Abstract
We analysed the 5-year relative survival among 4473 breast cancer cases diagnosed in 1990–1992 from cancer registries in Estonia, France, Italy, Spain, the Netherlands and the UK. Among eight categories based on ICD-O codes (infiltrating ductal carcinoma, lobular plus mixed carcinoma, comedocarcinoma, ‘special types’, medullary carcinoma, not otherwise specified (NOS) carcinoma, other carcinoma and cancer without microscopic confirmation), the 5-year relative survival ranged from 66% (95% CI 61–71) for NOS carcinoma to 95% (95% CI 90–100) for special types (tubular, apocrine, cribriform, papillary, mucinous and signet ring cell); 27% (95% CI 18–36) for cases without microscopic confirmation. Differences in 5-year relative survival by tumor morphology and hormone receptor status were modelled using a multiple regression approach based on generalised linear models. Morphology and hormone receptor status were confirmed as significant survival predictors in this population-based study, even after adjusting for age and stage at diagnosis.
Similar content being viewed by others
Main
Tumour morphology and hormone receptor status are established predictors of breast cancer survival (Ruder et al, 1989; Northridge et al, 1997; Early Breast Cancer Trialists' Collaborative Group, 1998; Li et al, 2003). Detailed stage information is seldom available in population-based studies and few have assessed the influence of both these groups of predictors on prognosis using appropriate statistical methods (Northridge et al, 1997; Li et al, 2003).
The EUROCARE high-resolution studies, which are principally concerned with interpreting regional differences in survival, also provide population-based information on biological prognostic factors, such as tumour morphology and hormone receptor status, as well as information on stage, diagnostic investigations and therapy. Using such data, the present study aimed to examine, at the population level, the influence of morphology and hormone receptor status on breast cancer survival, adjusting by disease stage and age at diagnosis.
Material and methods
We analysed data on a representative sample of 4478 breast cancer patients investigated in previous EUROCARE high-resolution studies on breast cancer (Sant, 2001; Sant et al, 2003). All had primary invasive breast cancer diagnosed in 1990–1992 in the territories of 17 population-based cancer registries in six countries: Estonia (national registry); France (Bas-Rhin, Calvados, Côte d'Or, Doubs, Hérault, Isère, Somme, and Tarn); Italy (Firenze, Modena, Ragusa and Varese); Spain (Granada); the Netherlands (Eindhoven) and the UK (Mersey and Thames). Details of the study design and sampling have been published (Sant, 2001). At least 5 years of follow-up was available for all women. Each registry used its own follow-up procedures. The UK registries updated the life status of patients included in this study by linking death certificates to the registry records; all other registries actively ascertained the life status of cases from various sources of information (e.g. registry of general practitioners, municipality files).
Detailed information on stage, diagnostic examinations and treatment was collected according to a standardised protocol (Sant, 2001). Most of the information required was obtained from patients' clinical records. However, in some cases these were incomplete, and other records had to be examined (e.g. pathology reports and discharge records).
ICD-O classification (Percy et al, 1990) was available for all cases. A total of 4473 cases were included in the morphology analysis after excluding five erroneously classified cases (Table 1). Based on the ICD-O code, we grouped the cases into the following eight categories: infiltrating ductal carcinoma, lobular plus mixed carcinoma, comedocarcinoma, the so-called special types (77 tubular, five apocrine, 20 cribriform, 27 papillary, 77 mucinous and five signet ring cell carcinoma) (Tavassoli and Devilee, 2003), medullary carcinoma, not otherwise specified (NOS) carcinoma, other carcinoma (trabecular, acinar, squamous, small cell, pilomatrix, transitional carcinoma, lymphoepithelioma and carcinoid) and cancer without microscopic confirmation.
Oestrogen and progesterone receptor status was classified into five categories: negative, positive, test performed with unknown result, test not performed and unknown whether performed or not. Receptor status, in particular whether positive or negative, was determined directly from the clinical record: absolute values were not required by the study protocol.
Tumours were staged according to TNM rules (3rd edition) (Spiessel et al, 1992). Pathological T and N categories were used for women who underwent surgery; clinical T, N and M categories used for women not treated surgically (approximately 10%). We categorised tumour stage as follows: T1N0M0, T2-3N0M0, T1-3N+M0, T4 M0, M1 and stage not specified.
