Abstract
HER-2 overexpression is associated to a poor prognosis in high-risk and metastatic breast cancer (MBC) patients treated with high-dose chemotherapy (HDC). HER-2 status is also a predictive factor and when trastuzumab is administered in combination with or sequentially to chemotherapy, a significant disease-free and/or overall survival improvement has been observed in HER-2+ early and MBC. Unfortunately, in both settings, trastuzumab is associated with an increased risk of cardiac dysfunction (CD). We have reviewed the clinical charts of HER-2-overexpressing MBC patients treated with trastuzumab after HDC. Age, baseline left ventricular ejection fraction (LVEF), radiation therapy on cardiac area, exposure to anthracycline, single or multiple transplant, high-dose agents, trastuzumab treatment duration were recorded as potential risk factors. In total, 53 patients have been included in the analysis. Median LVEF at baseline was 60.5%; at the end of trastuzumab (data available for 28 patients only), it was 55% (P=0.01). Five out of the 28 (17.9%) patients experienced CD. Two out of 53 (3.8%) patients developed a congestive heart failure. Age ⩾50 years and multiple transplant procedure were potential risk factors for CD. The overall incidence of CD observed in this population of HER-2+ MBC patients treated with trastuzumab after HDC is not superior to that reported with concomitant trastuzumab and anthracyclines. However, patients with age ⩾50 years or receiving multiple course of HDC should be considered at risk for CD.
Similar content being viewed by others
Main
High-dose chemotherapy with autologous hemopoietic progenitor support has been compared to standard dose chemotherapy in high-risk early breast cancer as well as in metastatic disease. In high-risk breast cancer, there are negative trials showing no superiority for high-dose chemotherapy (Bergh et al, 2000; Hortobagyi et al, 2000; Tallman et al, 2003); in contrast, other trials have shown significant improvement in relapse-free and overall survival (Roche et al, 2003; Rodenhuis et al, 2003; Nitz et al, 2005). In metastatic breast cancer, whereas some trials have failed to demonstrate a survival benefit, others have suggested an advantage in event-free survival in favour of high-dose treatment (Stadtmauer et al, 2000; Crown et al, 2004; Lotz et al, 2005; Schmid et al, 2005). In spite of these conflicting results, it is however clear that, at present, high-dose chemotherapy cannot be considered standard treatment for any breast cancer patient. On the other side, longer follow-up of the randomized trials and a meta-analysis of their pooled data might confirm a limited advantage; moreover, because of the reduced treatment-related mortality and availability of new anticancer drugs, this treatment modality could still represent a field of research for some subsets of patients.
It is now clear that breast cancer represents a very heterogeneous disease and, from a clinical stand point, at least three breast cancer subtypes must be recognized: hormone-receptor positive, HER-2 positive and triple negative. In particular, overexpression of HER-2 oncogene occurs in 20–30% of the patients with invasive breast cancer and is associated with poor prognosis and decreased overall survival (Slamon et al, 1987). Retrospective studies have shown that HER-2 overexpression is an independent poor predictive factor of outcome after high-dose chemotherapy both in high-risk and metastatic breast cancer (Bitran et al, 1996; Kim et al, 2001; Nieto et al, 2002; Guarneri et al, 2004). Moreover, Rodenhuis et al (2003) in the National Duch trial of high-dose chemotherapy in high-risk breast cancer have reported an unplanned subset analysis based on HER-2 status suggesting that the improvement of relapse-free survival of high-dose chemotherapy in patients with stage II and III breast cancer and 10 or more axillary nodes may be confined to patients with HER-2-negative tumours. A part from its possible prognostic and predictive role, the HER-2 status determines the choice of treatment: when trastuzumab, a humanised monoclonal antibody that selectively binds to the extracellular domain of the HER-2 protein, is used in combination with chemotherapy, response rate, time to progression and median overall survival are improved (Slamon et al, 2001; Marty et al, 2005). Unfortunately, Trastuzumab was unexpectedly found to be associated with an increased risk of cardiac dysfunctions and asymptomatic decrease in left ventricular ejection fraction (LVEF); this risk was especially high in patient receiving concurrent anthracyclines, older than 50 years or with decreased LVEF after anthracyclines (Seidman et al, 2002; Perez and Rodeheffer, 2004; Tan-Chiu et al, 2005).
