Abstract
A series of 176 archival cervical intraepithelial neoplasia (CIN) was analysed for the presence, viral load and integration status of ‘high-risk’ types of human papillomavirus (HR-HPV). The samples were assayed using newly developed methods based on real-time PCR. Two methods for the extraction of DNA from the paraffin-embedded biopsies were compared: a protocol based on the MagNA pure system (Roche) and a Qiagen spin column kit (Qiagen). It was possible to amplify 94% (166) of the samples. Of these, 36, 63 and 80% of the CIN I, II and III cases contained HR-HPV. HPV 16 was the most prevalent, and was found in 20, 28 and 46% of the CIN I, II and III cases, respectively. The second most frequent HR-HPV was type 33 group, and in CIN II it was as prevalent as HPV 16. The median number of copies of HR-HPV per cell was not significantly different in the CIN I, II and III cases, but there was a wide range of viral load values over several magnitudes, regardless of the grade of CIN. All samples were found to contain integrated forms of HPV 16, frequently mixed with an episomal form.
Similar content being viewed by others
Main
Intensive research has provided evidence for a central, causal role of certain types of HPV in the development of invasive cervical carcinoma (Schiffman et al, 1993; Davidson et al, 1994; Walboomers et al, 1999; Bosch and Munoz, 2002). The presence of high-risk HPV-DNA identifies both women with disease and those who are at a particular risk of progression to disease (Nobbenhuis et al, 1999). Persistent infection with high-risk types of HPV (HR-HPV), especially type 16, is regarded as the principal risk factor in the development of squamous cervical lesions or squamous cervical cancer (Munoz et al, 2003). However, most infections with HPV regress spontaneously, and, for the cases that do progress to cancer, a long period of latency is normally observed. HPV infections are prevalent and often transient among younger women, with a peak of 20–25% at 20–24 years of age. With increasing age, there is a decline in the prevalence of HPV to about 7% at 35 years of age (Soutter and Fletcher, 1994). It is likely that HPV-positive women at that age represent a subset of individuals who do not manage to clear their infections spontaneously. Thus, the persistence of a high-risk HPV infection is associated with the risk of developing cervical intraepithelial neoplasia (CIN).
A high prevalence of transient infections makes detection of the virus an inefficient means of identifying women at risk of developing cervical cancer (Ho et al, 1998; Jacobs et al, 2000). Viral load has been suggested as a marker of nontransient infection; a high HPV load in archival Pap smears with normal cytology had a considerably higher risk of developing carcinoma in situ, and even cervical squamous carcinoma (Josefsson et al, 2000; Lorincz et al, 2002; Dalstein et al, 2003; Gravitt et al, 2003; Moberg et al, 2004). Recently, it has been concluded that HPV load is a type-dependent risk marker for invasive carcinoma (Moberg et al, 2005). Furthermore, it has been suggested that there is an association between a high viral load and the persistence of infection with HPV (Ho et al, 1998).
The integration status of high-risk HPV in premalignant cervical lesions might be a further promising risk marker for progression of cervical cancer (Lazo, 1997; Kalantari et al, 1998). Viral DNA integration into the host cell genome usually disrupts the E1 and E2 open reading frames, while those of E6 and E7 remain intact (Kalantari et al, 1998, 2001). The deletion of E2 ORF, due to the integration, results in disruption of expression of E2 protein and subsequent upregulation of the transcription of the oncogenic E6 and E7 proteins (Romanczuk and Howley, 1992). Continuous production of oncogenic E6 and E7 proteins contribute to the malignant state in infected tissue. Thus, viral integration into the host genome is possibly another critical event for malignant transformation.
In the present study, our aim was to evaluate the frequency of HR-HPV types and viral load in a series of paraffin-embedded biopsies with pre-neoplastic and neoplastic lesions. Based on these data, we sought to determine if type distribution and viral loads of different HR-HPV types in CIN I–III lesions show any significant differences. We also evaluated any differences in the integration status of HPV 16, as a function of the grade of CIN.
