Abstract
The DBCCR1 gene at chromosome 9q33 has been identified as a candidate tumour suppressor, which is frequently targeted by promoter hypermethylation in bladder cancer. Here, we studied the possible involvement of DBCCR1 in the development of oral squamous cell carcinoma. DNA from 34 tumours was examined for loss of heterozygosity (LOH) at three markers surrounding DBCCR1 and for hypermethylation of the DBCCR1 promoter, using methylation-specific PCR and methylation-specific melting-curve analysis. LOH was found in 10 of 31 cases (32%), and DBCCR1 hypermethylation was present in 15 of 34 cases (44%). Hypermethylation of DBCCR1 was also present in three of seven epithelial tissues adjacent to the tumours, including two hyperplastic and one histologically normal epithelia. Furthermore, of four oral leukoplakias with dysplasia, one showed LOH at 9q33 and two showed DBCCR1 hypermethylation. These data suggest that LOH at 9q33 and hypermethylation of the DBCCR1 promoter are frequent and possibly early events in oral malignant development.
Similar content being viewed by others
Main
Oral cancer comprises about 3% of all newly diagnosed cancer cases in the Western countries. Despite advances in therapy, the 5-year survival rate after diagnosis is still poor and remains ∼50% (Landis et al, 1999; Silverman, 2001). Clinically, oral carcinomas often develop in a two-step process. The first step is characterised by the appearance of potentially malignant lesions such as leukoplakias and erythroplakias, and the second step is characterised by the development of carcinomas. However, clinical and histopathological features are insufficient measures for predicting the prognosis of potentially malignant lesions (Warnakulasuriya, 2000, 2001). Furthermore, a recent study indicated that clinically and histologically normal mucosa adjacent to tumours may harbour patches of genetically altered cells (Braakhuis et al, 2003). It is, therefore, important to find molecular markers for identifying the minor fraction of oral lesions that will develop into carcinoma.
Loss of heterozygosity (LOH) at multiple chromosome regions and genetic and epigenetic alterations of several proto-oncogenes and tumour suppressor genes have been demonstrated in oral carcinomas, including alterations of the TP53, p16, p15, MGMT, E-cadherin genes and RAS (Califano et al, 1996; Partridge et al, 1999; Williams, 2000; Ogi et al, 2002; Viswanathan et al, 2003). In addition, our previous study showed that hypermethylation of the ABO gene promoter was associated with loss of expression of A/B antigen in approximately one-third of oral squamous cell carcinomas (Gao et al, 2004). LOH at 9q34, in which the ABO gene is located, was also a frequent event in these tumours. However, a number of tumours from AO and BO heterozygotes showed deletion of the O allele, which does not encode a functional glycosyltransferase, suggesting the existence of an additional tumour suppressor gene on chromosome 9q. The DBCCR1 (deleted in bladder cancer chromosomal region candidate 1) gene at chromosome 9q33 was identified as a putative tumour suppressor gene that is frequently targeted by hypermethylation in transitional cell carcinomas of the bladder (Habuchi et al, 1997, 1998, 2001; Nishiyama et al, 1999). There are, at present, no reports of DBCCR1 alterations in other cancers. The aim of this study was to examine for LOH at the 9q33 region and determine the methylation status of DBCCR1 in oral squamous cell carcinomas and potentially malignant oral lesions.
Materials and methods
Sample preparation
Surgical specimens of oral lesions were obtained from School of Dentistry, National Yang-Ming University, Taipei, and Odense University Hospital, Denmark. The median age of the patients was 60 years (range 35–89 years); there were six women and 32 men. The materials included unfixed frozen tissues from 34 patients with oral squamous cell carcinoma and four patients with potentially malignant lesions (leukoplakia with epithelial dysplasia). A laser microdissection system (PALM) was used to separate tumour cells or leukoplakia epithelium from normal connective tissue. In seven cases, tumour-adjacent epithelium was isolated as well. DNA was extracted by routine procedures using the DNeasy Kit (Qiagen). Informed consent and approval by the Ethics Committee were obtained according to Danish legislation.