In order to estimate the cardiac tolerability of trastuzumab after high-dose chemotherapy, we have retrospective analysed the clinical files of HER-2-positive breast cancer patients treated with high-dose chemotherapy in the Italian Centers of the GITMO group (Gruppo Italiano Trapianto Midollo Osseo).
Patients and methods
A questionnaire was sent to 11 major Italian centres. The following information were requested: histology, hormonal receptor status, HER-2 status (IHC or, if available, FISH status), radiation therapy on cardiac area, previous chemotherapy with regimes including anthracycline and paclitaxel, cumulative dose of anthracycline, use of cardioprotective agents, status of disease at the time of high-dose chemotherapy procedure, single or multiple transplant procedure, dose of cyclophosphamide >4 g m−2 and mitoxantrone >60 mg m−2, status of disease after transplant, dose and schedule of trastuzumab, cytotoxic agents associated with trastuzumab, LVEF before starting trastuzumab and at the end of treatment, any episode of congestive heart failure (CHF). Cardiac dysfunction was defined as (1) a decline of LVEF ⩾10% to below 50%, (2) a decline of LVEF between 5 and 9% to below 50% with symptomatic (NYHA class III–IV) CHF, (3) any symptomatic (NYHA class III–IV) CHF event. Any one of the three criteria was sufficient to confirm a diagnosis of cardiac dysfunction.
Statistical analysis
The Wilcoxon matched-pairs signed-ranks test was used to determine if the distribution of the LVEF at baseline and at the end of treatment was the same. Time to suspension and time to cardiac event were calculated using the Kaplan–Meier method. Time to suspension was calculated from the date of beginning of the treatment with trastuzumab until the suspension or last follow-up. Time to cardiac event was calculated from the date of beginning of the treatment with trastuzumab until the date of the cardiac event or last follow-up. The log-rank test was used to compare the curves of time to cardiac event. The hazard ratio and the 95% CI was calculated. The level of significance was set to be 0.05. The statistical software used for the analysis was STATA/SE version 8.0.
Results
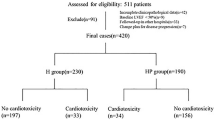
All the centres returned the questionnaire and we could collect data from 53 patients treated with trastuzumab for metastatic disease between February 1999 and June 2005.
Patients characteristics are shown in Table 1. Median age was 47 years (range 29–66). Histology type was ductal carcinoma in 85% of the patients; hormone receptor status was positive in 44.2% of the patients. HER-2 expression was scored by immunohistochemistry method as 3+ in 49 patients and as 2+ in four patients; in the 2+ patients, HER-2 amplification was confirmed by FISH. A total of 44 patients (83%) had received treatment with anthracycline/paclitaxel-containing regimens and 16 patients (30%) had received radiation therapy on cardiac area. Median cumulative doses of doxorubicin or epidoxorubicin were 266 mg m−2 (range 60–500) and 395 mg m−2 (range 120–660), respectively. High-dose chemotherapy was administered as adjuvant treatment to 17 patients, for locally advanced disease to three patients and for metastatic disease to 33 patients. A total of 21 patients received a single course of high-dose chemotherapy and 32 patients a double course of high-dose chemotherapy. High-dose therapy included melphalan–thiotepa in 27 patients (50.9%), mitoxantrone–melphalan in 14 patients (26.4%), mitoxantrone–thiotepa in six patients (11.3%), mitoxantrone–melphalan–thiotepa in three patients (5.7%); three patients (5.7%) received other regimens. Median interval between high-dose chemotherapy and the beginning of trastuzumab was 6 months (range 0–90). Trastuzumab was administered at weekly or 3-weekly schedule in 33 and 20 patients, respectively. Trastuzumab was given as single agent in 17 patients, in combination with paclitaxel in 21 patients, and with vinorelbine in 15 patients. Median duration of treatment with trastuzumab was 11 months (1–46) with 32 patients receiving trastuzumab for more than 12 months. At the time of analysis, 41 patients have stopped the treatment with trastuzumab: seven for cardiac toxicity, 29 for progression of disease, four for patient's decision, one patient died early after the administration of trastuzumab; 12 patients are still on treatment.
