Abstract
Small-cell lung cancer (SCLC) accounts for approximately 15% of all cases of lung cancer and is a particularly aggressive form of lung cancer characterised by a poor prognosis, rapid tumour growth, and early metastasis. Roughly, two-thirds of patients with SCLC present with extensive disease (ED) and one-third with limited disease (LD). Combination chemotherapy is the most effective treatment modality for SCLC, and several new agents, including carboplatin, ifosfamide, taxans, and topotecan, have been demonstrated to be active; however, there are no data on the survival benefit of these drugs. A CPT-11+ cisplatin regimen has shown improvement in overall survival over the global gold standard regimen, etoposide + cisplatin (Japanese Clinical Oncology Group: JCOG 9511), and three confirmatory randomised controlled trials are in progress to determine the reproducibility of the JCOG 9511 study. JCOG is evaluating the role of CPT-11 and a new triplet regimen containing CPT-11 in limited-stage SCLC. Strategies and the current protocols of the JCOG are presented and discussed. In the future, it will be essential to evaluate molecular target-based drugs for LD and ED SCLC with new standard combination chemotherapy regimens that include CPT-11.
Similar content being viewed by others
Main
Lung cancer is one of the most common cancers not only in Western countries but also in Japan as well. Small-cell lung cancer (SCLC) has a poor prognosis and accounts for approximately 15% of all lung cancer deaths. It is characterised by an aggressive clinical course, rapid tumour growth, and metastatic spread, and despite being a chemo- and radiosensitive tumour, majority of SCLC patients die because of recurrence after the response to initial treatment. Roughly, one-third present with limited-stage disease (LD), and the remainder with extensive-stage disease (ED). Surgery and radiation therapy have been used as a single modality or in combined modality therapy but have resulted in few cures (Hanna and Einhorn 2002). The standard treatment strategy for LD-SCLC and ED-SCLC is chemoradiotherapy and chemotherapy, respectively (Evans et al, 1987; Fukuoka et al, 1991; Fukuda et al, 1996; Saijo 2002; Sandler 2002). A cisplatin (CDDP) + etoposide (VP-16) (PE) regimen is the most frequently used chemotherapeutic regimen worldwide, and various strategies, such as the introduction of new anticancer drugs, non-cross-resistant alternative chemotherapy (Evans et al, 1987; Fukuoka et al, 1991; Murray et al, 2001), weekly dose-intensive chemotherapy (Murray et al, 1991), high-dose chemotherapy with haematopoietic stem cell support (Elias et al, 1993), and the evaluation of timing, dose, or fractionation of radiation therapy have been tested in randomised controlled trials to improve the results of treatment of SCLC (Sandler, 2001). Several new anticancer drugs, including ifosfamide and taxans, have been shown to be active against SCLC, but, have not resulted in improvement of overall survival. The most active one of these drugs to date has been the topoisomerase I inhibitor irinotecan (CPT-11) (Saijo et al, 1994; Le Chevalier et al, 1997; Devore et al, 1998; Kelly, 2001; Shihabi and Belani, 2001). This review focuses on the contribution of CPT-11 to improvement of the results of treatment of SCLC and discusses the future development of CPT-11 in the treatment of SCLC.
Single-agent activity of CPT-11 against SCLC
In the phase I trial of CPT-11, the recommended dose of CPT-11 was determined to be 100–125 mg m−2 once a week and 150 mg m−2 every 2 weeks (Negoro et al, 1991a, 1991b).
A multi-institutional phase II study was conducted in previously treated and untreated SCLC patients, and nine out of 27 previously treated patients and four out of 8 previously untreated patients experienced an objective tumour response (Kanzawa et al, 1990; Negoro et al, 1991a, 1991b). Masuda used CPT-11 100 mg/m−2 as a 90-min infusion every week to treat 16 patients with refractory or relapsed SCLC, and seven out of 15 evaluable patients responded to CPT-11 (Masuda et al, 1992).
In addition to SCLC, CPT-11 has been demonstrated to be active as single-agent chemotherapy for non-small-cell-lung-cancer, colon cancer, breast cancer, uterine cancer, stomach cancer, ovarian cancer, etc.