Materials and methods
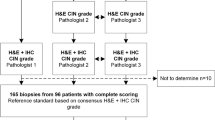
Specimens from 176 biopsies, which represented CIN I–III lesions, obtained between 2002 and 2003, were collected from the Department of Pathology, Karolinska University Hospital at Huddinge. The biopsies were fixed in neutral buffered formalin and embedded in paraffin. Serial sections were cut from each block. The first was stained with haematoxylin-eosin and evaluated histopathologically, whereas the following were used for the preparation of DNA and the HPV test. The biopsies were grouped according to the morphological diagnosis and types of HPV present. The diagnosis of all cases was reviewed and reconfirmed by one pathologist.
Extraction of DNA from tissue sections
To optimise the DNA extraction method for our study, two different DNA-extraction protocols were compared.
Extraction using specific magnetic glass particles (MGPs) to bind DNA (Roche MagNA pure kit)
Protocol A is based on binding the isolated DNA from tissue samples to the surface of specific MGPs. This procedure is automated and performed by using the MagNA Pure LC system (Roche).
The paraffin-embedded (formaldehyde-fixed) tissue sections were deparaffinised with xylene and absolute ethanol. To melt the paraffin, the paraffin-embedded tissue sections were incubated at 65°C for 10 min, and, subsequently, 1 ml xylene and 500 μl absolute ethanol were added and mixed gently. After centrifugation at 14 000 rpm for 2 min, the supernatant was discarded and 1 ml absolute ethanol was added. After a new 2-min centrifugation at 14 000 rpm, the pellet was dried for 10–15 min using a Speed Vac vacuum drier.
The dried pellet was re-suspended in a 130 μl tissue lysis buffer and 20 μl proteinase K, and was subsequently incubated at 56°C overnight. The cell suspension was mixed with a 350 μl cell lysis buffer in a sample cartridge, and then loaded into the MagNa Pure instrument. The other reagents, that is, MGPs, which bind the total DNA from the lysed cell suspension, proteinase K, and a wash and elution buffer, were also loaded into the instrument. The extracted DNA was eluted with a 50 μl elution buffer.
Extraction using a specific spin column to bind DNA (Qiagen kit)
Protocol B is a manual DNA extraction method, which is based on the QIAamp Spin Column kit (Qiagen).
The paraffin-embedded tissue sections were deparaffinised by the procedure described above. After addition of 1 ml xylene, the tube was incubated at room temperature for 30 min and subsequently centrifuged at 14 000 rpm for 5 min. This step was repeated once, after which 1 ml absolute ethanol was added to the tube, followed by centrifugation at 14 000 rpm for 5 min. The pellet was dried in the Speed Vac for 10–15 min and was then resuspended in a 180 μl tissue lysis buffer and 20 μl proteinase K. After incubation of the solution at 56°C overnight, a 200 μl cell lysis buffer was added. A new incubation at 70°C for 10 min was carried out before the addition of 200 μl 95% ethanol. The mixture was then applied to the QIAamp spin column. After centrifugation of the column at 8000 rpm for 1 min, the column was washed twice with a 500 μl wash buffer AW1 followed by AW2. The purified DNA was eluted with 50 μl distilled water.
Detection and quantification of HPV by the ‘QUANTOVIR HPV’ system
Extracted DNA from the MagNA pure was subsequently quantified, and HR-HPV typed, by using the ‘QUANTOVIR HPV’ detection and quantification system as described by Moberg et al (2003).
The ‘QUANTOVIR HPV’ detection and quantification kit was used for preparation of the Master Mix. The real-time PCR reaction was performed in a total volume of 25 μl (22 μl Master Mix and 3 μl DNA template), and with the use of optical 96-well micro-plates were used. The Master Mix contained 1 × PCR buffer – 200 μ M each of dATP, dCTP and dGTP and 400 μ M dUTP – 3.5 mM MgCl2, 10 × G-carboxy-X-rhodamine,6-Rox, and 0.625 U Taq DNA polymerase final concentrations in sterile water. The PCR amplification program consisted of an initial holding step of 10 min at 95°C, followed by a two-step cycle of 15 s at 95°C and 1 min at 57°C for 40 cycles. Three parallel reactions per sample were performed: no. 1 quantified HPV 16, 31, 18 and 45 (the last two together); no. 2 quantified HPV 33, 35, 39, 52, 58 and 67 (HPV 33, 52, 58 and 67 together); no. 3 quantified the single copy human gene for hydroxymethylbilane synthase. A total of six nontemplate control reactions, which consisted only of PCR components without template DNA, were used as negative controls to ensure that the reagent mix was free of contamination. The assay was performed by using the ABI PRISM 7700 Sequence Detection System, running the 1.6.3 version of the SDS program (Applied Biosystems).