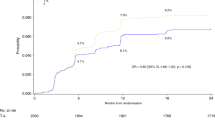
Cardiac dysfunction
Baseline LVEF was available for all patients; LVEF at the end of treatment was available for 28 patients and 13 patients had also a third measurement of LVEF. Median LVEF values at baseline and at the end of trastuzumab were 60.5% (43–72) and 55% (25–72), respectively (Figure 1); this difference resulted statistically significant with a P-value of 0.01. At the end of treatment with trastuzumab, seven patients (25%) had a reduction of LVEF to less than 50%. In this group of patients, one patient had a decline of LVEF of 3% without cardiac symptoms, one patients had a reduction of LVEF of 7% and developed mild cardiac symptoms classified as NYHA class II, five patients had a decline of LVEF ⩾10% and two of these developed congestive heart failure classified as NYHA class III. According to our definition, five out of 28 patients with evaluable LVEF experienced a cardiac event (17.9%).
On the entire group of patients, two out of 53 (3.8%) developed a congestive heart failure (NYHA class III). Both patients had a decline of LVEF >10% to below 50%. These two patients started trastuzumab within 2 months from high-dose chemotherapy and the duration of treatment with trastuzumab was 18 and 46 months, respectively. One of these two patients had previously received doxorubicin (cumulative dose of 300 mg m−2).
Trastuzumab was discontinued in seven patients with a LVEF<50%. Follow-up data for cardiac function recovery are available for four patients only: all these patients recovered a normal LVEF at a median interval of 11 months (range 3–19).
Analysis of risk factors
The incidence of cardiac dysfunction was analysed according to risk factors including age, baseline LVEF, previous radiation therapy on cardiac area, single vs multiple transplant, dose of cyclophosphamide and mitoxantrone, previous anthracycline exposure and duration of treatment with Trastuzumab (Table 2). Age ⩾50 years was the only factor significantly associated with cardiac dysfunction (P: 0.027). Moreover, we have analysed risk factors associated with a significant decline of LVEF at the end of treatment with trastuzumab (Table 3). Age ⩾50 years and multiple courses of high-dose chemotherapy were associated with a 13% reduction in LVEF (P=0.02) and a 4% reduction in LVEF (P=0.02), respectively.
Baseline LVEF<55%, previous treatment with anthracicline/paclitaxel, high-dose of cyclophospamide alone or in combination with high-dose mitoxantrone and duration of treatment with trastuzumab >12 months were not associated with a significant reduction of LVEF. Previous radiation therapy on cardiac area was associated with a 4% reduction of LVEF, but this value did not reach the statistical significance (0.08).
Discussion
Several studies have shown that high-dose chemotherapy is not able to modify the poorer prognosis of HER-2-positive breast cancer patients (Slamon et al, 1987; Bitran et al, 1996; Nieto et al, 2002; Rodenhuis et al, 2003; Guarneri et al, 2004). It is therefore clear that these patients should be treated with trastuzumab. Unfortunately, very few data on the cardiac tolerability of trastuzumab after high-dose chemotherapy are available.