Development of the CPT-11+CDDP regimen
It is essential to combine the maximum effective doses of active anticancer drugs in order to obtain a better therapeutic effect. We have demonstrated that combinations of cisplatin with topoisomerase I inhibitors have an exclusively synergistic effect (Kanzawa et al, 1990; Fukuda et al, 1996). DNA interstrand crosslinks are significantly increased by such combinations, and DNA repair after interstrand crosslinks formed by cisplatin is inhibited by topoisomerase inhibitors. On the other hand, the topoisomerase I inhibitory activities of CPT-11 and SN-38 are increased by CDDP. In nude mice transplanted with human SCLC, the CPT-11 and CDDP combination showed a synergistic effect (Tamura et al, 1997). Phase I studies of CPT-11 and CDDP combinations with or without the support of granulocyte-colony stimulating factor (G-CSF) were conducted in untreated patients with stage IV NSCLC. CPT-11 was given on days 1, 8, and 15, and CDDP on day 1, and the schedule was repeated every 4 weeks. The dose of CDDP was fixed at 60 or 80 mg m−2. Without the support of G-CSF, the recommended dose of CPT-11 for a phase II study in combination with 60 and 80 mg m−2 of CDDP was 80 and 60 mg m−2, respectively. The dose-limiting toxicities were granulocytopenia and diarrhoea (Masuda et al, 1993).
Phase II study of CPT-11 and CDDP
The West Japan Thoracic Oncology Group (WJTOG) conducted a phase II trial of CPT-11 and CDDP in SCLC. In all 75 untreated patients with SCLC were treated with 80 or 60 mg m−2 of CPT-11 on days 1, 8, and 15 and 60 mg m−2 of CDDP on day 1 every 28 days. Patients with LD-SCLC received thoracic irradiation after four cycles of chemotherapy whereas patients with ED received four or six cycles of chemotherapy. The dose of CPT-11 was reduced to 60 mg m−2 after four of 10 patients experienced severe haematological toxicity, diarrhoea, and hepatic toxicity, while one patient died of toxicity. Among the 35 ED patients, the objective response rate was 86% (30 patients), with 10 patients (29%) having a complete response (CR). The median survival time was 13 months. Among the 40 LD patients, 33 (83%) had a response and 12 (30%) had a CR, and the median survival time for this subset of patients was 14.3% months. The significant grade 3/4 toxicities were neutropenia (77%), anaemia (39%), nausea (35%), and diarrhoea (19%) (Kudoh et al, 1998). These results were very encouraging, especially for ED-SCLC.
Phase III study of CPT-11+CDDP vs VP-16+CDDP (JCOG 9511)
Based on the results of a study of the CPT-11+CDDP combination, JCOG conducted a phase III study comparing CPT-11+CDDP with VP-16+CDDP for untreated ED-SCLC.
The study arm consisted of CPT-11 60 mg m−2 on days 1, 8, and 15 and CDDP 60 mg m−2 on day 1, every four weeks, for four courses. The control arm consisted of VP-16 100 mg m−2 on days 1–3 and CDDP 80 mg m−2 on day 1, every 3 weeks, for four courses. The initial sample size was 230 patients, 115 cases per arm, in order to demonstrate a 30% increase in overall survival with the significant difference of α error P<0.05 and β error <0.8. However, enrollment into the study was stopped because of a huge difference (P=0.00025) in survival on an interim analysis.
In the final data, 154 patients were randomised, 77 into each arm, and the overall and CR rates were 84 and 3%, respectively, in the CPT-11+ CDDP arm and 68 and 9%, respectively, in the VP-16+CDDP arm, (P=0.02 for the difference in overall response rate). The median survival time was 12.8 and 9.4 months in the CPT-11+CDDP arm and VP-16+CDDP arm, respectively. The CPT-11 + CDDP arm was characterised by significantly better survival than the standard regimen, VP-16+ CDDP (P=0.002 unadjusted one-sided log-rank test). The rates (95% confidence limit) of overall survival in CPT-11+CDDP arm were 58.4 (47.7–69.4) % at 1 year and 19.5 (10.0–27.8)% at 2 years: in VP-16 plus CDDP arm the rates of overall survival at these time points, were 37.7 (26.8–48.5) % and 5.2 (1.0-12.0)%, respectively (Figure 1).