Since the ABI 7700 software could not quantify three different fluorophores in the same reaction, a separate QUANTOVIR algorithm was developed, using the MATLAB program vers. 5.2.1, directly coupled to the data collection program of the ABI 7700 apparatus. This was used for calculation of the threshold cycle, and conversion of the data into HPV copy numbers per cell. The number of cells was calculated from the copy numbers of a single copy human gene (hydroxymethylbilane synthase), and this and other calculations were performed automatically by the specially developed software.
The established linear dynamic range of the method is 102–107 copies of HR-HPV per genomic DNA equivalent (Moberg et al, 2003).
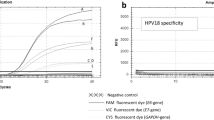
HPV integration status
The recently developed real-time PCR-based integration method of Peitsaro et al (2002) was performed by using the ABI prism 7700 Sequence Detection system and the TaqMan PCR Master Mix (PE Applied Biosystems, Perkin-Elmer). The basic principle of the method is to use specific primers and probes for separate assays of the region (‘hinge region’) of the E2 ORF, most often deleted during integration, and part of the E6 ORF. The latter ORF is always retained in the integrated virus. The E6 probe was labelled with FAM at the 5′- and TAMRA at the 3′-end, while the E2 probe was labelled with VIC at the 5′- and TAMRA at 3′-end. The final concentrations of primers and probes in a total of 50 μl of reaction mixture were 0.3 and 0.1 μ M, respectively. Two standard curves for E6 and E2 were obtained by amplification of a dilution series of one million to 10 copies of a clone of the entire HPV 16 genome in pBR322. There was a linear relationship between the threshold cycle values plotted against the log of the copy number over the entire range of dilutions (data not shown). The 96-well optical plate was used to run reactions. In each experiment, samples were loaded in duplicate and three negative controls were included.
DNA from the SiHa cell line, containing one copy of fully integrated HPV 16, was also used as a control for full integration in these experiments. No E2 signal should be produced, since the assayed region of E2 is deleted in SiHa cells.
Results
The study comprises 166 cases: among these 50 (30%) CIN I, 60 (36%) CIN II and 56 (34%) CIN III. The mean age of women with CIN I was 39.6, in women with CIN II was 33.3 and in women with CIN III was 34.7.
Extraction method
A comparison between the Qiagene and Magna Pure kits showed that Magna Pure provided higher DNA yields than Qiagene for the extraction of paraffin-embedded tissue sections. The MagNA pure system has further advantages in its semi-automation and quickness. It has been used throughout this study.
Frequencies of HR-HPV
Of the 176 samples analysed with the ‘Quantovir HPV’ system, 10 were totally negative, that is, no signal was obtained from the human gene. The frequencies of the different types of HR-HPV in the remaining 166 samples, from different stages of CIN, are summarised in Table 1 and Figure 1.
There was a steady increase in the frequency of HR-HPV from CIN I to III. Of the CIN III samples, 45 (80%) were positive for HR-HPV. As shown in Figure 1, the increased frequencies of HR-HPV were due to increase in the number of positive cases with HPV 16, 18/45 and 33 groups (HPV 33, 52, 57, 58), while the number of positive cases with HPV 31 and 39 was constant. As could be expected, the oncogenic HPV 16 predominated at all stages of CIN: 20, 28 and 46% at CIN I, II and III, respectively.
However, the high proportion (23%) of the HPV 33 group in the biopsies from CIN II seemed almost as high as that for HPV 16 (Table 1, Figure 1). No HPV 35 was found in this material.