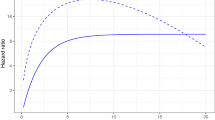
Relative survival (5-year) was calculated by the Hakulinen method (Hakulinen, 1982; Hakulinen and Abeywickrama, 1985) with 95% confidence intervals (CI) calculated from the standard error according to Greenwood's (1926) method. Relative survival is an estimate of the probability of cancer survival after adjusting for competing causes of death determined from general population life tables for women, specific for each country or registry.
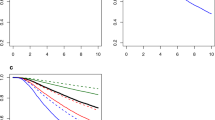
Differences in 5-year relative survival by tumour morphology and hormone receptor status were modelled with a recently developed multiple regression approach based on generalised linear models and adopting the Poisson assumption for the observed number of deaths (Dickman et al, 2004). The relative excess risks (RERs) derived from these models quantify the extent to which the hazard of death in a given group differs from that in the reference category, after taking into account the background risk of death in the general population of each country or region. The multivariable analyses only included cases from registries with hormone receptor status available for ⩾60% of operated cases (2346 women; 52% of total). Cases from the registries of Firenze (Florence), Somme, Granada, Mersey, Thames, Eindhoven and Estonia were excluded (Table 1).
Age at diagnosis was categorised into <40 years, 40–49, 50–59 (reference category) and 60 years or over. Hormone receptor status was grouped into four categories: both positive (ER+ PGR+), both negative (ER− PGR−), tests performed with one positive result (ER+ or PGR+) and cases with test not performed or result unknown. All calculations were carried out using the Stata statistical package (Stata Corporation, 2001).
Results
Table 1 shows the total number of cases by registry together with morphology and hormone receptor status and other indicators of data completeness and quality. Overall 97% of cases were microscopically confirmed (range 89–99%) and 90% were treated surgically (range 74–95%). Infiltrating ductal carcinoma and NOS carcinoma accounted for 69 and 7% of the surgically treated cases, respectively, with conspicuous variation across registries (36–82% and 0–54%, respectively). Oestrogen receptor status was available in 60% of operated cases (range 0–89%) and progesterone receptor status was available in 54% of operated cases (range 0–85%).
Table 2 shows the 5-year relative survival by morphology group, for all cases. The largest morphological categories were infiltrating ductal carcinoma (65%), lobular or mixed carcinoma (12%) and NOS carcinoma (10%). The other categories contained many fewer cases. Of all cases, 3% were not confirmed microscopically.
The 5-year relative survival was 81% (95% CI 80–82) for infiltrating ductal carcinoma, 87% for comedocarcinoma (95% CI 80–94), 86% for lobular or mixed carcinoma (95% CI 82–90) and 86% for medullary carcinoma (95% CI 76–96). The special types category had the greatest survival (95%; 95% CI 90–100), NOS carcinoma had the second lowest survival (66%; 95% CI 61–71) and cases without microscopic confirmation the lowest survival (27%; 95% CI 18–36).
Table 3 shows hormone receptor status in 2346 cases from a subset of 10 registries with this information available for ⩾60% of operated women, together with mean age at diagnosis and 5-year relative survival. A total of 1222 (52%) of these women had oestrogen-positive cancers, 1091 (47%) had progesterone-positive cancers. More specifically, 980 (42%) had both oestrogen- and progesterone-positive tumours, while 393 (17%) were negative for both oestrogen and progesterone receptors (see Table 4). The mean age of women with oestrogen-positive cancers was slightly greater than for those with oestrogen-negative cancers, but did not differ between those with progesterone-negative and progesterone-positive tumours.
Women with oestrogen receptor-positive disease had better survival (90%; 95% CI 88–92) than those with oestrogen receptor-negative disease (77%; 95% CI 73–81). Similarly, women with progesterone receptor-positive disease had better survival (90%; 95% CI 88–92) than those with progesterone receptor-negative disease (79%; 95% CI 75–83). Women for whom information on receptor status was not available had intermediate 5-year relative survival (86%, 95% CI 82–90). The survival of patients with both receptors positive was 90% (95% CI 87–93) compared to 73% (95% CI 68–78) for those with both receptors negative (data not shown).