Grade 3/4 leukopenia occurred in 27% of patients on CPT-11 + CDDP and in 52% on VP-16 + CDDP (P=0.002). Grade 3/4 neutropenia developed in 65% of patients on CPT-11+CDDP and in 92% on VP-16+CDDP (P<0.001). Grade 3/4 diarrhoea, on the other hand, occurred in 16% of the patients in the CPT-11+CDDP arm, but in none of the patients in the VP-16+ CDDP arm (P<0.001). Treatment with four cycles of CPT-11+ CDDP every 4 weeks yielded a highly significant improvement in survival in ED-SCLC over standard VP-16+ CDDP, with less myelosuppression. There were no statistically significant differences between patient characteristics, and there were slightly more patients with more favourable pretreatment characteristics, such as female gender, PS 0 or 1, fewer patients with brain metastasis, in the CPT-11+ CDDP arm. In view of the small sample size in the study, even small differences in patient characteristics may have resulted in outcome differences between the two arms. Another problem was compliance with the regimen. Only 29% of patients received the full dose of chemotherapy without skips or delays in CPT-11+ CDDP arm. Based on the results of JCOG 9511, CPT-11+ CDDP is considered the reference chemotherapy arm for ED-SCLC in future JCOG trials (Noda et al, 2002).
The data of JCOG 9511 are clearly interesting, however, only 154 patients have been randomised. It is essential to evaluate the reproducibility of the effect of CPT-11. Three randomised controlled trials, PHA GMA 262, SWOG SO124, and Aventis GMA 3001, are in progress; to confirm the data obtained in JCOG 9511 (Table 1).
Chemotherapy with cisplatin+CPT-11+VP-16
The VP-16+CDDP regimen is still considered the standard regimen in North America, and CPT-11+CDDP showed a survival benefit in JCOG9511. The combination chemotherapy with CPT-11+ VP-16 also shows promising results (Karato et al, 1993; Masuda et al, 1998). It is quite reasonable to investigate the three-drug combination CPT-11+VP-16+CDDP to increase efficacy without increasing toxicity (Table 2). The JCOG has conducted two phase I/II studies of CDDP + VP-16+CPT-11 combination chemotherapy using two different schedules: weekly (JCOG 9507) and four-weekly (JCOG 9512) (Ohe and Saijo, 2002). Based on the doses determined in the two phase I studies, a randomized phase II study (JCOG 9902-DI) Table 3 was conducted comparing weekly and every-four-week schedules of this three-drug combination to select the appropriate arm for the future phase III trial (JCOG 9902-DI) (Figure 2).
Weekly chemotherapy consisted of CDDP 25 mg m−2 on day 1 of weeks 1–9, CPT-11 90 mg m−2 on day 1 of weeks 1, 3, 5, 7, and 9, and VP-16 60 mg m−2 on days 1–3 of weeks 2, 4, 6, and 8, G-CSF support. Chemotherapy for the every-4-week schedule consists of CDDP 60 mg/m2 on day 1, CPT-11 60 mg/m2 on days, 1, 8, and 15, and VP-16 50 mg m−2 on days 1–3, with G-CSF support. The doses of these agents were decided in phase I studies, but the schedule for the weekly regimen has been modified. The original JCOG 9507 schedule consisted of CDDP 25 mg m−2 on day 1 of weeks 1–9, escalating doses of CPT-11 on day 1 of weeks 2, 4, 6, and 8, and VP-16 60 mg m−2 on days 1–3 of weeks 1, 3, 5, 7, and 9, with G-CSF support. Since we concluded that irinotecan is more active against SCLC than VP-16 based on the results of JCOG 9511, CPT-11 and CDDP is given in week 1 instead of VP-16 and CDDP in JCOG 9902-DI.
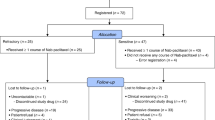
A total of 60 patients with chemotherapy-naïve ED-SCLC have been enrolled in the study, and the eligibility criteria included age ⩽70 years, PS 0-2, and no prior therapy. Arm A consisted of P (25 mg m−2 day 1) weekly for 9 weeks, CPT-11 (90 day 1) in weeks 1, 3, 5, 7 and 9, and VP-16 (60 days 1–3) in weeks 2, 4, 6, and 8. Arm B consisted of cisplatin (60 mg m−2 day 1), I (60 days 1, 8, 15), and VP-16 (50 days 1–3) every 4 weeks for four cycles. G-CSF support was used in both arms. Between August 1999 and October 2000, 60 patients were randomised to arm A (n=30) and arm B (n=30).
