann Oncol 11: 1249–1254
Nabholtz J-M, Senn HJ, Bezwoda WR, Melnychuk D, Deschênes L, Douma J, Vandenberg TA, Rapoport B, Rosso R, Trillet-Lenoir V, Drbal J, Molino A, Nortier JWR, Richel DJ, Nagykalnai T, Siedlecki P, Wilking N, Genot JY, Hupperets PSGJ, Pannuti F, Skarlos D, Tomiak EM, Murawsky M, Alakl M, Riva A, Aapro M, 304 Study Group (1999) Prospective randomized trial of docetaxel vs mitomycin plus vinblastine in patients with metastatic breast cancer progressing despite previous anthracycline-containing chemotherapy. J Clin Oncol 17: 1413–1424
Pagani O, Sessa C, Nole F, Crivellari D, Lombardi D, Thurlimann B, Hess D, Borner M, Bauer J, Martinelli G, Graffeo R, Zucchetti M, D’Incalci M, Goldhirsch A (2000) Epidoxorubicin and docetaxel as first-line chemotherapy in patients with advanced breast cancer: a multicentric phase I-II study. Ann Oncol 11: 985–991
Pierga JY, Asselain B, Jouve M, Dieras V, Carton M, Laurence V, Girre V, Beuzeboc P, Palangie T, Dorval T, Pouillart P (2001) Effect of adjuvant chemotherapy on outcome in patients with metastatic breast carcinoma treated with first-line doxorubicin-containing chemotherapy. Cancer 91: 1079–1089
Valagussa P, Tancini G, Bonadonna G (1986) Salvage treatment of patients suffering relapse after adjuvant CMF chemotherapy. Cancer 58: 1411–1417
Valero V, Hortobagyi GN (2003) Are anthracycline-taxane regimens the new standard of care in the treatment of metastatic breast cancer? J Clin Oncol 21: 959–962
Venturini M, Bruzzi P, Del Mastro L, Garrone O, Bertelli G, Guelfi M, Pastorino S, Rosso R, Sertoli MR (1996) Effect of adjuvant chemotherapy with or without anthracyclines on the activity and efficacy of first-line cyclophosphamide, epidoxorubicin, and fluorouracil in patients with metastatic breast cancer. J Clin Oncol 14: 764–773
Acknowledgements
The authors thank all the patients enrolled in the study. Federika Crudele, Fiorella Romano, Giuliana Canzanella and Giovanni de Matteis for data management.
Clinical Trials Unit, Medical Oncology C, Cell Biology and Preclinical Models (National Cancer Institute) and Medical Statistics (Second University) are supported by Associazione Italiana per la Ricerca sul Cancro (AIRC), with grants not affecting collection, analysis and interpretation of data reported in the paper.
Author information
Authors and Affiliations
Consortia
Corresponding author
Appendix A1
Appendix A1
Members of the NCI-Naples Breast Cancer Group who contributed to this manuscript:
Cell Biology and Preclinical Models Unit: Nicola Normanno, Antonella De Luca, Monica Rosaria Maiello, Adele Carotenuto.
Clinical Trials Unit: Francesco Perrone, Alessandro Morabito, Ermelinda De Maio, Massimo Di Maio, Roberta D’Aniello, Gianfranco De Feo.
Medical Oncology C: Andrea de Matteis, Francesca Di Rella, Adriano Gravina, Vincenzo Labonia, Gabriella Landi, Francesco Nuzzo, Carmen Pacilio, Emanuela Rossi.
Nuclear Medicine: Secondo Lastoria, Aldo Bartiromo.
Pathology: Gerardo Botti, Maurizio Di Bonito, Franca La Vecchia, Maria Staiano, Franca Formichelli, Maria Pia Curcio.
Pharmacy: Maria Rosaria Salzano.
Radiotherapy: Brunello Morrica.
Senology: Giuseppe D’Aiuto, Franca Avino, Immacolata Capasso, Claudio Longo, Michele Pizzorusso, Massimo Rinaldo, Renato Thomas.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Pacilio, C., Morabito, A., Nuzzo, F. et al. Is epirubicin effective in first-line chemotherapy of metastatic breast cancer (MBC) after an epirubicin-containing adjuvant treatment? A single centre phase III trial. Br J Cancer 94, 1233–1236 (2006). https://doi.org/10.1038/sj.bjc.6603096
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6603096
Keywords
This article is cited by
-
Pharmacoethnicity of docetaxel-induced severe neutropenia: integrated analysis of published phase II and III trials
International Journal of Clinical Oncology (2013)
-
Capecitabine plus paclitaxel versus epirubicin plus paclitaxel as first-line treatment for metastatic breast cancer: efficacy and safety results of a randomized, phase III trial by the AGO Breast Cancer Study Group
Breast Cancer Research and Treatment (2013)
-
Meta-analysis of phase III trials of docetaxel alone or in combination with chemotherapy in metastatic breast cancer
Journal of Cancer Research and Clinical Oncology (2012)
-
Filling in the gaps: reporting of concurrent supportive care therapies in breast cancer chemotherapy trials
Supportive Care in Cancer (2011)
-
Rechallenging with anthracyclines and taxanes in metastatic breast cancer
Nature Reviews Clinical Oncology (2010)