Abstract
Thalidomide is effective in the treatment of multiple myeloma. The immunomodulatory drug and thalidomide analogue lenalidomide is currently in late stage clinical development for MDS and multiple myeloma. This minireview highlights the course of initial and ongoing lenalidomide clinical development in oncology with reference to earlier thalidomide studies.
Similar content being viewed by others
Preclinical development of IMiDs®
The IMiDs® are immunomodulatory thalidomide analogues designed to optimise certain properties including anticancer properties, but they lack or minimise much of the toxicity associated with thalidomide (Bartlett et al, 2004a). Extensive preclinical testing of this class of compound, involving pharmacology, pharmacokinetics and toxicity, has led to the identification of lenalidomide (CC-5013; REVLIMID®) for clinical development in the oncology setting.
While the IMiDs share many of thalidomide's biological properties, the relative potency and range of these effects vary quite dramatically from each other and from thalidomide. Thus, each molecule cannot be assumed to have the same overall biological effects or therapeutic properties as thalidomide or other IMiDs. Preclinical data continue to support the clinical application of lenalidomide in cancer. For example, in contrast to thalidomide's teratogenicity, lenalidomide is nonteratogenic in the New Zealand rabbit preclinical model, which is the most sensitive animal model for thalidomide-associated teratogenicity.
The IMiDs have many different effects on biological systems and the combination of these properties probably accounts for their antineoplastic activity. IMiDs are antiangiogenic (Dredge et al, 2002a; Lentzsch et al, 2002) and T-cell costimulatory (Haslett et al, 1998). IMiDs also activate the innate component of the immune system: enhanced natural killer cell cytotoxicity leading directly to multiple myeloma cell lysis (Davies et al, 2001). The ability of IMiDs to activate innate immune responses may be crucial to the generation of effective adaptive antitumour responses in vivo, although this area remains relatively unexplored, as has a potential role for IMiDs in the enhancement of protective antitumour immunity (Dredge et al, 2002b).
Certain IMiDs appear to possess direct in vitro antimyeloma activity (Hideshima et al, 2000); primary human multiple myeloma (MM) cells derived from the bone marrow of patients resistant to chemotherapy are susceptible to IMiD-induced growth arrest. IMiDs may also potentiate the effects of TNF-related apoptosis-inducing ligand (TRAIL), dexamethasone and proteasome inhibitors that are currently used as antimyeloma therapies. These IMiDs can also interfere with myeloma cell–bone marrow stromal cell interactions by affecting adhesion molecule expression, which might be crucial for MM cell growth and survival, and prevent the upregulation of IL-6 and vascular endothelial growth factor (VEGF), which is involved in angiogenesis (Gupta et al, 2001).
Clinical development of lenalidomide
Thalidomide is currently indicated in the US only for the cutaneous manifestations of erythema nodosum leprosum (ENL), a reactional state of leprosy. A regulatory application is under review by the US Food and Drug Administration for use in MM. In Australia, New Zealand, Turkey and Israel, thalidomide is approved for the treatment of MM after the failure of standard therapies, as well as for ENL. Teratogenicity is the most serious potential side effect; therefore, thalidomide is available only under a restricted distribution system. In order to understand how IMiDs with their broad preclinical activities might affect human disease, Celgene embarked on a strategy to evaluate thalidomide's therapeutic activity in small groups of patients with a wide variety of diseases. Larger trials in more targeted disease states followed, based on the early signals obtained during these small clinical trials. Discussed below will be a brief review of what has been observed with thalidomide and lessons learned for further development of lenalidomide, the lead IMiD chosen for use in the oncology setting.
Multiple myeloma
Multiple myeloma is an incurable B-cell malignancy characterised by the clonal proliferation of malignant cells, usually in the bone marrow, that leads to the production of a monoclonal immunoglobulin. Multiple myeloma afflicts 14 000–15 000 new patients annually in the US. The current median survival rate for symptomatic patients is 3–5 years. High-dose chemotherapy (Melphalan) combined with transplantation of haematopoietic stem cells increases the rate of complete remission and extends event-free and overall survival. However, relapse rates are very high and few salvage therapies are available. Antiangiogenic therapy is a viable option for the treatment of patients with MM since it is associated with prominent bone marrow vascularity, the degree of which correlates with prognosis. In addition, plasma levels of various proangiogenic molecules are elevated in active MM. It is also evident that circulating endothelial progenitor cells (EPC) contribute to angiogenesis in MM and that the elevation of EPC levels correlates with disease activity. Interestingly, inhibition of EPC is associated with patient response to thalidomide (Zhang et al, 2005). Also, since adhesion to bone marrow stroma is associated with chemotherapy resistance, thalidomide and lenalidomide therapy might theoretically make previously chemotherapy-resistant tumours sensitive by affecting stromal–myeloma cell interactions. The clinical strategy for the use of thalidomide in MM was to determine its activity as monotherapy, followed by trials using it with other drug combinations including drugs that were not previously effective in treating patients.