Viral loads
HR-HPV
The viral loads obtained for HR-HPV in the different grades of CIN are summarised in Figure 2. There was a distribution of viral load values of several orders of magnitude at all grades of CIN. The span of values of copies of HR-HPV per cell ranged from 0.14 to 8400. The mean values of the copies per cell were: CIN I – 8; CIN II – 17 and CIN III – 6. However, by using the one-way ANOVA analysis, there was no significant difference determined between these mean values.
HPV 16
Since HPV 16 is the most predominant type in this material, as well as in cervical squamous carcinomas, viral load values were examined separately for this type. As for HR-HPV in general, there was an equally broad distribution of viral loads (Figure 3). The mean values of copies per cell were: CIN I – 2, CIN II – 18 and CIN III – 6. Moreover, in this case, there was no significant difference between the mean values as determined by the one-way ANOVA analysis.
Viral integration
A specially designed real-time PCR method (Peitsaro et al, 2002) was used to estimate HPV 16 integration by comparing viral loads from the parts of the E2 ORF that are mostly deleted during integration, and those of the E6 ORF. The latter gives an estimate of the total number of HPV 16 genomes, episomal and integrated. All of the 48 HPV 16 cases, found in the previous typing and viral load determination, were found to contain integrated virus genomes. However, there was a higher proportion of cases with no detectable copies of the E2 gene, indicating complete integration (Table 2), at the CIN III stage (36%) than at the CIN I (25%) and CIN II (7%) stages. Among the cases showing E2/E6 ratios less than 1.0, presumably containing episomal and integrated virus genomes, the relative contents of the two forms varied considerably (Figure 4). The average ratios of episomal and integrated forms were not significantly different in the three stages of CIN, as determined by the one-way ANOVA analysis. However, if a cutoff value is introduced at a ratio of 1 : 100 of episomal and integrated forms, respectively, there are significantly more cases below this value in CIN III (horizontal line in Figure 4).
HPV 16 integration status at different CIN grade. Integration status is calculated from the ratios of copy numbers for gene E2 divided by the same values for gene E6. The E2 values are related to the number of episomal copies, whereas the E6 values arise from the total number of HPV 16 copies. The values are shown in log form. The top horizontal bar indicates the log ratio expected from purely episomal form (E2/E6 ratio=1). The horizontal line in the upper graph at log −2, indicates an integration status, where there is one episomal form for a total of 100 copies of HPV 16.
Discussion
Epidemiological and molecular biological studies have shown that infection with high-risk HPV is the most important aetiological agent in the pathogenesis of cervical cancer (Bosch et al, 1995). At present, more than 99% of the squamous cell tumours are considered to harbour oncogenic types of HPV (Walboomers et al, 1999). HPV 16, 18, 45, 31 and 33 are the most frequently identified viruses in CIN II–III and cervical squamous cell carcinomas (Munoz et al, 2003).
In our study, a stored formalin-fixed and paraffin-embedded material was used for the Quantovir test. We investigated the presence of different types of HPV and the viral loads in women with CIN I–III. The Quantovir test, a quantitative assay which is applicable for clinical use and capable of detecting a range of high-risk types of HPV involved in cervical carcinogenesis, has been previously described in detail (Moberg et al, 2003). The system has many technical advantages: a high sensitivity, high specificity and wide dynamic range. Quantification of three different fluorophore molecules in each reaction tube is possible by using a newly developed software to calculate copies of HPV-DNA per cell. Identification and a viral load estimate of HPV types in a reaction involving other types is reliable as long as it represents at least 1–10% of the amount of the main HPV type (Moberg et al, 2003). The sensitivity of the assay decreased when the ratio between the types of HPV was less than 1 : 100. Furthermore, several techniques for analysis of HPV are available, causing variations with respect to both sensitivity and specificity. Although the linear dynamic range of the method was certified only down to 100 copies HR-HPV per cell equivalent (Moberg et al, 2003), compared to the five copies described by Gravitt et al (2003), quantification was also possible below that level. However, these figures should be regarded as approximative. We compared two extraction methods the MagNA pure system (Roche) and a Qiagen spin column kit (Qiagen). We found that the MagNA pure kit was more sensitive and provided the highest DNA yields from the material.