A retrospective analysis on 1219 patients treated for metastatic disease with standard chemotherapy with or without trastuzumab in seven phase II and III clinical trials showed symptomatic cardiac dysfunction (NYHA class III–IV) in 2–16% of patients who received trastuzumab. The incidence was 2–4% for patients receiving first-line trastuzumab as single agent or in combination with paclitaxel, while it increased to 16% for patients receiving trastuzumab plus doxorubicin–cyclophosphamide combination. The overall cardiac dysfunction rate was 13 and 27% for patients receiving trastuzumab plus paclitaxel or trastuzumab plus doxorubicin–cyclophosphamide (AC) combination, respectively. Analysis of potential risk factors for cardiac dysfunction in patients with metastatic breast cancer treated with standard-dose chemotherapy plus trastuzumab has demonstrated that increasing age and the association of trastuzumab plus anthracycline was a statistically significant predictive factor. Other factors such as prior radiotherapy, and mean cumulative dose of doxorubicin were not found to be independent predictive factors of cardiac dysfunction (Seidman et al, 2002). Moreover, Perez and Rodeheffer (2004) reviewed data from new prospective clinical trials reporting lower incidence of trastuzumab-related cardiac toxicity when more stringent patient selection and cardiac monitoring criteria were adopted. More recently, Tan-Chiu et al (2005) reported data on cardiac dysfunction associated to herceptin in combination with paclitaxel following AC regimen in high-risk breast cancer. The incidence of CHF was 4.1%. Age ⩾50 years and baseline LVEF<55% were found as risk factors significantly associated with CHF.
Cardiotoxicity is also a major concern in the treatment with high-dose chemotherapy. Risk factors for cardiotoxicity include high-dose cyclophosphamide, high-dose mitoxantrone and previous radiation therapy on cardiac area (Morandi et al, 2005). Several studies failed to demonstrated a relationship between previous anthracycline exposure and development of cardiac toxicity following high-dose chemotherapy (Nieto et al, 2000; Petros et al, 2002). However, we and others have reported that high-dose alkylating agents in metastatic breast cancer patients previously exposed to cumulative dose of epirubicin ⩾450 mg m−2 is associated with a 4–5% of congestive heart failure rate (Alidina et al, 1999; Gennari et al, 1999; Bengala et al, 2001). Moreover, we have shown that a double course of high-dose chemotherapy after anthracycline-containing regimen in patients of metastatic breast cancer can induce a transient decline of LVEF to less than 50% in 14.3% of the patients (Bengala et al, 2003).
Our retrospective analysis shows that median LVEF is significantly lower after trastuzumab in patients previously treated with high-dose chemotherapy; moreover, in these patients, cardiac dysfunction rate and symptomatic cardiac failure (NYHA class III) rate were 17.9 and 3.8%, respectively. The incidence of CD was higher than that reported with trastuzumab as single agent or in combination with paclitaxel but not superior to that observed with trastuzumab administered concomitantly with anthracyclines. Age >50 years and multiple transplant procedures have been the only factors associated with an increased risk of cardiotoxicity. Interestingly, 83% of our patients had received anthracycline–taxane chemotherapy, another potentially cardiotoxic regimen, before HD treatment; moreover, duration of trastuzumab treatment was relatively long (median 11 months), with 32 patients treated for more than 1 year.
Nieto et al (2004) and Goncalves et al (2005) have prospectively studied the feasibility of the concurrent administration of trastuzumab with alkylator-based high-dose chemotherapy in breast cancer. End points of the studies were safety and pharmacokinetic profile evaluation. Trastuzumab was administered for a median of 9 weeks (range 9–48) and 15 weeks (range 1–39) in the two trials with no apparent increased toxicity and in particular cardiac dysfunction.