Table 4 shows tumour morphology in relation to positive hormone receptor status for the cases with available information on oestrogen (n=1731) or progesterone status (n=1704) from the 10 registries, with information available in 60% or more of operated cases. The lobular plus mixed carcinoma category had the highest proportions of cases with positive receptor status (82% for oestrogen and 70% for progesterone), while the medullary carcinoma category had the lowest proportions with positive receptors (26% for oestrogen and 35% for progesterone). In the other morphologic groups, the proportions ranged from 48 to 71% for oestrogen and from 50 to 67% for progesterone.
For most morphologic categories, the proportion with positive oestrogen receptors was higher than the proportion with positive progesterone receptors, exceptions being comedocarcinoma and medullary carcinoma.
Table 5 shows the results of the multivariable regression analysis to determine the RERs of death for morphologic group, age, stage at diagnosis and hormone receptor status, in each case taking into account the influence of the other variables.
Comedocarcinoma, (0.34, 95% CI 0.12–0.98), special types (0.35, 95% CI 0.12–0.99) and lobular and mixed carcinoma (0.58, 95% CI 0.37–0.91) had lower RERs of death than infiltrating ductal carcinoma (reference category). For the other carcinomas category, the RER (1.38, 95% CI 0.72–2.63) was about 40% higher and for the medullary carcinoma category the RER (1.19, 95% CI 0.49–2.85) was about 20% higher than reference; the RER for NOS carcinoma was 1.08 (95% CI 0.68–1.71). With respect to age, the 40–49 year age group had the lowest RER of death (0.71, 95% CI 0.49–1.02) compared to the 50–59 year reference category. With respect to tumour stage, RERs increased with advancing stage and in all cases were significantly higher than reference (T1N0M0). Unspecified stage cancers had an intermediate RER.
Women positive for both hormone receptors (ER+ PGR+) had a significantly lower RER of death (0.32, 95% CI 0.24–0.43) than those negative for both receptors (ER− PGR−, reference). A positive result for one receptor (ER+ or PGR+) was also significantly protective compared to reference (0.41; 0.28–0.62). Women with receptors not determined or with unknown result had an intermediate RER (0.49, 95% CI 0.35–0.67). In a separate analysis of the only ER+ and only PGR+ groups, RERs were 0.39 (95% CI 0.24–0.62) and 0.51 (95% CI 0.27–0.97), respectively, compared to the ER- PGR- reference (data not shown).
We also tested the two-way interactions: morphology and stage, morphology and age, morphology and registry, hormone receptor status and registry. None of these interactions was statistically significant.
Discussion
As in previous population-based and clinical studies (Ruder et al, 1989; Northridge et al, 1997; Early Breast Cancer Trialists' Collaborative Group, 1998; Li et al, 2003), tumour morphology and hormone receptor status are important predictors of breast cancer survival. The 5-year survival varied from 66% for NOS carcinoma to 95% for special type tumours, while patients with oestrogen- and progesterone-positive tumours had better survival (90%) than those negative for both receptors (73%). Morphology and receptor status remained significant survival predictors after adjusting for age and stage at diagnosis.
A strength of our study is that it is population-based (covering all the cases in registry populations) and is therefore not susceptible to the selection bias of clinical series. Detailed stage at diagnosis not usually available in population-based studies and age were taken account of in analysing the prognostic effects of morphology and receptor status.
Previous studies on the present data set analysed the effect of tumour stage on survival (Sant et al, 2003, 2004). We used this detailed stage information – available in 92% of cases – to adjust for stage in the multivariable analysis of prognostic effects of morphology and receptor status. Although stage depends on the number of axillary nodes examined, this number was similar for each morphological group; thus, inclusion of number of nodes examined in the model had little effect on the results (data not shown).
Another strength of the study is that the effects of competing causes of death were controlled for by estimating the relative survival. Population-based studies on the SEER database, which analysed the relative risk of breast cancer death according to tumour morphology, did not estimate survival in this way. One of these (Li et al, 2003) did not control for competing causes of death; the other (Northridge et al, 1997) used cause-specific survival to control for competing causes of death. It is also important to note that only summary information on stage was available in these studies (categories: localised disease, regional metastasis, distant metastasis and unstaged) and the models did not adjust for hormone receptor status.