LOH analysis
DNA from tumour or leukoplakia lesions and matched normal tissues was screened for LOH at the 9q33 region using the three microsatellite markers, D9S195, D9S1872 (http://www.gdb.org) and 9-11407. The latter marker was designed by one of us (HE) and is located ∼300 kb upstream of exon 1 of the DBCCR1 gene, according to GenBank accession no. AY438564. The primer sequences of 9-11407 were 5′-CAACAAAGTCAATCCCAGCA-3′ and 5′-GGTTCACTAAGAGCACAATTGTTTA-3′. PCR was performed using a 33P end-labelled primer, and the amplified fragments were separated by electrophoresis in a 6% denaturing polyacrylamide gel, as described elsewhere (Gao et al, 2004). LOH was determined as at least a 50% reduction in the relative intensity of one allele compared with the normal control. Control samples were included during all procedures.
Methylation analysis
Genomic DNA was treated with sodium bisulphite as described previously (Clark et al, 1994). For methylation-specific PCR (MS-PCR) analysis of the DBCCR1 promoter (GenBank accession no. AF027734), the primers for the unmethylated reaction were 5′-TTTATGGTTGTAAATTGATTTGGTGTGT-3′ and 5′-CAACTCACATTCCAAACACAACACA-3′, which amplify a 269-bp product (positions 15–283), and the primers for the methylated reaction were 5′-TTGTAAATTGATTTGGCGCGC-3′ and 5′-TTCCGAACACGACGCGAAA-3′, which amplify a 253-bp product (positions 22–274). PCR was carried out using the HotStarTaq Kit (Qiagen); the annealing temperatures for the unmethylated and methylated reactions were 60 and 62°C, respectively. Primer sequences and reaction conditions for MS-PCR analysis of the ABO gene promoter were as described (Kominato et al, 1999; Gao et al, 2004). The PCR products were resolved on 2% agarose gels. DNA treated with SssI methyltransferase (New England Biolabs) served as the methylated control.
For methylation-specific melting-curve analysis (MS-MCA) of DBCCR1, the primers were 5′-GGGAGGTAGAGGGAGTAGTGAT-3′ and 5′-AAAATACCTAACTCCTAACAACCTAAC-3′, which amplify a 117-bp product (positions 127–243). PCR and subsequent MCA were carried out as previously described (Worm et al, 2001) using the LightCycler (Roche) and the FastStart DNA Master SYBR Green I Kit (Roche). Reactions were started by initial denaturation at 95°C for 10 min, followed by cycling at 95°C for 10 s, a transition from 72 to 66°C at 0.5°C cycle−1 for 10 s and 72°C for 20 s. Melting-curve analysis was performed immediately after amplification by measuring the fluorescence of SYBR Green I during a linear temperature transition from 70 to 95°C at 0.05°C s−1. Fluorescence data were converted into melting peaks by the LightCycler software (Ver.3.39) by plotting the negative derivative of fluorescence over temperature vs temperature (−dF/dT vs T).
Statistical analysis
Correlation analyses were performed using Fisher's exact probability test.
Results
LOH analysis of chromosome 9q33
LOH analysis of the 9q33 region using three microsatellite markers showed allelic loss in 10 of 31 (32%) informative cases of oral squamous cell carcinoma (Table 1; see Figure 1 for examples). Among these, four showed LOH at D9S1872, six at D9S195, and seven at 9-11407. Notably, three cases showed LOH at 9-11407 located ∼300 kb upstream of DBCCR1, but retention of D9S195 located in intron 1 of DBCCR1. In one case, in which DNA was isolated from both well- and poor-differentiated tumour cells from the same tumour, LOH at D9S195 was found in both populations, but only the poor-differentiated tumour cells showed LOH at 9-11407 and D9S1872 (Figure 1). LOH at D9S1872 was also found in one of four leukoplakias with dysplasia. No LOH was found in epithelial tissues adjacent to the tumours.
Methylation analysis
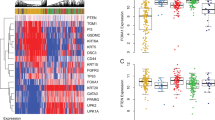
Hypermethylation of the DBCCR1 gene promoter was present in 15 out of 34 (44%) oral squamous cell carcinomas, as determined by MS-PCR analysis (Table 1; see Figure 2 for examples). In three out of seven cases, DBCCR1 hypermethylation was also found in tumour-adjacent tissues, including two hyperplastic and one histologically normal epithelia. To further characterise DBCCR1 methylation patterns in oral carcinomas and to exclude possible false-positive MS-PCR results, all samples showing a positive signal for methylated DBCCR1 alleles using MS-PCR were also examined using MS-MCA (Figure 2). Aberrant methylation was confirmed in all cases. However, in one case (#31572), well- and poor-differentiated tumour cells isolated from the same lesion showed different methylation patterns (Figure 2). Hypermethylation of the DBCCR1 gene was also found in two of four leukoplakias with dysplasia, none of which showed LOH at 9q33 (Table 1).