By using the Quantovir test, we identified five different oncogenic types of HPV (16, 31, 18/45, 33, 39) in our material. As could be expected, the oncogenic HPV 16 predominated at all stages of CIN: 20, 28 and 46% at CIN I, II and III, respectively. The most obvious findings were that HPV types 31 and 39 did not occur more frequently in higher degrees of CIN, and that the frequency (23%) of the HPV 33 group in the biopsies from patients with CIN II seemed almost as high as that for HPV 16. In previous studies, in which the sensitive PCR technique for detection and typing of HPV DNA was used, it was reported that HPV 16 is the most common type, followed by types 31 and 18. Even in a general population of 32–38-year-old healthy women, HPV 16 is the most prevalent type (2.2%) (Forslund et al, 2002).
Earlier studies have described the relative frequency of the most common oncogenic types of HPV in pre-invasive cervical lesions and cervical carcinoma. Our results demonstrated a predominance of HPV 16, followed by HPV 33. However, it is also of importance to identify the less prevalent and rare types of HPV in different pre-invasive lesions since the types of HPV identified may vary geographically.
Several studies have published reports investigating viral load's association with risk for cervical cancer and its precursors. The majority use HCII to measure viral load, and while some find viral load to be positively associated with increased risk for prevalent or incident disease (Sun et al, 2001, 2002; Dalstein et al, 2003) others do not (Lorincz et al, 2002; Sherman et al, 2002). Recent studies employing quantitative PCR to estimate HPV load show association between viral load and prevalent or incident disease more consistently (Ylitalo et al, 2000; Gravitt et al, 2003; Schlecht et al, 2003). Considerable viral-load variation has been observed within histopathological grades of the disease (Swan et al, 1999), making it hard to define uniform cutoff values. In addition, viral loads have been reported to be associated with lesion size rather than lesion severity.
It is noteworthy that in our study this is the first time that viral load of HR-HPV has been estimated in a systematic manner in CIN I–III lesions. As we expected and as previous studies have shown, there was a wide range of viral load values over several magnitudes, regardless of CIN grade (Peitsaro et al, 2002), but the average of copies of HR-HPV per cell were not significantly different in the CIN I, II and III cases (8, 17 and 6, respectively). The same was found also for the separately calculated values of HPV 16. The results might be influenced by the sample material, which was paraffin-embedded, formaldehyde-fixed biopsies. In general, it is difficult to obtain high DNA yields from such material as compared with fresh biopsies.
In accordance with a previous publication (Peitsaro et al, 2002), integration was detected at all stages of CIN. A real-time PCR-based integration assay was employed, where specific primers and probes directed to a unique region of E2 ORF and E6 ORF, respectively, were used. The hinge region of E2 ORF, which is most often deleted during HPV 16 integration into the host genome (Kalantari et al, 1998), was selected to use as target to design E2 primers and probes.
Our results showed that all HPV 16 cases (totally 48) were found to contain integrated virus genome. However, there was a higher proportion of cases with complete integration at the CIN III grade (nine cases) than at CIN I and II (2 and 1 cases); the average ratio of (copy numbers of E2 gen/copy numbers of E6 gen) was not significantly different in the three CIN grades. The reason could be, for instance, the limited number of samples (48 samples), or the episomal signal could arise from border areas of the biopsy that are not yet malignant. If a microdissection could be performed, to select only the parts of the biopsy with clear malignant properties, it is possible that the difference in the integrated/episomal ratio would be more significant.
As we expected, there was a significantly higher number of CIN III samples showing very low levels of episomal compared to integrated form (<1/100), than for the other CIN grades.