Monotherapy thalidomide trials in advanced relapsed/refractory (Kumar et al, 2003; Richardson et al, 2004) as well as previously untreated asymptomatic MM (Rajkumar et al, 2003; Weber et al, 2003) (also known as ‘smouldering’ or indolent myeloma) have consistently shown partial response rates (SWOG criteria) of approximately 30%, with an acceptable safety profile. Thalidomide combined with dexamethasone in relapsed, refractory MM induces a partial response in 56% of patients (Palumbo et al, 2004a). In newly diagnosed patients, thalidomide and dexamethasone therapy resulted in 64% partial responses (Rajkumar et al, 2002). A planned interim analysis of a phase III Eastern Cooperative Oncology Group study in newly diagnosed MM patients demonstrated a significantly higher response rate in patients randomised to thalidomide with dexamethasone than in those on dexamethasone alone (80 vs 53%, respectively, P=0.0023, n=109). Grade 3–4 toxicities were higher in the combination therapy arm, particularly deep vein thrombosis (Rajkumar et al, 2004a). The results of this ECOG trial have been submitted to the FDA to support the supplemental New Drug Application (sNDA) for the use of thalidomide in the treatment of MM.
Although uncommon with single agent thalidomide, there may be potential for thromboembolic events when thalidomide is combined with dexamethasone and other agents, which has led to preliminary evaluation of various regimens as prophylaxis in high-risk patients. Full therapeutic dose anticoagulation (either coumadin or low molecular weight heparin) has been used in patients who are at higher risk for DVT, with some evidence of prophylactic effect (Zangari et al, 2001) and aspirin may have a role in reducing incidence associated with thalidomide and DVd (Baz et al, 2004). While being anticoagulated as a treatment for a DVT, patients can be continued on thalidomide treatment (Zangari et al, 2001).
Encouraging results have also been observed with thalidomide when combined with a corticosteroid and a chemotherapeutic agent. A variety of such combinations of oral medications in newly diagnosed patients have produced greater than 80% partial responses and up to 26% complete responses (Dimopoulos et al, 2004; Palumbo et al, 2004b). Increased toxicities, including venous thromboses, have been seen with the melphalan/prednisone/dexamethasone (MPT) regimen (neither the pulsed melphalan/dexamethasone/thalidomide (MDT) nor the cyclophosphamide/thalidomide/dexamethasone (CTD) regimen reported increased DVT incidence), suggesting that the sequential administration of chemotherapy and thalidomide may result in higher responses, without an increase in DVTs (Dimopoulos et al, 2004). Thalidomide's addition to other commonly used combination therapies, such as VAD or Doxil/Vincristine/dexamethasone (DVd), results in almost a doubling of the response and complete response rate. Increased venous thromboses and infections may be controlled or prevented with low molecular heparin or low-dose aspirin and antibiotics, respectively.
Thalidomide has been observed to have activity in other haematological diseases and cancers, including myelodysplastic syndromes, MDS (Raza et al, 2001), chronic lymphocytic leukaemia (Furman et al, 2005), myelofibrosis (Mesa et al, 2004), Waldenstrom's macroglobulinaemia (Dimopoulos et al, 2003), prostate cancer (Dahut et al, 2004) and brain cancer (Fine et al, 2003).
On the basis of the thalidomide experience, lenalidomide was evaluated as an oral MM treatment in two Phase III clinical studies in patients with relapsed, refractory MM. Thalidomide-like side effects, such as somnolence, constipation or neuropathy were of low incidence despite anti-MM activity. At least 71% of 24 relapsed and refractory patients (median of three prior treatment regimens including autologous stem cell transplant and thalidomide in 15 and 16 patients, respectively) evaluated in a dose-finding trial experienced ⩾25% paraprotein reduction. The median time to best response was 2 months and the median treatment duration 6 months (Richardson et al, 2002). The most common grade 3 and 4 adverse events were neutropenia (grade 3 in 60%; grade 4 in 16%) and thrombocytopenia (grade 3 in 20%). No thromboembolic events were reported in this first monotherapy trial of lenalidomide in relapsed, refractory myeloma.