In conclusion, our retrospective analysis shows that the administration of trastuzumab after high-dose chemotherapy is feasible with an incidence of cardiac dysfunction and symptomatic cardiac failure not superior to that reported with trastuzumab in combination with anthracyclines. Age ⩾50 years, multiple courses of high-dose chemotherapy and prior radiation therapy on cardiac area are risk factors for cardiac dysfunction in this patient population.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Alidina A, Lawrence D, Ford LA, Baer MR, Bambach B, Bernstein SH, Czuzman MS, Slack JL, Spangenthal E, Wetzler M, Barcos MP, Proulx GM, Anderson B, McCarthy Jr PL (1999) Thiotepa-associated cardiomiopathy during blood or marrow transplantation: association with the female sex and cardiac risk factors. Biol Blood Marrow Transplant 5: 322–327
Bengala C, Danesi R, Guarneri V, Pazzagli I, Donati S, Favre C, Fogli S, Biadi O, Innocenti F, Del Tacca M, Mariani M, Conte PF (2003) High-dose consolidation chemotherapy with idarubicin and alkylating agents following induction with gemcitabine–epirubicin–paclitaxel in metastatic breast cancer: a dose finding study. Bone Marrow Transplant 31: 275–280
Bengala C, Pazzagli I, Innocenti F, Donati S, Favre C, Menconi MC, Greco F, Danesi R, Orlandini C, Guarneri V, Del Tacca M, Conte PF (2001) High-dose thiotepa and melphalan with hempoietic progenitor support following induction therapy with epirubicin–paclitaxel–containing regimens in metastatic breast cancer (MBC). Ann Oncol 12: 69–74
Bergh J, Wiklund T, Erikstein B, Lidbrink E, Lindman H, Malmstrom P, Kellokumpu-Lehtinen P, Bengtsson NO, Soderlund G, Anker G, Wist E, Ottosson S, Salminen E, Ljungman P, Holte H, Nilsson J, Blomqvist C, Wilking N (2000) Tailored fluorouracil, epirubicin and cyclophosphamide compared with marrow-supported high-dose chemotherapy as adjuvant treatment for high-risk breast cancer: a randomized trial of Scandinavian Breast Group 9401 study. Lancet 356: 1384–1391
Bitran JD, Samuels B, Trujillo Y, Klein L, Schroeder L, Martinec J (1996) Her2/neu overxpression is associated with treatment failure in women with high-risk stage II and stage IIIA breast cancer (>10 involved lymph nodes) treated with high-dose chemotherapy and autologous hematopoietic progenitor cell support following standard-dose adjuvant chemotherapy. Clin Cancer Res 2: 1509–1513
Crown JP, Leyvraz S, Verrill M, Guillem V, Efremidis A, Garcia-Conde Bru J, Welch R, Montes A, Leonard R, Baselga J (2004) Effect of tandem high-dose chemotherapy on long-term complete remission in metastatic breast cancer compared to conventional dose in patients who were not selected on basis of response to prior chemotherapy: mature results of the IBDIS-1. Proc Am Soc Clin Oncol 23: 34 (Abstr. 631).
Gennari A, Salvadori B, Donati S, Bengala C, Orlandini C, Danesi R, Del Tacca M, Bruzzi P, Conte PF (1999) Cardiotoxicity of epirubicin/paclitaxel-containing regimens: role of cardiac risk factors. J Clin Oncol 17: 3596–3602
Goncalves A, Braud AC, Viret F, Tarpin C, Charaffe-Jauffret E, Jacquemier J, Maraninchi D, Viens P (2005) High-dose alkylating agents with autologous hematopoietic stem cell support and trastuzumab in ERBB2 overxpressing metastatic breast cancer: a feasibility study. Anticancer Res 25: 663–668
Guarneri V, Bengala C, Orlandini C, Gennari A, Donati S, Campani D, Collecchi P, Maur M, Conte PF (2004) HER2 overxpression as prognostic factor in metastatic breast cancer patients treated with high-dose chemotherapy and autologous stem cell support. Bone Marrow Transplant 34: 413–417