A combination of organised and opportunistic screening has reduced the incidence of squamous carcinoma substantially during the last decades in Sweden (Mählck et al, 1994; Ponten et al, 1995). In several studies, the Pap smear has been shown to have a high false-negative rate (Macgregor et al, 1994). A review of evidence-based data revealed that as many as 50% of precancerous cervical lesions may be missed by a single Pap test (Sherman et al, 1994). Another drawback of cervical cytology is its high false-positive rate (Sherman et al, 1994). Kinney et al (1998) showed that only 30% of women with histologically confirmed high-grade disease had corresponding atypia in their Pap smears. Studies have shown that 15–28% of HPV-DNA-positive women with normal cytology develop CIN within 2 years, compared with only 1–3% of HPV-DNA negative women (Schiffman and Castle, 2003). Against this background, a new screening strategy for cervical cancer has been presented in which HPV testing is combined with cytological examinations (Walboomers et al, 1999). In addition, the abundance of transient infections and lack of treatment for HPV infections make it impractical to follow up all infected individuals. HPV testing was identified to have higher sensitivity and equal specificity compared to repeated Pap smear collection as a triage for CIN II–III (Andersson et al, 2004). Viral load and integration have been proposed, as ways of increasing the specificity of HPV tests. Based on others results (Ylitalo et al, 2000; Moberg et al, 2004), women infected with a high viral load of HPV 16 are at increased risk of developing cervical carcinoma in situ already several years before diagnosis, compared to women infected with a low viral dose. Viral load mainly seems to have relevance for HPV 16-related tumours. By using quantitative methods to measure HPV viral load, we probably have a sensitive tool to identify women of over-risk for cervical carcinoma. This would have important applications for the cervical screening. Prospective randomised studies including quantitative HPV testing are needed on fresh material.
Vaccines emerging today are directed mainly against HPV 16 and 18. Even if vaccines were expanded to cover HPV 31 and 45, they would still only prevent 80% of cervical cancers worldwide. HPV vaccination is likely to significantly reduce HPV infection and cervical cancer burden, but the need for screening of some form is likely to remain in the foreseeable future.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Andersson S, Dillner L, Elfgren K, Mints M, Persson M, Rylander E (2004) A comparison of the HPV test and Pap smear as a second screening method for women with minor cytological abnormalities. Acta Obstet Gynecol Scand (in press)
Bosch FX, Manos MM, Munoz N, Sherman M, Jansen AM, Peto J, Schiffman MH, Moreno V, Kurman R, Shah KV (1995) Prevalence of human papillomavirus in cervical cancer: a worldwide perspective. International Biological Study on Cervical Cancer (IBSCC) Study Group. J Natl Cancer Inst 87: 796–802
Bosch FX, Munoz N (2002) The viral etiology of cervical cancer. Virus Res 89: 183–190
Dalstein V, Riethmuller D, Pretet JL, Le Bail Carval K, Sautiere JL, Carbillet JP, Kantelip B, Schaal JP, Mougin C (2003) Persistence and load of high-risk HPV are predictors for development of high-grade cervical lesions: a longitudinal French cohort study. Int J Cancer 106: 396–403
Davidson M, Schnitzer PG, Bulkow LR, Parkinson AJ, Schloss ML, Fitzgerald MA, Knight JA, Murphy CM, Kiviat NB, Toomey KE (1994) The prevalence of cervical infection with human papillomaviruses and cervical dysplasia in Alaska Native women. J Infect Dis 169: 792–800
Forslund O, Antonsson A, Edlund K, van den Brule AJ, Hansson BG, Meijer CJ, Ryd W, Rylander E, Strand A, Wadell G, Dillner J, Johansson B (2002) Population-based type-specific prevalence of high-risk human papillomavirus infection in middle-aged Swedish women. J Med Virol 66: 535–541