Other studies evaluated different dosing regimens in order to minimise myelosuppression. A phase II study comparing 25 mg lenalidomide daily for 20 days vs 50 mg daily for 10 days (both regimens repeated every 28 days) in relapsed, refractory MM patients reported that the 25 mg dosing schedule produced a greater response rate. A total of 40% of patients achieved ⩾50% paraprotein reduction with this dosing vs 15% using the higher dose/shorter regimen. The estimated 12-month event-free survival was 30%, and the estimated overall survival was 61% (Zangari et al, 2003).
A larger study evaluated 83 patients on one of two syncopated dosing schedules, and found that 30 mg daily (21 days out of every 28 days) caused less myelosuppression than 15 mg b.i.d. (21 days out of every 28), although response rates were similar. A total of 24% of patients achieved ⩾50% paraprotein reduction, including five patients with complete remission (6%). An additional 33% of 30 patients who progressed on lenalidomide alone achieved at least a partial response (⩾50% paraprotein reduction) when dexamethasone was added (Richardson et al, 2003).
Lenalidomide has also been evaluated with Doxil, Vincristine and dexamethasone (DVd) in relapsed, refractory MM (Baz et al, 2004) and in combination with dexamethasone in newly diagnosed MM (Rajkumar et al, 2004b). A phase I/II trial of lenalidomide in refractory MM in combination with DVd (DVd-R) reported a 33% (seven out of 21) complete and near complete response and a 66% SWOG response. With prophylactic low-dose aspirin, one pulmonary embolus occurred (in a refractory patient with renal failure, performance status 3). Amoxicillin and acyclovir were also included in the protocol. Grade 3 neutropenia occurred in two patients, but there was no neutropenic sepsis. The other grade 3 adverse event reported was neuropathy (one patient) (Hussein et al, 2004).
The first report of lenalidomide in newly diagnosed MM patients was in combination with pulsed dexamethasone. The first analysis of this phase II trial occurred when the trial had been running for less than 6 months. Despite this short observation period, an 83% (25 out of 30) objective response rate was observed. Patients received 81 mg day−1 of aspirin as DVT prophylaxis. Although various grade 3 nonhaematological toxicities were observed, there were no toxicities ⩾grade 4 and no deep vein thromboses (Rajkumar et al, 2004b).
Two phase III randomised, double-blind, multicentre trials (US, Canada, Australia and Europe) of lenalidomide plus high-dose dexamethasone vs high-dose dexamethasone alone in previously treated patients with MM were conducted in more than 700 relapsed/refractory patients. In March 2005, a protocol-specified interim analysis by an Independent Data Monitoring Committee determined that for both trials there was a statistically significant improvement in time to disease progression in those patients randomised to receive lenalidomide/dexamethasone vs dexamethasone alone. The prespecified P-value for stopping the trials (P<0.0015) was exceeded and the safety profile was favourable. Reported in a Scientific Symposium at the 2005 American Society of Clinical Oncology (ASCO), the primary end point of time –to disease progression in the lenalidomide plus dexamethasone arm was 60.1 weeks (53.4 weeks – International) compared with a median time –to disease progression of 20.7 weeks (20.6 – International) for the dexamethasone alone arm (P⩽0.00001). Overall response rate with lenalidomide/dex was 61.2% (57.9% – International) vs 22.8% (21.7% – International) with dex alone (P⩽0.001). The complete response rate was 26.5 and 13.6% (lenalidomide/dex) vs 4.1 and 4.0% (dex alone) based on the investigators’ assessment.
Increased side effects were noted in the combination arm, compared with the dex/placebo arm, particularly grade 3/4 neutropenia and thrombocytopenia. Thromboembolic events were noted in a greater percentage of US patients than International patients (13.5 and 4.5%, respectively) (vs 3.5/3.4% in placebo/dex arm), suggesting that further investigation is required to explain this finding.
Treatment assignments will be unblinded, affording patients in the control arm the opportunity to add lenalidomide to their treatment regimen. These trials will form the basis for regulatory filings.
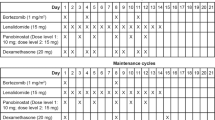
Lenalidomide is also currently used in combination with other therapies that have antimyeloma activity. A number of cooperative groups in US and Europe are evaluating lenalidomide's activity in a variety of MM disease states (See Table 1).