Hortobagyi GN, Buzdar AU, Theriault RL, Valero V, Frye D, Booser DJ, Holmes FA, Giralt S, Khouri I, Andersson B, Gajewski JL, Rondon G, Smith TL, Singletary SE, Ames FC, Sneige N, Strom EA, McNeese MD, Deisseroth AB, Champlin RE (2000) Randomized trial of high-dose chemotherapy and blood cell autografts for high-risk primary breast carcinoma. J Natl Cancer Inst 92: 225–233
Kim YS, Konoplev SN, Montemurro F, Hoy E, Smith TL, Rondon G, Champlin RE, Sahin AA, Ueno NT (2001) HER2 overxpression as poor prognostic factor for patients with metastatic breast cancer undergoing high-dose chemotherapy with autologous stem cell transplantation. Clin Cancer Res 7: 4008–4012
Lotz JP, Cure H, Janvier M, Asselain B, Morvan F, Legros M, Audhuy B, Biron P, Guillemot M, Goubet J, Laadem A, Cailliot C, Maignan CL, Delozier T, Glaisner S, Maraninchi D, Roche H, Gisselbrecht C (2005) High-dose chemotherapy with haematopoietic stem cell transplantation for metastatic breast cancer patients: final results of the French multicentric randomized CMA/PEGASE 04 protocol. Eur J Cancer 41: 71–80
Marty M, Cognetti F, Maraninchi D, Snyder R, Mauriac L, Tubiana-Hulin M, Chan S, Grimes D, Anton A, Lluch A, Kennedy J, O'Byrne K, Conte P, Green M, Ward C, Mayne K, Extra JM (2005) Randomized phase II trial of the efficacy and safety of trastuzumab combined with docetaxel in patient with human epidermal growth factor receptor 2-positive metastatic breast cancer administered as first-line treatment: the M77001 Study Group. J Clin Oncol 23: 4265–4274
Morandi P, Ruffini PA, Benvenuto GM, Raimondi R, Fosser V (2005) Cardiac toxicity of high-dose chemotherapy. Bone Marrow Transplant 35: 323–334
Nieto Y, Cagnoni PJ, Bearman SI, Shpall EJ, Matthes S, Jones RB (2000) Cardiac toxicity following high-dose cyclophosphamide, cisplatin and BCNU (STAMP-I) for breast cancer. Biol Blood Marrow Transplant 6: 198–203
Nieto Y, Nawaz S, Jones RB, Shpall EJ, Cagnoni PJ, McSweeney PA, Baron A, Razook C, Matthes S, Bearman SI (2002) Prognostic model for relapse after high-dose chemotherapy with autologous stem-cell transplantation for stage IV oligometastatic breast cancer. J Clin Oncol 20: 707–718
Nieto Y, Vredenburgh JJ, Shpall EJ, Bearman SI, McSweeney PA, Chao N, Rizzieri D, Gasparetto C, Matthes S, Baron AE, Jones RB (2004) Phase II feasibility and pharmacokinetic study of concurrent administration of trastuzumab study of concurrent administration of trastuzumab and high-dose chemotherapy in advanced HER2+ breast cancer. Clin Cancer Res 10: 7136–7143
Nitz UA, Mohrmann S, Fischer J, Lindemann W, Berdel WE, Jackisch C, Werner C, Ziske C, Kirchner H, Metzner B, Souchon R, Ruffert U, Schutt G, Pollmanns A, Schmoll HJ, Middecke C, Baltzer J, Schrader I, Wiebringhaus H, Ko Y, Rosel S, Schwenzer T, Wernet P, Hinke A, Bender HG, Frick M, West German Study Group (2005) Comparison of rapidly cycled tandem high-dose chemotherapy plus peripheral-blood stem-cell support versus dose-dense conventional chemotherapy for adjuvant treatment of high-risk breast cancer: results of a multicentre phase III trial. Lancet 366: 1935–1944
Perez EA, Rodeheffer R (2004) Clinical cardiac tolerability of trastuzumab. J Clin Oncol 22: 322–329
Petros WP, Broadwater G, Berry D, Jones RB, Vredenburgh JJ, Gilbert CJ, Gibbs JP, Colvin OM, Peters WP (2002) Association of high-dose cyclophosphamide, cisplatin and carmustine pharmacokinetics with survival, toxicity and dosing weight in patients with primary breast cancer. Clin Cancer Res 8: 698–705
Roche H, Viens P, Biron P, Lotz JP, Asselain B, PEGASE Group (2003) High-dose chemotherapy for breast cancer: the French PEGASE experience. Cancer Control 10: 42–47