Gravitt PE, Burk RD, Lorincz A, Herrero R, Hildesheim A, Sherman ME, Bratti MC, Rodriguez AC, Helzlsouer KJ, Schiffman M (2003) A comparison between real-time polymerase chain reaction and hybrid capture 2 for human papillomavirus DNA quantitation. Cancer Epidemiol Biomarkers Prev 12: 477–484
Ho GY, Bierman R, Beardsley L, Chang CJ, Burk RD (1998) Natural history of cervicovaginal papillomavirus infection in young women. N Engl J Med 338: 423–428
Jacobs MV, Walboomers JM, Snijders PJ, Voorhorst FJ, Verheijen RH, Fransen-Daalmeijer N, Meijer CJ (2000) Distribution of 37 mucosotropic HPV types in women with cytologically normal cervical smears: the age-related patterns for high-risk and low-risk types. Int J Cancer 87: 221–227
Josefsson AM, Magnusson PK, Ylitalo N, Sorensen P, Qwarforth-Tubbin P, Andersen PK, Melbye M, Adami HO, Gyllensten UB (2000) Viral load of human papilloma virus 16 as a determinant for development of cervical carcinoma in situ: a nested case–control study. Lancet 355: 2189–2193
Kalantari M, Blennow E, Hagmar B, Johansson B (2001) Physical state of HPV16 and chromosomal mapping of the integrated form in cervical carcinomas. Diagn Mol Pathol 10: 46–54
Kalantari M, Karlsen F, Kristensen G, Holm R, Hagmar B, Johansson B (1998) Disruption of the E1 and E2 reading frames of HPV 16 in cervical carcinoma is associated with poor prognosis. Int J Gynecol Pathol 17: 146–153
Kinney WK, Manos MM, Hurley LB, Ransley JE (1998) Where's the high-grade cervical neoplasia? The importance of minimally abnormal Papanicolaou diagnoses. Obstet Gynecol 91: 973–976
Lazo PA (1997) Papillomavirus integration: prognostic marker in cervical cancer? Am J Obstet Gynecol 176: 1121–1122
Lorincz AT, Castle PE, Sherman ME, Scott DR, Glass AG, Wacholder S, Rush BB, Gravitt PE, Schussler JE, Schiffman M (2002) Viral load of human papillomavirus and risk of CIN3 or cervical cancer. Lancet 360: 228–229
Macgregor JE, Campbell MK, Mann EM, Swanson KY (1994) Screening for cervical intraepithelial neoplasia in north east Scotland shows fall in incidence and mortality from invasive cancer with concomitant rise in preinvasive disease. BMJ 308: 1407–1411
Mählck C, Jonsson H, Lenner P (1994) Pap smear screening and changes in cervical cancer mortality in Sweden. Int J Gynecol Obstet 44: 267–272
Moberg M, Gustavsson I, Gyllensten U (2003) Real-time PCR-based system for simultaneous quantification of human papillomavirus types associated with high risk of cervical cancer. J Clin Microbiol 41: 3221–3228
Moberg M, Gustavsson I, Gyllensten U (2004) Type-specific associations of human papillomavirus load with risk of developing cervical carcinoma in situ. Int J Cancer 112: 854–859
Moberg M, Gustavsson I, Wilander E, Gyllensten U (2005) High viral loads of human papillomavirus predict risk of invasive cervical carcinoma. Br J Cancer 92: 891–894
Munoz N, Bosch FX, de Sanjose S, Herrero R, Castellsague X, Shah KV, Snijders PJ, Meijer CJ (2003) Epidemiologic classification of human papillomavirus types associated with cervical cancer. N Engl J Med 348: 518–527
Nobbenhuis MA, Walboomers JM, Helmerhorst TJ, Rozendaal L, Remmink AJ, Risse EK, van der Linden HC, Voorhorst FJ, Kenemans P, Meijer CJ (1999) Relation of human papillomavirus status to cervical lesions and consequences for cervical-cancer screening: a prospective study. Lancet 354: 20–25
Peitsaro P, Johansson B, Syrjanen S (2002) Integrated human papillomavirus type 16 is frequently found in cervical cancer precursors as demonstrated by a novel quantitative real-time PCR technique. J Clin Microbiol 40: 886–891
Ponten J, Adami HO, Friberg LG, Gustafsson L, Miller AB, Parkin M, Sparen P, Trichopoulos D (1995) HPV and cervical cancer. Int J Cancer 63: 317