MDS and other haematological malignancies
The myelodysplastic syndromes (MDS) are a spectrum of malignant disorders of blood cell production, which affects over 250 000 people worldwide, with the potential to develop into acute leukaemia. Lenalidomide appears to be very active in restoring red blood cell production in anaemic MDS patients, enabling them to become independent of blood transfusions. Even more remarkable is the effect of lenalidomide on patients with the 5q-syndrome (a type of MDS) in which treatment can render undetectable the 5q-chromosomal deletion that defines the condition. The apparent efficacy of lenalidomide in this patient population led to the submission of a New Drug Application (NDA) in April 2005 seeking approval to market this drug as a treatment for transfusion-dependent MDS patients with a 5q deletion chromosomal abnormality.
In an open-label trial, 43 patients with primary MDS (French–American–British (FAB) criteria), who were transfusion dependent (74%) or had symptomatic anaemia (Hg <10g dl−1), received lenalidomide for 16 weeks (List et al, 2005a). Three oral dosing schedules were evaluated: 25, 10 and 10 mg day−1 × 21 days of a 28-day cycle. Patients had derived no response to recombinant erythropoietin, or had a low probability of responding (endogenous serum level >500 mU ml−1). FAB classes were refractory anaemia (RA-47%), RA with ringed sideroblasts (RARS-30%), RA with excess blasts (RAEB-19%), RAEB in transformation (RAEB-t-2%) and chronic myelomonocytic leukaemia (CMML-2%). Clonal karyotypic abnormalities (⩾2 abnormal cells in metaphase) were present in 46% of patients, including interstitial deletion of chromosome 5q31.1 alone in 11 patients.
Response rate (modified International Working Group (IWG) criteria) was 56%, with 20 out of 32 (63%) transfusion-dependent patients achieving transfusion independence, and one out of 11 patients, who did not require transfusions, increasing haemoglobin >2 g dl−1. The median time to response varied with dose level (9 weeks at 25 mg day−1 to 11.5 weeks at 10 mg syncopated dosing). After a median of 81 weeks, the median duration of transfusion independence had not been reached and the median haemoglobin was 13.2 g dl−1.
An interesting finding was that the cytogenetic pattern was significantly correlated with haematological response: 83% of patients with 5q31.1 deletion responded vs 57% with a normal karyotype and 15% with other cytogenetic abnormalities. FAB and IPSS categories did not correlate with response. The median time to response was more rapid in patients with 5q31.1 deletion than in patients with a normal or other karyotype (8 weeks vs 11.2, P=0.029). Eleven out of 20 patients with clonal cytogenetic abnormalities had cytogenetic responses, including 10 complete cytogenetic remissions. Nine of the 10 complete cytogenetic remissions occurred in patients with del(5)(q31.1). The median time to cytogenetic remission was 8 weeks.
Neutropenia (65%, all ⩾grade 3) and thrombocytopenia (74% overall; 54% ⩾grade 3) were the most common adverse events. Severe myelosuppression was dose dependent and led to treatment interruption or dose reduction in 58% of patients with the median time to treatment resumption being 22 days. Other adverse events were mild and infrequent. This initial indication of lenalidomide activity in MDS led to phase II and III studies of lenalidomide in MDS with and without 5q deletion.
Data reported in a plenary session at ASCO 2005 support the previous findings. Of 148 transfusion-dependent MDS patients with del5q31, participating in a multicentre phase II trial of lenalidomide, 66% achieved transfusion independence (ITT analysis), achieving a median haemoglobin increase of 5.3 g dl−1. With a median duration of 58 weeks follow-up, 73% of responders remained transfusion independent, and the median duration of transfusion independence had not been reached. A greater proportion of patients with an isolated, vs other del5q became transfusion independent (69 vs 49%, P=0.003). Cytogentic response was noted in 70% of patients; 63% of these achieved complete cytogenetic remission. The most common adverse events were ⩾grade 3 neutropenia or thrombocytopenia, which resolved after dose reduction or after temporarily withholding lenalidomide. In total, 15 deaths occurred, two of which were suspected to be drug related (List et al, 2005b). The data from this trial form the basis for the NDA.