Full cycles were delivered in 73 and 70% of the patients in arms A and B, respectively. The incidences of grade 3–4 neutropenia, anaemia, thrombocytopenia, infection, and diarrhoea were 57, 43, 27, 7, and 7%, respectively, in arm A, and 87, 47, 10, 13, and 10%, respectively in arm B. Treatment-related death was observed in one patient in arm A. The CR rate and partial response (PR) rate were 7 and 77%, respectively, in arm A, and 17 and 60% in arm B. MST and the 1-year survival rate were 8.9 months and 40%, respectively, in arm A, and 12.8 months and 56% in arm B. In conclusion, arm B was appropriate as an investigational arm in further phase III studies (Sekine et al, 2003). JCOG is conducting a randomised controlled trial comparing a CPT-11+CDDP regimen consisting of CPT-11 60 mg m−2 on days 1 and 8, and CDDP 60 mg m−2 on day 1 with a CPT-11 + VP-16 + CDDP regimen consisting of CPT-11 60 mg m−2 on days 1 and 8, CDDP 60 mg m−2 on day 1, and VP-16 50 mg m−2 on days 1–3. Both the regimens will be given every 3 weeks.
Treatment of recurrent SCLC with a CPT-11+CDDP+VP-16 regimen
There is no standard treatment for relapsed SCLC (Schulthesis et al, 2001). Since CPT-11 and VP-16 have been studied in several phase II trials as active agents for relapsed SCLC, we conducted a phase II study to evaluate the efficacy and toxicity of CPT-11 combined with weekly CDDP and VP-16 (PE) in patients (pts) with SCLC who had relapsed at least 8 weeks after completion of first-line therapy. Patients had to have measurable or assessable disease, be age 75 years old or under, and have performance status of 0 to 2 (ECOG), and adequate organ function. The PE/CPT regimen consisted of CDDP 25 mg m−2 on day 1 at 1-week intervals for 9 weeks (at least 6 weeks), VP-16 60 mg m−2 on days 1–3 in weeks 1, 3, 5, 7, and 9 (at least in weeks 1, 3, 5), and CPT-11 90 mg m−2 in weeks 2, 4, 6, and 8 (at least in weeks 2, 4, 6). After day 1 in week 2, G-CSF was administered on days when no cytotoxic drugs were given.
Between October 1998 and March 2001, 40 pts were enrolled in this study. Patient characteristics were median age 67 years (range 41–74), 29 males and 11 females, 5 LD and 35 ED. Prior chemotherapy included PE in 11 patients, carboplatin and VP-16 in 11, PE/CODE in six, cisplatin and irinotecan in six, PE/CPT in two, and others in four patients. Eight patients received thoracic radiotherapy. In all, 32 patients (80%) completed six or more weeks of chemotherapy. There were five CRs and 26 PRs, and the overall response rate was 78% (95% CI 64.6–90.4%). The median survival time was 11.4 months. Grade 3/4 neutropenia and thrombocytopenia were observed in 73 and 33%, respectively. Grade 3 nausea/vomiting was observed in 8%, and grade 3/4 diarrohea in 8%. In conclusion, the PE/CPT regimen was active against relapsed SCLC and well tolerated (Goto et al, 2002).