Romanczuk H, Howley PM (1992) Disruption of either the E1 or the E2 regulatory gene of human papillomavirus type 16 increases viral immortalization capacity. Proc Natl Acad Sci USA 89: 3159–3163
Schiffman MH, Bauer HM, Hoover RN, Glass AG, Cadell DM, Rush BB, Scott DR, Sherman ME, Kurman RJ, Wacholder S (1993) Epidemiologic evidence showing that human papillomavirus infection causes most cervical intraepithelial neoplasia. J Natl Cancer Inst 85: 958–964
Schiffman MH, Castle P (2003) Epidemiologic studies of a necessary causal risk factor: human papillomavirus infection and cervical neoplasia. J Natl Cancer Inst 95: E2
Schlecht NF, Trevisan A, Duarte-Franco E, Rohan TE, Ferenczy A, Villa LL, Franco EL (2003) Viral load as a predictor of the risk of cervical intraepithelial neoplasia. Int J Cancer 103: 519–524
Sherman ME, Schiffman M, Cox JT (2002) Effects of age and human papilloma viral load on colposcopy triage: data from the randomized Atypical Squamous Cells of Undetermined Significance/Low-Grade Squamous Intraepithelial Lesion Triage Study (ALTS). J Natl Cancer Inst 94: 102–107
Sherman ME, Schiffman MH, Lorincz AT (1994) Toward objective quality assurance in cervical cytopathology: correlation of cytopathologic diagnosis with detection of high-risk human papillomavirus types. Am J Clin Pathol 102: 182–187
Soutter WP, Fletcher A (1994) Invasive cancer of the cervix in women with mild dyskaryosis followed up cytologically. BMJ 308: 1421–1423
Sun CA, Lai HC, Chang CC, Neih S, Yu CP, Chu TY (2001) The significance of human papillomavirus viral load in prediction of histologic severity and size of squamous intraepithelial lesions of uterine cervix. Gynecol Oncol 83: 95–99
Sun CA, Liu JF, Wu DM, Nieh S, Yu CP, Chu TY (2002) Viral load of high-risk human papillomavirus in cervical squamous intraepithelial lesions. Int J Gynaecol Obstet 76: 41–47
Swan DC, Tucker RA, Tortolero-Luna G, Mitchell MF, Wideroff L, Unger ER, Nisenbaum RA, Reeves WC, Icenogle JP (1999) Human papillomavirus (HPV) DNA copy number is dependent on grade of cervical disease and HPV type. J Clin Microbiol 37: 1030–1034
Walboomers JM, Jacobs MV, Manos MM, Bosch FX, Kummer JA, Shah KV, Snijders PJ, Peto J, Meijer CJ, Munoz N (1999) Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol 189: 12–19
Ylitalo N, Sorensen P, Josefsson AM, Magnusson PK, Andersen PK, Ponten J, Adami HO, Gyllensten UB, Melbye M (2000) Consistent high viral load of human papillomavirus 16 and risk of cervical carcinoma in situ: a nested case–control study. Lancet 355: 2194–2198
Acknowledgements
We wish to thank Carmen Flores-Staino for technical assistance. We are grateful to Quantovir AB for their gift of HPV kits used in this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Andersson, S., Safari, H., Mints, M. et al. Type distribution, viral load and integration status of high-risk human papillomaviruses in pre-stages of cervical cancer (CIN). Br J Cancer 92, 2195–2200 (2005). https://doi.org/10.1038/sj.bjc.6602648
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6602648
Keywords
This article is cited by
-
A multiplex RPA-CRISPR/Cas12a-based POCT technique and its application in human papillomavirus (HPV) typing assay
Cellular & Molecular Biology Letters (2024)
-
Increased expression of HPV-E7 oncoprotein correlates with a reduced level of pRb proteins via high viral load in cervical cancer
Scientific Reports (2023)
-
Immunohistochemistry and real-time PCR as diagnostic tools for detection of Borrelia burgdorferi sensu lato in ticks collected from humans
Experimental and Applied Acarology (2016)
-
Human papillomavirus prevalence in South African women and men according to age and human immunodeficiency virus status
BMC Infectious Diseases (2015)
-
The DNA load of six high-risk human papillomavirus types and its association with cervical lesions
BMC Cancer (2015)