Lenalidomide is currently in phase II studies in myelofibrosis with myeloid metaplasia. Clinically relevant responses have been reported in four out of 15 (27%) patients. Improvement in anaemia (two patients), splenomegaly (two patients) and/or constitutional symptoms (three patients) occurred. One patient became transfusion independent in addition to experiencing marked improvement in constitutional symptoms. One patient's haemoglobin increased to 13.4 g dl−1 (from 8.3 g dl−1), leucocytes decreased from >66 × 109 to within normal range and circulating blasts disappeared (pretreatment level 9%) after lenalidomide therapy. Grade 3 and 4 adverse events included neutropenia (five patients), thrombocytopenia (three patients), rash and fatigue (two patients each). Three patients experienced extreme thrombocytosis (Tefferi et al, 2004) (steep increase in platelet count has also been reported in a small number of patients taking thalidomide for myelofibrosis). One patient developed disseminated extramedullary haematopoiesis after taking lenalidomide for 1 month.
Encouraging results have also been reported from a small trial of lenalidomide in chronic lymphocytic leukaemia, with six out of seven evaluable patients responding at day 30 (one CR, five PR, one withdrew consent) (Miller et al, 2005). Lenalidomide is also currently being evaluated in other haematological conditions including amyloidosis and Waldenstrom's macroglobulinaemia.
Lenalidomide has been granted both Orphan Drug and Fast Track status by the FDA and Orphan Drug status for both MM and MDS by the European Commission on MM and the European Commission on MDS.
IMiDs in solid tumours
The first published study of lenalidomide in patients with solid tumours suggests that lenalidomide has limited clinical activity in patients with advanced and heavily pretreated metastatic malignant melanoma and other solid cancers (Bartlett et al, 2004b). The primary objective of this phase I study was to assess the safety and tolerability of lenalidomide and in this regard there were no serious adverse effects attributed to treatment. Also, analyses of serum cytokines and peripheral blood cell-surface markers showed conclusive evidence for immune activation. However, unblinded interim results of two phase III lenalidomide monotherapy studies in malignant melanoma patients determined that a statistically significant treatment effect would not be achieved, although the safety profile was acceptable. On the recommendation of the Data Monitoring Committee, the programme was halted.
Lenalidomide is currently being evaluated in non-Hodgkin's lymphoma, NSCLC and cancers of the pancreas, prostate, brain, kidneys and ovaries.
Conclusions
Thalidomide is now recognised as an agent with meaningful activity in haematology and oncology. This activity provided the rationale for the development of thalidomide analogues with the goal of enhancing antineoplastic activity while reducing or eliminating thalidomide-associated side effects. The IMiDs® have antiangiogenic, direct antitumour, anti-inflammatory and immune stimulatory properties. A particular challenge is to characterise how these properties interact within the physiological milieu of disease states.
As this review has documented, lenalidomide has entered the clinic for the treatment of various cancers. Pharmacological, preclinical and clinical data clearly demonstrate qualitative and quantitative differences between thalidomide and lenalidomide. The reported remarkable safety and efficacy of lenalidomide in the treatment of MDS and MM support regulatory filings in these indications. In addition, other neoplastic conditions will be assessed for sensitivity to lenalidomide. As with most agents in haematology/oncology, the authors believe that appropriate combination therapy involving lenalidomide will lead to highly effective therapy for treating a variety of malignant conditions. We look forward to understanding how various combination therapies can improve the management of afflicted patients.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Bartlett JB, Dredge K, Dalgleish AG (2004a) The evolution of thalidomide and its IMiD derivatives as anticancer agents. Nat Rev Cancer 4: 314–322