Rodenhuis S, Bontenbal M, Beex LV, Wagstaff J, Richel DJ, Nooij MA, Voest EE, Hupperets P, van Tinteren H, Peterse HL, TenVergert EM, de Vries EG, Netherlands Working Party on Autologous Transplantation in Solid Tumors (2003) High-dose chemotherapy with hematopoietic stem-cell rescue for high-risk breast cancer. N Engl J Med 349: 7–16
Schmid P, Schippinger W, Nitsch T, Huebner G, Heilmann V, Schultze W, Hausmaninger H, Wischnewsky M, Possinger K (2005) Up-front tandem high-dose chemotherapy compared with standard chemotherapy with doxorubicin and paclitaxel in metastatic breast cancer: results of a randomized trial. J Clin Oncol 23: 432–440
Seidman A, Hudis C, Pierri MK, Shak S, Paton V, Ashby M, Murphy M, Stewart SJ, Keefe D (2002) Cardiac dysfunction in the trastuzumab clinical trials experience. J Clin Oncol 20: 1215–1221
Slamon DJ, Clark GM, Wong SG, Levin WJ, Ullrich A, McGuire WL (1987) Human breast cancer: correlation of relapse and survival with amplification of the HER-2/neu oncogene. Science 235: 177–182
Slamon DJ, Leyland-Jones B, Shak S, Fuchs H, Paton V, Bajamonde A, Fleming T, Eiermann W, Wolter J, Pegram M, Baselga J, Norton L (2001) Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med 344: 783–792
Stadtmauer EA, O'Neill A, Goldstein LJ, Crilley PA, Mangan KF, Ingle JN, Brodsky I, Martino S, Lazarus HM, Erban JK, Sickles C, Glick JH (2000) Conventional-dose chemotherapy compared with high-dose chemotherapy plus autologous hematopoietic stem-cell transplantation for metastatic breast cancer: Philadelphia Bone Marrow Group. N Engl J Med 342: 1069–1076
Tallman MS, Gray R, Robert NJ, LeMaistre CF, Osborne CK, Vaughan WP, Gradishar WJ, Pisansky TM, Fetting J, Paietta E, Lazarus HM (2003) Conventional adjuvant chemotherapy with or without high-dose chemotherapy and autologous stem-cell transplantation in high-risk breast cancer. N Engl J Med 349: 17–26
Tan-Chiu E, Yothers G, Romond E, Geyer Jr CE, Ewer M, Keefe D, Shannon RP, Swain SM, Brown A, Fehrenbacher L, Vogel VG, Seay TE, Rastogi P, Mamounas EP, Wolmark N, Bryant J (2005) Assessment of cardiac dysfunction in a randomized trial comparing doxorubicin and cyclophosphamide followed by paclitaxel, with or without trastuzumab as adjuvant therapy in node-positive, human epidermal growth factor receptor 2-overexpressing breast cancer: NSABP B-31. J Clin Oncol 23: 7811–7819
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Bengala, C., Zamagni, C., Pedrazzoli, P. et al. Cardiac toxicity of trastuzumab in metastatic breast cancer patients previously treated with high-dose chemotherapy: a retrospective study. Br J Cancer 94, 1016–1020 (2006). https://doi.org/10.1038/sj.bjc.6603060
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6603060
Keywords
This article is cited by
-
The effect of training interventions on physical performance, quality of life, and fatigue in patients receiving breast cancer treatment: a systematic review
Supportive Care in Cancer (2019)
-
Efficient induction of a Her2-specific anti-tumor response by dendritic cells pulsed with a Hsp70L1–Her2341–456 fusion protein
Cellular & Molecular Immunology (2011)
-
Adjuvant effect of HER-2/neu-specific adenoviral vector stimulating CD8+ T and natural killer cell responses on anti-HER-2/neu antibody therapy for well-established breast tumors in HER-2/neu transgenic mice
Cancer Gene Therapy (2011)
-
Anti-HER2 vaccines: new prospects for breast cancer therapy
Cancer Immunology, Immunotherapy (2010)
-
Analysis of cardiotoxicity from rh-endostatin therapy combined with chemotherapy
Chinese Journal of Clinical Oncology (2008)