Methylation analysis of the DBCCR1 gene promoter in oral squamous cell carcinomas. Left, MS-PCR. Genomic DNA was treated with sodium bisulphfite and PCR-amplified with primer pairs specific for methylated (M) and unmethylated (U) alleles. Right, MS-MCA. Bisulphfite-treated DNA was amplified in the presence of SYBR Green I using primers that do not discriminate between methylated and unmethylated DBCCR1 alleles. The melting characteristics of the PCR products were determined directly in the PCR tube by continuous fluorescence monitoring during a temperature transition. SssI-methylated DNA and genomic DNA from normal peripheral blood lymphocytes (PBL) provided positive controls for methylated and unmethylated DBCCR1 alleles, respectively. Tu, tumour; Ep, epithelium; Cn, connective tissue; T1, well-differentiated tumour cells adjacent to normal epithelium; T2, poor-differentiated tumour cells far away from normal epithelium.
Concomitant LOH at 9q33 and hypermethylation of the DBCCR1 gene were found in seven carcinomas (P=0.057); however, this correlation was only significant for microsatellite marker 9-11407, which is located ∼300 kb upstream of exon 1 of the DBCCR1 gene (Table 2). Hypermethylation of ABO was found in 11 out of 34 (32%) tumour samples and in three adjacent epithelia (Table 1) (Gao et al, 2004), but there was no correlation between the DBCCR1 and ABO hypermethylation events (P = 0.11; Tables 1 and 2).
Discussion
Substantial evidence suggests that aberrant hypermethylation of promoter CpG islands may constitute an alternative mechanism to intragenic mutations and deletions for inactivation of tumour suppressor genes (Worm and Guldberg, 2002; Nephew and Huang, 2003). Hypermethylation of the DBCCR1 gene as well as LOH and homozygous deletions at the DBCCR1 locus have been shown to be frequent events in bladder cancer (Fujiwara et al, 2001; Habuchi et al, 1998, 2001; Nishiyama et al, 1999). Previous studies of head and neck carcinomas have demonstrated LOH involving the 9q32-33 region, which covers the DBCCR1 gene (Ah-See et al, 1994). In the present study, LOH at 9q33 was found in 32% of oral squamous cell carcinomas, suggesting that this region contains a tumour suppressor gene involved in oral carcinogenesis. Notably, LOH frequently involved microsatellite marker D9S195, which is located in intron 1 of DBCCR1 and was originally used to identify this gene as a candidate tumour suppressor (Habuchi et al, 1997). Methylation analysis of the DBCCR1 promoter region using two different techniques showed aberrant hypermethylation in 44% of the tumours. These data add DBCCR1 to the list of tumour suppressor genes known to be targeted by promoter hypermethylation in oral carcinomas, including p16, p15, E-cadherin, MGMT and ABO (Akanuma et al, 1999; Kim et al, 2000; Yakushiji et al, 2001; Chang et al, 2002; Hasegawa et al, 2002; Viswanathan et al, 2003; Gao et al, 2004). No correlation was found between hypermethylation of DBCCR1 at 9q33 and ABO at 9q34, suggesting that these genes are epigenetically targeted in oral carcinogenesis by independent and possibly specific events.
Genetic and epigenetic alterations of the DBCCR1 gene were not restricted to oral carcinomas. LOH at 9q33 was also demonstrated in one of four patients with severe epithelial dysplasia, and DBCCR1 hypermethylation was present in another two of these four cases. Aberrant hypermethylation levels were found even in tumour-adjacent epithelia with no histopathological evidence of malignancy, suggesting that it may represent an early event in oral malignant development. In bladder cancer, field cancerisation has been attributed to age-related methylation of DBCCR1 in normal epithelium (Habuchi et al, 2001). The presence of DBCCR1 hypermethylation in oral tumour-adjacent epithelium is of great interest and should be further investigated in order to elucidate whether local recurrence or field cancerisation in oral cancer patients can be explained, at least in some cases, by the existence of a DBCCR1-hypermethylated field in histologically normal epithelium.