Bartlett JB, Michael A, Clarke IA, Dredge K, Nicholson S, Kristeleit H, Polychronis A, Pandha H, Muller GW, Stirling DI, Zeldis J, Dalgleish AG (2004b) Phase I study to determine the safety, tolerability and immunostimulatory activity of thalidomide analogue CC-5013 in patients with metastatic malignant melanoma and other advanced cancers. Br J Cancer 90(5): 955–961
Baz R, Marchant K, Yiannaki EO, Platt L, Brand C, Tso E, Hussein MA (2004) Aspirin decreases the thrombotic complications (DVT) of liposomal doxorubicin, vincristine, decreased frequency dexamethasone and thalidomide (DVd-T) treatment of multiple myeloma (MM). Blood 104(11): 658a–659a, (abstract #2397)
Dahut WL, Gulley JL, Arlen PM, Liu Y, Fedenko KM, Steinberg SM, Wright JJ, Parnes H, Chen CC, Jones E, Parker CE, Linehan WM, Figg WD (2004) Randomized phase II trial of docetaxel plus thalidomide in androgen-independent prostate cancer. J Clin Oncol 22(13): 2532–2539
Davies FE, Raje N, Hideshima T, Lentzsch S, Young G, Tai YT, Lin B, Podar K, Gupta D, Chauhan D, Treon SP, Richardson PG, Schlossman RL, Morgan GJ, Muller GW, Stirling DI, Anderson KC (2001) Thalidomide and immunomodulatory derivatives augment natural killer cell cytotoxicity in multiple myeloma. Blood 98: 210–216
Dimopoulos MA, Repoussis P, Terpos E, Kyrtsonis MC, Zomas A, Katodritou E, Delibasi S, Vassou A, Anagnostopoulos A, Pouli A, Zervas K, Margaritis D, Anagnostopoulos N, Maniatis AG (2004) Primary treatment with pulsed melphalan, dexamethasone, thalidomide (MDT) for symptomatic patients with multiple myeloma [greater than or equal to] 75 years of age. Blood 104(11): 414a (abstract #1482)
Dimopoulos MA, Tsatalas C, Zomas A, Hamilos G, Panayiotidis P, Margaritis D, Matsouka C, Ecomonopoulos T, Anagnostopoulos N (2003) Treatment of Waldenstrom's macroglobulinemia with single-agent thalidomide or with the combination of clarithromycin, thalidomide and dexamethasone. Semin Oncol 30(2): 265–269
Dimopoulos M, Weber D, Chen C, Spencer A, Niesvizky R, Attal M, Knight R, Faleck H, Olesnyckyj M, Zeldis J (2005) Evaluating oral lenalidomide (revlimid) and dexamethasone versus placebo and dexamethasone in patients with relapsed or refractory multiple myeloma. Haematologica (The Hematol J) 90(Suppl 2): 160, Abstract # 0402
Dredge K, Marriott JB, Macdonald C, Man H, Chen R, Muller GW, Stirling D, Dalgleish AG (2002a) Novel thalidomide analogues display anti-angiogenic activity independently of immunomodulatory effects. Br J Cancer 87(10): 1166–1172
Dredge K, Marriott JB, Todryk SM, Muller GW, Chen R, Stirling DI, Dalgleish AG (2002b) Protective antitumor immunity induced by a costimulatory thalidomide analog in conjunction with whole tumor cell vaccination is mediated by increased Th1-type immunity. J Immunol 168(10): 4914–4919
Fine HA, Wen PY, Maher EA, Viscosi E, Batchelor T, Lakhani N, Figg WD, Purow BW, Borkowf CB (2003) Phase II trial of thalidomide and carmustine for patients with recurrent high-grade gliomas. J Clin Oncol 21(12): 2299–2304
Furman RR, Leonard JP, Allen SL, Coleman M, Rosenthal T, Gabrilove JL (2005) Thalidomide alone or in combination with fludarbabine are effective treatments for patients with fludarabine-relapsed and refractory CLL. J Clin Oncol 23(16, Suppl): 595s, (abstract # 6640)
Gupta D, Treon SP, Shima Y, Hideshima T, Podar K, Tai YT, Lin B, Lentzsch S, Davies FE, Chauhan D, Schlossman RL, Richardson P, Ralph P, Wu L, Payvandi F, Muller G, Stirling DI, Anderson KC (2001) Adherence of multiple myeloma cells to bone marrow stromal cells upregulates vascular endothelial growth factor secretion: therapeutic applications. Leukemia 15: 1950–1961