CPT-11-containing regimens for LD-SCLC
CPT-11-containing regimens are considered to be one of the most promising strategies for improving the survival of LD-SCLC patients. Early concurrent thoracic radiation therapy with combination chemotherapy consisting of VP-16/CDDP is a standard treatment for LD-SCLC patients (Perry et al 1987; Pignon et al, 1992; Murray et al, 1993; Jeremic et al, 1997; Work et al, 1997). Twice-daily thoracic radiation therapy and prophylactic cranial irradiation after a CR have recently been added to the standard treatment (Trussi et al, 1999; Takada et al, 2002). Thus, concurrent twice-daily thoracic radiation therapy with combination chemotherapy consisting of CPT-11/CDDP may be the most powerful treatment for LD-SCLC patients, if the full dose of CPT-11 can be given with acceptable toxicity. Previously, the JCOG conducted a dose-finding study for CPT-11/CDDP plus concurrent radiation therapy in unresectable stage III NSCLC (JCOG 9405). The CPT-11 dose intensity in that study was low because of the need to skip CPT-11 administration of days 8 and/or 15 as a result of leukopenia or diarrhoea, and the radiation therapy completion rate was low as well. Based on the results of JCOG 9405, chemotherapy with CPT-11/CDDP plus concurrent radiation therapy was deemed unacceptable (Yokoyama et al, 1998).
The JCOG also conducted a phase II study of single-agent CPT-11 (60 mg m−2) in combination with radiation therapy in NSCLC (JCOG 9504). When CPT-11 is used as a single agent with concurrent radiation therapy, the dose of CPT-11 must be reduced from 100 to 60 mg m−2 in a weekly schedule. However, this dose reduction may reduce the efficacy of CPT-11 in the treatment of LD-SCLC patients. Full-dose chemotherapy consisting of VP-16/CDDP can also be used in combination with concurrent radiation therapy (Table 3).
Japanese Clinical Oncology Group, therefore, conducted a pilot study of concurrent twice-daily thoracic radiation therapy plus VP-16/CDDP followed by three cycles of chemotherapy with standard doses of CPT-11/CDDP (JCOG-9903-DI). To be eligible, patients had to have previously untreated LD-SCLC, be <75 years of age, and have an ECOG performance status (PS) of 0-2 and adequate organ function. Treatment consisted of 80 mg m−2 of CDDP on day 1 and 100 mg m−2 of VP-16 on day 1–3. Accelerated twice daily thoracic radiation therapy (TRT) started on day 2 and involved administration of 1.5 Gy in 30 fractions over a period of 3 weeks. After completion of PE/TRT, the patients received 3 cycles of CPT-11+CDDP started on day 29. IP consisted of 60 mg m−2 of CPT-11 on days 1, 8, and 15 and 60 mg m−2 of CDDP on day 1 every 4 weeks.
Between October 1999 and July 2000, 31 patients were enrolled in the study. Patient characteristics were: male 27, female 4, median age 62 years, range 43–74 years, PS 0/1: 8/23. Of the 30 patients who received the protocol treatment, 11 pts had a CR, 18 had a PR, and one progressive disease, for a response rate of 97%. Totally 25 patients received CPT-11+CDDP. Grade 3/4 toxicities during CPT-11+CDDP phase were: WBC (48/12%), plt (4/0%), Hb (44/—), diarrohea (4/4%). No treatment-related deaths were observed. The 1-year survival rate was 79.3% among patients who received the protocol treatment, and 87.5% among pts who received the CPT-11+CDDP regimen. The median survival time has not been obtained (Table 4) (Mori et al, 2002). In conclusion, PE plus concurrent twice daily TRT followed by three cycles of CPT-11+CDDP is a safe and active regimen with an encouraging 1-year survival rate. JCOG is conducting a phase III study comparing it with the standard PE concurrent accerelated hyperfractionated TRT regimen (Figure 3).