In the present work, we were not able to detect any divergence between the two groups of patients, which were of different ethic origin and exposed to different environmental factors (betel/tobacco and alcohol/tobacco). However, the material is too limited to make any firm conclusions. In a new prospective study, we are investigating whether the methylation and LOH status have a clinical significance.
There is still little information about the possible function of the DBCCR1 gene in carcinogenesis. Unresolved issues include the apparent lack of DBCCR1 expression in most normal tissues and the unclear correlation between hypermethylation and transcriptional silencing of this gene (Habuchi et al, 1998), questioning the role of DBCCR1 as a tumour suppressor in the homeostasis of normal cells. Previous cell cycle studies suggested that DBCCR1 has growth-suppressing and antiproliferative activities mediated via modulation of the G1 checkpoint. Overexpression of DBCCR1 caused a slower G1 transition rather than G1 arrest and did not affect apoptosis (Nishiyama et al, 2001). Although these functional studies and the high rate of DBCCR1 hypermethylation in oral squamous cell carcinomas support the candidacy of DBCCR1 as a tumour suppressor at 9q33, additional studies are required to unravel its possible role in oral malignant development.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Ah-See KW, Cooke TG, Pickford IR, Soutar D, Balmain A (1994) An allelotype of squamous carcinoma of the head and neck using microsatellite markers. Cancer Res 54: 1617–1621
Akanuma D, Uzawa N, Yoshida MA, Negishi A, Amagasa T, Ikeuchi T (1999) Inactivation patterns of the p16 (INK4a) gene in oral squamous cell carcinoma cell lines. Oral Oncol 35: 476–483
Braakhuis BJ, Tabor MP, Kummer JA, Leemans CR, Brakenhoff RH (2003) A genetic explanation of Slaughter's concept of field cancerization: evidence and clinical implications. Cancer Res 63: 1727–1730
Califano J, van der Riet P, Westra W, Nawroz H, Clayman G, Piantadosi S, Corio R, Lee D, Greenberg B, Koch W, Sidransky D (1996) Genetic progression model for head and neck cancer: implications for field cancerization. Cancer Res 56: 2488–2492
Chang HW, Chow V, Lam KY, Wei WI, Yuen A (2002) Loss of E-cadherin expression resulting from promoter hypermethylation in oral tongue carcinoma and its prognostic significance. Cancer 94: 386–392
Clark SJ, Harrison J, Paul CL, Frommer M (1994) High sensitivity mapping of methylated cytosines. Nucleic Acids Res 22: 2990–2997
Fujiwara H, Emi M, Nagai H, Ohgaki K, Imoto I, Akimoto M, Ogawa O, Habuchi T (2001) Definition of a 1-Mb homozygous deletion at 9q32–q33 in a human bladder-cancer cell line. J Hum Genet 46: 372–377
Gao S, Worm J, Guldberg P, Eiberg H, Krogdahl A, Liu CJ, Reibel J, Dabelsteen E (2004) Genetic and epigenetic alterations of the blood group ABO gene in oral squamous cell carcinoma. Int J Cancer 109: 230–237
Habuchi T, Luscombe M, Elder PA, Knowles MA (1998) Structure and methylation-based silencing of a gene (DBCCR1) within a candidate bladder cancer tumor suppressor region at 9q32–q33. Genomics 48: 277–288
Habuchi T, Takahashi T, Kakinuma H, Wang L, Tsuchiya N, Satoh S, AkaoT, Sato K, Ogawa O, Knowles MA, Kato T (2001) Hypermethylation at 9q32-33 tumour suppressor region is age-related in normal urothelium and an early and frequent alteration in bladder cancer. Oncogene 20: 531–537
Habuchi T, Yoshida O, Knowles MA (1997) A novel candidate tumour suppressor locus at 9q32-33 in bladder cancer: localization of the candidate region within a single 840 kb YAC. Hum Mol Genet 6: 913–919
Hasegawa M, Nelson HH, Peters E, Ringstrom E, Posner M, Kelsey KT (2002) Patterns of gene promoter methylation in squamous cell cancer of the head and neck. Oncogene 21: 4231–4236