Information on tumour morphology was satisfactorily complete in the present study (97% of diagnoses confirmed microscopically). The morphology categories special type and comedocarcinoma were associated with lower RERs of death than infiltracting ductal carcinoma (Table 5). The special type category includes, tubular, mucinous and papillary histotypes, which were reported to have good prognoses in a previous population-based study (Li et al, 2003), and in other studies (Cooper et al, 1978; Fisher et al, 1980; Wargotz and Silverberg, 1988; Ellis et al, 1992; Silverstein et al, 1994; Pedersen et al, 1995; Reinfuss et al, 1995; Toikkanen et al, 1997; Diab et al, 1999). Comedocarcinoma also had a relatively good prognosis in a previous study (Li et al, 2003). As expected, the categories other and NOS carcinoma had the lowest survival in our study.
Adjustment for age and stage had only limited effects on RERs for each morphologic category; in particular, rank did not change. However, comedocarcinoma, other and NOS carcinoma were generally diagnosed at a more advanced stage than other morphologic categories, and their RERs decreased from 0.55 to 0.34, from 1.57 to 1.38 and from 1.16 to 1.08, respectively, after these adjustments (data not shown). The overall proportion of NOS carcinomas was 7%, compared to 5% in the US SEER populations (Northridge et al, 1997).
A possible weakness of our study is that the morphologic diagnoses may not be entirely comparable between registries, as is suggested by the fact that, although all registries coded tumour morphology using ICD-O, the proportion of NOS carcinomas varied considerably between registries (Table 1), indicating that the quality of morphology data also varied. Thus, in Firenze, the proportions of NOS and infiltrating ductal carcinoma were strikingly low because pathologists systematically search for lobular or other components, so that a proportion of these cases are classified as mixed (lobular plus ductal) or special type carcinoma. Only one registry with a high proportion of NOS carcinomas (Herault, 39%) was included in the multivariable analysis, while the average proportion of NOS carcinomas in the other nine registries was around 2%. To identify misclassification in morphology coding, we looked for an interaction between morphology and registry, but found none. In addition, sensitivity analyses excluding Herault and Somme did not produce substantial changes in morphology RERs. We grouped tubular, apocrine, cribriform, papillary and mucinous carcinomas into the special type category because of their small numbers and because all had similarly favourable survival. Larger studies may be able to assign meaningful individual RERs to these rarer histotypes.
We are aware of no other studies that considered the prognostic influence of receptor status on the prognostic effect of morphology. Receptor status is not usually available to cancer registries, and for various reasons registries may not be able to obtain this information systematically. The percentage of our cases with known receptor status was lower than reported elsewhere (Early Breast Cancer Trialists' Collaborative Group, 1998; Chu et al, 2001; Chu and Anderson, 2002; Colditz et al, 2004). To enhance its reliability, our analysis was confined to registries with receptor status information available in at least 60% of cases. In these registries, the proportions of cases positive for oestrogen and progesterone receptors were similar to those of these other studies.
It is relevant that we do not know the criteria for deciding whether a tumour was receptor positive or negative, or to what extent these were uniform across our registry areas, a problem that has been addressed elsewhere (Chapman et al, 1993, 1996). We decided to collect the results as positive or negative. However, this may have reduced accuracy, as we did not have the absolute values against which to check the positive/negative result. To mitigate this problem, we erected four particular categories: ER+ plus PGR+; ER− plus PGR−; either ER+ or PGR+ (with the other result very often not known); and ‘other’ (cases with status unavailable or unreliable). The first two categories are likely to contain the least errors. As expected, ER+ plus PGR+ cases had better prognoses than ER− plus PGR− cases; either ER+ or PGR+ cases also had good prognoses, but less so than cases with both receptors present. The RER of death for the ‘other’ category was intermediate, suggesting that it contained considerable numbers of women whose tumours were receptor positive. Like those for morphology, RERs for receptor status did not change substantially when adjusted by stage and morphology (not shown).