Conclusions
Although dramatic improvements in survival in response to combination chemotherapy were observed in the 1970s and 1980s, the results of treating SCLC had reached a plateau. Novel drugs and approaches are essential to further improve the outcome of treatment. Significant activity of CPT-11 in the treatment of patients with SCLC provides the first evidence in 20 years that the survival of SCLC patients can be prolonged, although we must await the results of confirmatory studies. Current and future trials of CPT-11 will be aimed at evaluating three-drug regimens containing CDDP and CPT-11 in multimodality therapies and targeting limited-stage disease. In addition, CPT-11 may have the potential to be a part of second-line treatment for SCLC. In the future, combining a CPT-11 containing regimen with target-based therapy will also be a major focus of new directions in SCLC therapy in order to overcome resistance to CPT-11. In Japan, amrubicin has been demonstrated to be extremely active against SCLC and the optimal dose for the combination of amrubicin and CDDP has been decided. The role of amrubicin for the treatment of SCLC should also be investigated.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Devore R, Blanke C, Denham C, Hainsworth JD, Gralla RJ, Koletsky AJ, Savaraj N, Vogal CL, Sarma GP, Brooks DJ, Petit RG, Elfing GL, Schaaf LJ, Hanover CK, Miller LL (1998) Phase II study of CPT-11 in patients with previously treated small cell lung cancer. Proc Amer Soc Clin Oncol 17: 451a
Elias AD, Ayash L, Frei E, Skarim AT, Hunt M, Wheeler C, Schwartz G, Mazanet R, Tepler I, Eder JP (1993) Intensive combined modality therapy for limited-disease small cell lung cancer. J Natl Cancer Inst 85: 559–566
Evans WK, Feld R, Murray N, William A, Coy P, Osoba D, Shepherd FA, Clark DA, Levitt M, McDonald A, Wilson K, Shelley W, Pater J (1987) Superiority of alterrating cross resistant chemotherapy in extensive small cell lung cancer. A multicenter randomized clinical trial by National Cancer Institute of Canada. Ann Intern Med 107: 451–458
Fukuda M, Nishio K, Kanzawa F, Ogasawara H, Ishida T, Arioka H, Bojanwski M, Oka M, Saijo N (1996) Synergism between cisplatin and topoisomerase I inhibitors, NB506 and SN38, in human small cell lung cancer cells. Cancer Res 56: 789–793
Fukuoka M, Furuse K, Saijo N, Nishiwaki Y, Ikegami H, Tamura T, Shimoyama M, Suemasu K (1991) Randomized trial of cyclophosplamide, doxorubicin, and vincristine versus cisplatin and etoposide versus alternation of these regimens in small cell lung cancer. J Natl Cancer Inst 83: 855–861
Goto K, Sekine I, Nishiwaki Y, Sugiura T, Kawase I, Saijo N (2002) Phase II study of weekly cisplatin etoposide and irinotecan (PF/CPT) for relapsed small cell lung cancer. Proc Amer Soc Clin Oncol 21: 316
Hanna NH, Einhorn LH (2002) Small cell lung cancer: State of the art. Clin Lung Cancer 4: 87–94
Jeremic B, Shibamoto Y, Acimovi CL, Milisavljevic S (1997) Initial versus delayed accelerated hyperfractionated radiation therapy and concurrent chemotherapy in limited small cell lung cancer. J Clin Oncol 15: 893–900
Kanzawa F, Sugimoto Y, Minato K, Kasahara K, Bungo M, Nakagawa K, Fujiwara Y, Liu LF, Saijo N (1990) Establishment of a camptothecin analogue (CPT-11) resistant cell line of human non-small cell lung cancer. Cancer Res 50: 5919–5924
Karato A, Sasaki Y, Shinkai T, Eguchi K, Tamura T, Ohe Y, Oshita F, Nishio M, Kunikane H, Arioka H, Ohmatsu H, Nakashima H, Shiraishi J, Saijo N (1993) Phase I study of CPT-11 and etoposide in patients with refractory solid tumors. J Clin Oncol 11: 2030–2035
Kelly K (2001) Irinotecan in small cell lung cancer: current data. Clin Lung Cancer 2: S4–S8