Kim HS, Chung WB, Hong SH, Kim JA, Na SY, Jang HJ, Sohn YK, Kim JW (2000) Inactivation of p16INK4a in primary tumors and cell lines of head and neck squamous cell carcinoma. Mol Cells 10: 557–565
Kominato Y, Hata Y, Takizawa H, Tsuchiya T, Tsukada J, Yamamoto F (1999) Expression of human histo-blood group ABO genes is dependent upon DNA methylation of the promoter region. J Biol Chem 274: 37240–37250
Landis SH, Murray T, Bolden S, Wingo PA (1999) Cancer statistics, 1999. CA Cancer J Clin 49: 8–31 1
Nephew KP, Huang TH (2003) Epigenetic gene silencing in cancer initiation and progression. Cancer Lett 190: 125–133
Nishiyama H, Gill JH, Pitt E, Kennedy W, Knowles MA (2001) Negative regulation of G(1)/S transition by the candidate bladder tumour suppressor gene DBCCR1. Oncogene 20: 2956–2964
Nishiyama H, Takahashi T, Kakehi Y, Habuchi T, Knowles MA (1999) Homozygous deletion at the 9q32–33 candidate tumor suppressor locus in primary human bladder cancer. Genes Chromosomes Cancer 26: 171–175
Ogi K, Toyota M, Ohe-Toyota M, Tanaka N, Noguchi M, Sonoda T, Kohama G, Tokino T (2002) Aberrant methylation of multiple genes and clinicopathological features in oral squamous cell carcinoma. Clin Cancer Res 8: 3164–3171
Partridge M, Emilion G, Pateromichelakis S, Phillips E, Langdon J (1999) Location of candidate tumour suppressor gene loci at chromosomes 3p, 8p and 9p for oral squamous cell carcinomas. Int J Cancer 83: 318–325
Silverman Jr S (2001) Demographics and occurrence of oral and pharyngeal cancers, the outcomes, the trends, the challenge. J Am Dent Assoc 132 (Suppl): 7S–11S
Viswanathan M, Tsuchida N, Shanmugam G (2003) Promoter hypermethylation profile of tumor-associated genes p16, p15, hMLH1, MGMT and E-cadherin in oral squamous cell carcinoma. Int J Cancer 105: 41–46
Warnakulasuriya S (2000) Lack of molecular markers to predict malignant potential of oral precancer. J Pathol 190: 407–409
Warnakulasuriya S (2001) Histological grading of oral epithelial dysplasia: revisited. J Pathol 194: 294–297
Williams HK (2000) Molecular pathogenesis of oral squamous carcinoma. Mol Pathol 53: 165–172
Worm J, Aggerholm A, Guldberg P (2001) In-tube DNA methylation profiling by fluorescence melting curve analysis. Clin Chem 47: 1183–1189
Worm J, Guldberg P (2002) DNA methylation: an epigenetic pathway to cancer and a promising target for anticancer therapy. J Oral Pathol Med 31: 443–449
Yakushiji T, Noma H, Shibahara T, Arai K, Yamamoto N, Tanaka C, Uzawa K, Tanzawa H (2001) Analysis of a role for p16/CDKN2 expression and methylation patterns in human oral squamous cell carcinoma. Bull Tokyo Dent Coll 42: 159–168
Acknowledgements
We would like to thank Ms Hanne Lykke Hansen, Ms Vibeke Ahrenkiel, Ms Annemette Mikkelsen, Ms Lillian Rasmussen and Ms Wei Wang for their expert technical assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Gao, S., Worm, J., Guldberg, P. et al. Loss of heterozygosity at 9q33 and hypermethylation of the DBCCR1 gene in oral squamous cell carcinoma. Br J Cancer 91, 760–764 (2004). https://doi.org/10.1038/sj.bjc.6601980
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6601980
Keywords
This article is cited by
-
Brinp1 −/− mice exhibit autism-like behaviour, altered memory, hyperactivity and increased parvalbumin-positive cortical interneuron density
Molecular Autism (2016)
-
Role of DNA methylation in head and neck cancer
Clinical Epigenetics (2011)
-
Identification of 5 novel genes methylated in breast and other epithelial cancers
Molecular Cancer (2010)
-
Frequent hypermethylation of DBC1 in malignant lymphoproliferative neoplasms
Modern Pathology (2008)