We did not include tamoxifen treatment in the multivariable analysis, as information was incomplete, being often prescribed during follow-up, and not entered on the primary treatment record. However, we did analyse tamoxifen in all ER+ women, since for most of these hormone treatment information was available. Tamoxifen was found to be associated with a 10% reduction in the RER of death compared with ER+ women not prescribed the drug (results not presented) – a figure consistent with reductions reported elsewhere (Early Breast Cancer Trialists' Collaborative Group, 1998). We note that women in the 40–49 age class (predominantly premenopausal) had the lowest RER of death, consistent with previous findings (Langlands and Kerr, 1979; Adami et al, 1986; Sant et al, 2003).
Our analysis has shown that EUROCARE high-resolution studies are able to provide information on biological tumour characteristics at the level of the population, in addition to their principal aim of explaining regional and temporal survival differences. It is important to continue efforts to improve the completeness and quality of the data collected by population-based cancer registries.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Adami HO, Malker B, Holmberg L, Persson I, Stone B (1986) The relation between survival and age at diagnosis in breast cancer. N Engl J Med 315: 559–563
Chapman JA, Mobbs BG, Hanna WM, Sawka CA, Pritchard KI, Lickley HL, Trudeau ME, Ryan ED, Ooi TC, Sutherland DJ (1993) The standardization of estrogen receptors. J Steroid Biochem Mol Biol 45: 367–373
Chapman JW, Mobbs BG, McCready DR, Lickley HL, Trudeau ME, Hanna W, Kahn HJ, Sawka CA, Fish EB, Pritchard KI (1996) An investigation of cut-points for primary breast cancer oestrogen and progesterone receptor assays. J Steroid Biochem Mol Biol 57: 323–328
Chu KC, Anderson WF (2002) Rates for breast cancer characteristics by estrogen and progesterone receptor status in the major racial/ethnic groups. Breast Cancer Res Treat 74: 199–211
Chu KC, Anderson WF, Fritz A, Ries LA, Brawley OW (2001) Frequency distributions of breast cancer characteristics classified by estrogen receptor and progesterone receptor status for eight racial/ethnic groups. Cancer 92: 37–45
Colditz GA, Rosner BA, Chen WY, Holmes MD, Hankinson SE (2004) Risk factors for breast cancer according to estrogen and progesterone receptor status. J Natl Cancer Inst 96: 218–228
Cooper HS, Patchefsky AS, Krall RA (1978) Tubular carcinoma of the breast. Cancer 42: 2334–2342
Diab SG, Clark GM, Osborne CK, Libby A, Allred DC, Elledge RM (1999) Tumor characteristics and clinical outcome of tubular and mucinous breast carcinomas. J Clin Oncol 17: 1442–1448
Dickman PW, Sloggett A, Hills M, Hakulinen T (2004) Regression models for relative survival. Stat Med 23: 51–64
Early Breast Cancer Trialists' Collaborative Group (1998) Tamoxifen for early breast cancer: an overview of the randomised trials. Lancet 351: 1451–1467
Ellis IO, Galea M, Broughton N, Locker A, Blamey RW, Elston CW (1992) Pathological prognostic factors in breast cancer. II. Histological type. Relationship with survival in a large study with long-term follow-up. Histopathology 20: 479–489
Fisher ER, Palekar AS, Redmond C, Barton B, Fisher B (1980) Pathologic findings from the National Surgical Adjuvant Breast Project (protocol no. 4). VI. Invasive papillary cancer. Am J Clin Pathol 73: 313–322
Greenwood M (1926) The Errors of Sampling of the Survivorship Table, Vol. 33 of Reports on Public Health and Medical Subjects. London: Her Majesty's Stationery Office
Hakulinen T (1982) Cancer survival corrected for heterogeneity in patient withdrawal. Biometrics 38: 933–942
Hakulinen T, Abeywickrama KH (1985) A computer program package for relative survival analysis. Comput Programs Biomed 19: 197–207
Langlands AO, Kerr GR (1979) Prognosis in breast cancer: the effect of age and menstrual status. Clin Oncol 5: 123–133