Kudoh S, Fujiwara Y, Takada Y, Yamamoto H, Kinoshita A, Ariyoshi Y, Furuse K, Fukuoka M for the West Japan Lung Cancer Group (1998) Phase II study of irinotecan combined with cisplatin in patients with previously untreated small cell lung cancer. J Clin Oncol 16: 1068–1074
Le Chevalier T, Ibrahim N, Chomy P, Riviere A, Mannier A, Magherini E, Pujol JL (1997) A phase II study of irinotecan in patients with small cell lung cancer progressing after first line treatment. Proc Amer Soc Clin Oncol 16: 450a
Masuda N, Fukuoka M, Kusunoki Y, Matsui K, Takifuji N, Kudoh S, Negoro S, Nishioka M, Nakagawa K, Saijo N (1992) CPT-11: a new derivative of comptothecin for the treatment of refractory or relapsed small cell lung cancer. J Clin Oncol 10: 1225–1229
Masuda N, Fukuoka M, Kudoh S, Kusunoki Y, Matusi K, Takifuji N, Nakagawa K, Tomonari M, Nitta T, hirashima T, Negoro S, Takada M (1993) Phase I and pharmacologic study of irinotecan in combination with cisplatin for advanced lung cancer. Br J Cancer 68: 777–782
Masuda N, Matsui K, Negoro S, Takifuji N, Takeda K, Yano T, Kobayashi M, Hirashima T, Kusunoki Y, Ushijima S, Kawase I, Tada T, Sawaguchi H, Fukuoka M (1998) Combination of irinotecan and etoposide for treatment of refractory or relapsed small cell lung cancer. J Clin Oncol 16: 3329–3334
Mori K, Kuboka K, Nishiwaki Y, Sugiura T, Noda K, Kawahara M, Negoro S, Watanabe K, Yokoyama A, Nakamura S, Tamura T, Saijo N (2002) Cisplatin and etoposide plus concurrent accelerated hyperfractionated thoracic radiotherapy followed by three cycles of irinotecan and cisplatin. Proc Amer Soc Clin Oncol 21: 1173
Murray N, Shah A, Osoba D, Page R, Harssi H, Graftion C, Gostard K, Fairey R, Voss N (1991) Intensive weekly chemotherapy for the treatment of extensive small cell lung cancer. J Clin Oncol 9: 1632–1638
Murray N, Zee B, Coy P, Hodson I, Arnoid A, Payne D, Kostashuk E, Evans W, Dixan W, Sadura A, Feld R, Levitt M, Wierzbicki R, Ayoub J, Maroun J, Wilson K (1993) Importance of timing for thoracic irradiation in the combined modality treatment of limited stage small cell lung cancer: The National Cancer Institute of Canada Clinical Trials Group. J Clin Oncol 11: 336–344
Murray N, Livinggston RB, Shephard FA, James K, Zee B, Langleben A, Kraut M, Bearden J, Goodwin JW, Grafton C, Turrisi A, Walde D, Craft H, Osoba D, Ottoway J, Gandara D (2001) Randomized study of CODE versus alternating CAV/EP for extensive-stage small cell lung cancer: an intergroup study of NCI-Canada CTG and SWOG. J Clin Oncol 17: 2300–2308
Negoro S, Fukuoka M, Masuda N, Takada M, Kusunoki Y, Matsui K, Takifuji N, Kudoh S, Niitani H, Taguchi T (1991a) Phase I study of weekly intravenous infusions of CPT-11, a new derivative of camptothecin, in the treatment of advanced non small cell lung cancer. J Natl Cancer Inst 83: 1164–1168
Negoro S, Fukuoka M, Niitani H, Suzuki A, Nakabayashi T, Kimura M, Motomiya M, Kurita Y, Hasegawa K, Kukiyama T, Nishiwaki Y, Ogawa M, Nakao I, Saijo N, Obo K, Furue H, Ariyoshi Y, Shimokata K, Furuse K, Nakajima S, Irie K, Kimura I, Ogura T, Fujii M, Hara N, Hara Y, Nakano S, Araki J, Miyata Y, Taguchi T (1991b) A phase II study of CPT-11, a camptothecin derivative, in patients with primary lung cancer. Jpn J Cancer Chemother 18: 1013–1019
Noda K, Nishiwaki Y, Kawahara M, Negoro S, Sugiura K, Yokoyama A, Fukuoka M, Mori K, Watanabe K, Tamura T, Yamamoto S, Saijo N for Japan Clinical Oncology Group (2002) Irinotecan plus cisplatin compared with etoposide plus cisplatin for extensive small cell lung cancer. Eng J Med 346: 85–91
Ohe Y, Saijo N (2002) Result of recent Japanese clinical trials in lung cancer. Clin Lung Cancer 4: 243–248
Perry MC, Eaton WL, Propert KJ, Ware JH, Eimmer B, Chahinian AP, Skarin A, Carey RW, Kreisman H, Faulkner C (1987) Chemotherapy with or without radiation therapy in limited small cell carcinoma of the lung. N Engl J Med 316: 912–918