Haslett PA, Corral LG, Albert M, Kaplan G (1998) Thalidomide costimulates primary human T lymphocytes, preferentially inducing proliferation, cytokine production, and cytotoxic responses in the CD8+ subset. J Exp Med 187: 1885–1892
Hideshima T, Chauhan D, Shima Y, Anderson KC (2000) Thalidomide and its analogs overcome drug resistance of human multiple myeloma cells to conventional therapy. Blood 96(9): 2943–2950
Hussein MA, Karam MA, Brand C, Pearce GL, Reed J, Bruening K, Sartori P, Srkalovic G, Olesnyckyj M, Knight R, Balinski K, Zeldis J (2004) Doxil (D), vincristine (V), reduced frequency dexamethasone (d) and Revlimid(R) (DVd-R) a phase I/II trial in advanced relapsed/refractory multiple myeloma (Rmm) patients. Blood 104(11): 63a–64a, (abstract #208)
Kumar S, Gertz MA, Dispenzieri A, Lacy MQ, Geyer SM, Iturria NL, Fonseca R, Hayman SR, Lust JA, Kyle RA, Greipp PR, Witzig TE, Rajkumar SV (2003) Response rate, durability of response, and survival after thalidomide therapy for relapsed multiple myeloma. Mayo Clin Proc 78(1): 34–39
Lentzsch S, Rogers MS, Leblanc R, Birsner AE, Shah JH, Treston AM, Anderson KC, D'Amato RJ (2002) S-3-amino-phthalimido-glutarimide inhibits angiogenesis and growth of B-cell neoplasias in mice. Cancer Res 62(8): 2300–2305
List AF, Kurtin S, Roe DJ, Buresh A, Mahadevan D, Fuchs D, Rimsza L, Heaton R, Knight R, Zeldis JB (2005a) Efficacy of lenalidomide in myelodysplastic syndromes. N Engl J Med 352: 549–557
List AF, Dewald G, Bennett J, Giagounadis A, Raza A, Feldman E, Powell B, Greenberg P, Zeldis J, Knight R (2005b) Hematologic and cytogenetic (CTG) response to lenalidomide (CC-3013) in patients with transfusion dependent (TD) myelodysplastic syndrome (MDS) and chromosome 5q31.1 deletion: results of the multicenter MDS-003 Study. J Clin Oncol 23(16, Suppl): 2s (abstract # 5)
Mesa RA, Elliott MA, Schroeder G, Tefferi A (2004) Durable responses to thalidomide-based drug therapy for myelofibrosis with myeloid metaplasia. Mayo Clin Proc 79(7): 883–889
Miller KC, Czuzman MS, DiMicelli L, McCarthy P, Bernstein ZP, Zeldis JB, Mohr A, Chanan-Khan AA (2005) Antileukemic effects of novel immunomodulatory agent lenalidomide (L) with or without rituximab (R) in patients (pts) with relapsed (rel) or refractory (ref) chronic lymphocytic leukemia (CLL). Encouraging preliminary results of an ongoing phase II clinical study. J Clin Oncol 23(16, Suppl): 574s (abstract # 6557)
Palumbo A, Bertola A, Falco P, Rosato R, Cavallo F, Giaccone L, Bringhen S, Musto P, Pregno P, Caravita T, Ciccone G, Boccadoro M (2004a) Efficacy of low-dose thalidomide and dexamethasone as first salvage regimen in multiple myeloma. Hematol J 5(4): 318–324
Palumbo A, Bertola A, Musto P, Caravita T, Callea V, Cangialosi C, Liberati AM, Niscola P, Catalano L, Grasso M, Lauta VM, Petti MC, Morandi S, Galli M, Bringhen S, Cavallo F, Falco P, Boccadoro M (2004b) A prospective randomized trial of oral melphalan, prednisone, thalidomide (MPT) vs oral melphalan, prednisone (MP): an interim analysis. Blood 104(11): 63a (abstract #207)
Rajkumar SV, Blood E, Vesole DH, Shepard R, Greipp PR (2004a) Thalidomide plus dexamethasone vs dexamethasone alone in newly diagnosed multiple myeloma (E1A00): results of a phase III trial coordinated by the Eastern Cooperative Oncology Group. Blood 104(11): 63a (abstract #205)
Rajkumar SV, Gertz MA, Lacy MQ, Dispenzieri A, Fonseca R, Geyer SM, Iturria N, Kumar S, Lust JA, Kyle RA, Greipp PR, Witzig TE (2003) Thalidomide as initial therapy for early-stage myeloma. Leukemia 17(4): 775–779
Rajkumar SV, Hayman S, Gertz M, Dispenzieri A, Lacy M, Greipp P, Geyer S, Iturria N, Fonseca R, Lust JA, Kyle RA, Witzig TE (2002) Combination therapy with thalidomide plus dexamethasone for newly diagnosed myeloma. J Clin Oncol 20(21): 4319–4323
Rajkumar SV, Hayman SR, Lacy MQ, Dispenzieri A, Hoering A, Geyer SM, Zeldenrust SR, Greipp PR, Fonseca R, Lust JA, Russell SJ, Kyle RA, Witzig TE, Gertz MA (2004b) Combination therapy with CC-5013 (lenalidomide; Revlimid™) plus dexamethasone (Rev/Dex) for newly diagnosed myeloma (MM). Blood 104(11): 98a (abstract #331)