Li CI, Moe RE, Daling JR (2003) Risk of mortality by histologic type of breast cancer among women aged 50 to 79 years. Arch Intern Med 163: 2149–2153
Northridge ME, Rhoads GG, Wartenberg D, Koffman D (1997) The importance of histologic type on breast cancer survival. J Clin Epidemiol 50: 283–290
Pedersen L, Zedeler K, Holck S, Schiodt T, Mouridsen HT (1995) Medullary carcinoma of the breast. Prevalence and prognostic importance of classical risk factors in breast cancer. Eur J Cancer 31A: 2289–2295
Percy C, Van Holten V, Muir C (1990) International Classification of Diseases for Oncology, 2nd edn. Geneva: WHO
Reinfuss M, Stelmach A, Mitus J, Rys J, Duda K (1995) Typical medullary carcinoma of the breast: a clinical and pathological analysis of 52 cases. J Surg Oncol 60: 89–94
Ruder AM, Lubin F, Wax Y, Geier A, Alfundary E, Chetrit A (1989) Estrogen and progesterone receptors in breast cancer patients. Epidemiologic characteristics and survival differences. Cancer 64: 196–202
Sant M (2001) Differences in stage and therapy for breast cancer across Europe. Int J Cancer 93: 894–901
Sant M, Allemani C, Berrino F, Coleman MP, Aareleid T, Chaplain G, Coebergh JW, Colonna M, Crosignani P, Danzon A, Federico M, Gafà L, Grosclaude P, Hedelin G, Mace-Lesech J, Garcia CM, Moller H, Paci E, Raverdy N, Tretarre B, Williams EM (2004) Breast carcinoma survival in Europe and the United States. Cancer 100: 715–722
Sant M, Allemani C, Capocaccia R, Hakulinen T, Aareleid T, Coebergh JW, Coleman MP, Grosclaude P, Martinez C, Bell J, Youngson J, Berrino F (2003) Stage at diagnosis is a key explanation of differences in breast cancer survival across Europe. Int J Cancer 106: 416–422
Silverstein MJ, Lewinsky BS, Waisman JR, Gierson ED, Colburn WJ, Senofsky GM, Gamagami P (1994) Infiltrating lobular carcinoma. Is it different from infiltrating duct carcinoma? Cancer 73: 1673–1677
Spiessel B, Beahers OH, Hermanek P, Hutter RVP, Schieber O, Sobin LH, Wagner G (1992) UICC: TNM Atlas Classification of Malignant Tumours, 3rd edn. Berlin, Heidelberg, New York, London, Paris, Tokyo: Springer
Stata Corporation (2001) Stata Statistical Software: Release 7.0. College Station, TX: Stata Corporation
Tavassoli FA, Devilee P (2003) Tumours of the Breast and Female Genital Organs. WHO. Lyon: IARC Press
Toikkanen S, Pylkkanen L, Joensuu H (1997) Invasive lobular carcinoma of the breast has better short- and long-term survival than invasive ductal carcinoma. Br J Cancer 76: 1234–1240
Wargotz ES, Silverberg SG (1988) Medullary carcinoma of the breast: a clinicopathologic study with appraisal of current diagnostic criteria. Hum Pathol 19: 1340–1346
Acknowledgements
This study was supported by the European Union's BIOMED program. We thank Don Ward for help with the English, and Samba Sowe for secretarial assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Allemani, C., Sant, M., Berrino, F. et al. Prognostic value of morphology and hormone receptor status in breast cancer – a population-based study. Br J Cancer 91, 1263–1268 (2004). https://doi.org/10.1038/sj.bjc.6602153
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6602153
Keywords
This article is cited by
-
Outcomes of ovarian stimulation and fertility preservation in breast cancer patients with different hormonal receptor profiles
Journal of Assisted Reproduction and Genetics (2020)
-
Relative and disease-free survival for breast cancer in relation to subtype: a population-based study
Journal of Cancer Research and Clinical Oncology (2013)
-
Risk factors for uncommon histologic subtypes of breast cancer using centralized pathology review in the Breast Cancer Family Registry
Breast Cancer Research and Treatment (2012)
-
MALDI tissue imaging: from biomarker discovery to clinical applications
Analytical and Bioanalytical Chemistry (2011)
-
Histological type and grade of breast cancer tumors by parity, age at birth, and time since birth: a register-based study in Norway
BMC Cancer (2010)