Pignon JP, Aiagada R, Ihde DC, Johnson DH, Perry MC, Souhami RL, Brodin O, Joss RA, Kies MS, Lebeau B, Onoski T, Osterlind K, Tattersall MHN, Wagner H (1992) A meta—analysis of thoracic radiotherapy for small cell lung cancer. N Engl J Med 327: 1618–1624
Saijo N (1996) Clinical trials of irinotecan hydrochoride (CPT, campto injection, tepotecin injection) in Japan. In the camptothecins from discovery to the patients. Pantazis P, Giovanella BC, Rothenberg ML (eds). Ann NY Acad Sci 803: 292–305 (The New York Academy Sciences, New York)
Saijo N (2002) Preclinical and clinical trials of topoisomerase inhibitors, In ‘The Camptothecins Unfolding their Anticancer Potential’. Liehr JG, Giovanella BC, Verschraegen CF (eds). Ann NY Acad Sci 922: 92–99 (The New York Academy Sciences, New York)
Saijo N (2002) Irinotecan combined with radiation therapy for patients with stage III non-small cell lung cancer. Clin Lung Cancer 4: S21–S25
Sandler A (2001) Irinotecan: future directions in small cell lung cancer. Clin Lung Cancer 2: S9–S13
Saijo N, Nishio K, Kubota N, Kanzawa F, Shinkai T, Karato A, Sasaki Y, Eguchi K, Tamura T, Ohe Y, Oshita F, Nishio M (1994) 7-Ethyl-10-[4-(1-piperidino)-1-piperidino] carbonylony camptothecin: mechanisms of resistance and clinical trial. Cancer Chemoher Pharmacol 34: S112–S117
Sandler A (2002) Irinotecan in small cell lung cancer: Current data and the status of on going trials. Clin Lung Cancer 4: S30–S34
Schulthesis CP, Raheam MA, Perry MC (2001) Second line chemotherapy for small cell lung cancer: a review. Clin Lung Cancer 3: 118–124
Sekine I, Nishiwaki Y, Noda K, Kudoh S, Fukuoka M, Mori K, Negoro S, Yokoyama A, Matsui K, Osaki Y, Nakano T, Saijo N (2003) Randomized phase II study of cisplatin, irinotecan and etoposide combinations administered weekly or every four weeks for extensive small cell lung cancer: JCOG 9902-DI. Ann Oncol 14: 709
Shihabi S, Belani CP (2001) Role of topoisomerase I inhibitor in small cell lung cancer. Clin Lung Cancer 4: 275–281
Takada M, Fukuoka M, Kawahara M, Sugiura T, Yokoyama A, Yokota S, Nishiwaki Y, Watanabe K, Noda K, Tamura T, Fukuda H, Saijo N (2002) Phase III study of concurrent vs sequential thoracic radiotherapy in combination with cisplatin and etoposide for limited-stage small cell lung cancer: results of the Japan Clinical Oncology Group Study 9104. J Clin Oncol 20: 3054–3060
Tamura K, Takeda M, Kawase I, Tada T, Kudoh S, Okishio K, Fukuoka M, Yamaoka N, Fujiwara Y, Yamakido M (1997) Enhancement of tumor-radio response by irinotecan in human lung tumor xenografts. Jpn J Cancer Res 88: 218–223
Trussi AT, Kim K, Blum R, Sause WT, Livingston RB, Komaki R, Wagner H, Aisner S, Johnson DH (1999) Twice daily compared with once daily thoracic radiotherapy in limited small cell lung cancer treated concurrently with cisplatin and etoposide. N Engl J Med 340: 265–271
Work E, Nielsen O, Bentren S (1997) Randomized study of initial versus late chest irradiation combined with chemotherapy in limited stage small cell lung cancer. J Clin Oncol 15: 3030–3037
Yokoyama A, Kurita Y, Saijo N, Tamura T, Noda K, Shimokata K, Matsuda Y (1998) Dose finding study of irinotecan and cisplatin plus concurrent radiotherapy for unresectable stage III non small cell lung cancer. Br J Cancer 78: 257–262
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Saijo, N. Progress in treatment of small-cell lung cancer: role of CPT-11. Br J Cancer 89, 2178–2183 (2003). https://doi.org/10.1038/sj.bjc.6601456
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6601456
Keywords
This article is cited by
-
Emerging roles of Myc in stem cell biology and novel tumor therapies
Journal of Experimental & Clinical Cancer Research (2018)