Raza A, Meyer P, Dutt D, Zorat F, Lisak L, Nascimben F, du Randt M, Kaspar C, Goldberg C, Loew J, Dar S, Gezer S, Venugopal P, Zeldis J (2001) Thalidomide produces transfusion independence in long-standing refractory anemias of patients with myelodysplastic syndromes. Blood 98(4): 958–965
Richardson PG, Jagannath S, Schlossman R, Zeldenrust S, Rajkumar SV, Alsina M, Desikan KR, Mitsiades CS, Kelly K, Doss D, McKenney M, Gorelik S, Warren D, Freeman A, Rich R, Knight R, Olesnyckyj M, Patin J, Zeldis J, Dalton W, Anderson KC (2003) A multi-center, randomized, phase 2 study to evaluate the efficacy and safety of 2 CDC-5013 dose regimens when used alone or in combination with dexamethasone (Dex) for the treatment of relapsed or refractory multiple myeloma (MM). Blood 102(11): (abstract #825)
Richardson P, Schlossman R, Jagannath S, Alsina M, Desikan R, Blood E, Weller E, Mitsiades C, Hideshima T, Davies F, Doss D, Freeman A, Bosch J, Patin J, Knight R, Zeldis J, Dalton W, Anderson K (2004) Thalidomide for patients with relapsed multiple myeloma after high-dose chemotherapy and stem cell transplantation: results of an open-label multicenter phase 2 study of efficacy, toxicity, and biological activity. Mayo Clin Proc 79(7): 875–882
Richardson PG, Schlossman R, Weller E, Hideshima T, Mitsiades C, Davies F, LeBlanc R, Catley LP, Doss D, Kelly K, McKenney M, Mechlowicz J, Freeman A, Deocampo R, Rich R, Ryoo JJ, Chauhan D, Balinski K, Zeldis J, Anderson KC (2002) Immunomodulatory drug CC-5013 overcomes drug resistance and is well tolerated in patients with relapsed multiple myeloma. Blood 100(9): 3063–3067
Tefferi A, Hogan WJ, Wolanskyj AP, Shaw TA, Reyes GE, Hoering A, McClure RF, Mesa RA (2004) A phase II study of CC-5013 treatment for myelofibrosis with myeloid metaplasia: a preliminary report. Blood 104(11): 421a (abstract #1505)
Weber D, Rankin K, Gavino M, Delasalle K, Alexanian R (2003) Thalidomide alone or with dexamethasone for previously untreated multiple myeloma. J Clin Oncol 21(1): 16–19
Zangari M, Anaissie E, Barlogie B, Badros A, Desikan R, Gopal A, Morris C, Toor A, Siegel E, Fink L, Tricot G (2001) Increased risk of deep-vein thrombosis in patients with multiple myeloma receiving thalidomide and chemotherapy. Blood 98(5): 1614–1615
Zangari M, Barlogie B, Jacobson J, Zeldis JB, Anaissie EJ, Thertulien R, Fassas A, Lee C-K, Shaughnessy JD, Tricot GJ (2003) Revimid 25 mg (REV 25) × 20 vs 50 mg (REV 50) × 10 q 28 days with bridging of 5 mg × 10 vs 10 mg × 5 as post-transplant salvage therapy for multiple myeloma (MM). Blood 102(11): 1 (abstract #1642)
Zhang H, Vakil V, Braunstein M, Smith EL, Maroney J, Chen L, Dai K, Berenson JR, Hussain MM, Klueppelberg U, Norin AJ, Akman HO, Ozcelik T, Batuman OA (2005) Circulating endothelial progenitor cells in multiple myeloma: implications and significance. Blood 105(8): 3286–3294
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Bartlett, J., Tozer, A., Stirling, D. et al. Recent clinical studies of the immunomodulatory drug (IMiD®) lenalidomide. Br J Cancer 93, 613–619 (2005). https://doi.org/10.1038/sj.bjc.6602774
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6602774
Keywords
This article is cited by
-
Inhibition of metastatic potential in colorectal carcinoma in vivo and in vitro using immunomodulatory drugs (IMiDs)
British Journal of Cancer (2009)
-
Immunomodulatory drugs Revlimid® (lenalidomide) and CC-4047 induce apoptosis of both hematological and solid tumor cells through NK cell activation
Cancer Immunology, Immunotherapy (2008)
-
Phase II trial of lenalidomide in patients with metastatic renal cell carcinoma
Investigational New Drugs (2008)
-
Historical perspective and advances in the treatment of multiple myeloma
Oncology Reviews (2008)
-
New treatments for chronic lymphocytic leukemia
Current Oncology Reports (2007)