Abstract
Periodate-treated, non-anticoagulant heparin-carrying polystyrene consists of about ten periodate-oxidized, alkaline-degraded low molecular weight-heparin chains linked to a polystyrene core and has a markedly lower anti-coagulant activity than heparin. In this study, we evaluated the effect of non-anticoagulant heparin-carrying polystyrene on tumour growth and metastasis. Non-anticoagulant heparin-carrying polystyrene has a higher activity to inhibit vascular endothelial growth factor-165-, fibroblast growth factor-2- or hepatocyte growth factor-induced human microvascular endothelial cell growth than heparin, ten periodate-oxidized-heparin and ten periodate-oxidized-low molecular weight-heparin, which is probably due to the heparin-clustering effect of non-anticoagulant heparin-carrying polystyrene. Non-anticoagulant heparin-carrying polystyrene inhibited human microvascular endothelial cell, B16 melanoma and Lewis lung cancer cell adhesion to Matrigel-coated plates. Non-anticoagulant heparin-carrying polystyrene also showed strong inhibitory activities in the tubular formation of endothelial cells on Matrigel and B16-melanoma and Lewis lung cancer cell invasion in a Matrigel-coated chamber assay. In vivo studies showed that growth of subcutaneous induced tumours and lung metastasis of B16-melanoma and Lewis lung cancer cells were more effectively inhibited by non-anticoagulant heparin-carrying polystyrene than ten periodate-oxidized-heparin and ten periodate-oxidized-low molecular weight-heparin. Furthermore, non-anticoagulant heparin-carrying polystyrene markedly reduced the number of CD34-positive vessels in subcutaneous Lewis lung cancer tumours, indicating a strong inhibition of angiogenesis. These results suggest that non-anticoagulant heparin-carrying polystyrene has an inhibitory activity on angiogenesis and tumour invasion and may be very useful in cancer therapy.
Similar content being viewed by others
Main
Heparin (Hep)/heparan sulphate (HS) are members of the glycosaminoglycans (GAGs) and are normally present as proteoglycans (PGs), in which a number of Hep/HS-chains are covalently attached to a core protein. While HS is widely distributed on cell surfaces and in extracellular matrices in most animal tissues, Hep is synthesised by mast cells in connective tissue and stored in cytoplasmic granules (Ishihara and Ono, 1998). Heparin is isolated on a commercial basis from animal tissue (pig or bovine intestinal mucosa, or bovine lung etc.) and has been extensively used as an anti-thrombotic drug for a long time (Ishihara and Ono, 1998). The biological role of Hep/HS is highly diverse. Aside from its well-known anti-coagulant action, the molecules are found to be associated with growth factors and cytokines in various biological processes, as well as being involved in cell adhesion, recognition, migration, and regulation of various enzymatic activities (Lindahl et al, 1994; Kjellen and Lindahl, 1991).
Several studies have reported both inhibitory and stimulatory effects of Hep on tumour growth and metastasis (Zacharski and Ornstein, 1998; Engelberg, 1999; Smorenburg and Van Noorden, 2001). Besides the anticoagulant function, Hep binds to various growth factors, cytokines, and extracellular matrix (ECM) proteins and consequently is able to affect proliferation and migration of cancer cells and angiogenesis in tumours (Lindahl et al, 1994). Furthermore, Heps have been found to inhibit expression of oncogenes and to affect the immune system (Smorenburg and Van Noorden, 2001). Heparins also show both inhibitory and stimulatory effects of various proteolytic enzymes, which are essential for invasion of cancer cells and angiogenesis through the ECM (Zacharski and Ornstein, 1998; Engelberg, 1999; Smorenburg and Van Noorden, 2001). Due to the wide variety of activities of Heps, the ultimate effect of a Hep treatment on cancer progression is unpredictable. In addition, the use of a high-dose Hep has been limited by its strong anti-coagulant property, which may cause severe bleeding complications (Levine et al, 1989; Lapierre et al, 1996).
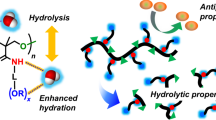
Periodate-treated, non-anticoagulant Hep-carrying polystyrene (NAC-HCPS) has been described previously as a synthetic glyco-conjugate that is soluble in water and has an amphiphilic structural unit consisting of hydrophilic polysaccharides and hydrophobic polystyrene moieties (Ishihara et al, 2000a). It has been estimated that the molecular size of NAC-HCPS is approximately 80–120 kDa and comprises of over ten periodate-oxidised, alkaline-degraded low molecular weight (IO4-LMW-) Hep chains enriched in trisulphated disaccharide structures linked to its polystyrene core (Ishihara et al, 2000a, 2000b). Non-anticoagulant Hep-carrying polystyrene shows a significantly reduced anticoagulant activity and enhanced abilities to interact with various heparin-binding growth factors, such as fibroblast growth factor-2 (FGF-2), vascular endothelial growth factor-165 (VEGF165) and hepatocyte growth factor (HGF), which are known to stimulate angiogenesis (Ishihara et al, 2000b).
The present study evaluates the effect of NAC-HCPS on malignant processes in vitro and in vivo, thereby focusing on angiogenesis. Non-anticoagulant Hep-carrying polystyrene inhibit, (i) heparin-binding growth factor-induced human microvascular endothelial cell (HMVEC) proliferation, (ii) HMVEC adhesion onto Matrigel, (iii) formation of capillary-like tubular structures on Matrigel by HMVECs in vitro, and (iv) vascularisation in tumour tissue in vivo. In addition, NAC-HCPS is an inhibitor for experimental subcutaneous tumour growth and metastasis to the lung using B16 melanoma (B16) and Lewis lung cancer (3LL) cells.
Materials and methods
Preparation of modified Heps and NAC-HCPS
Non-anticoagulant Hep-carrying polystyrene was prepared as has been reported previously (Ishihara et al, 2000a). An outline of the used chemical reaction route to synthesise modified heparins and NAC-HCPS is presented in Figure 1. Briefly, 25 g of Hep from porcine intestine (185.8 USP Units mg−1) dissolved in 400 ml of 0.1 M NaIO4 in 0.05 M sodium acetate buffer (pH 5) was stirred at 4°C for 3 days. The unreacted NaIO4 was then neutralised by addition of glycerol (25 ml), and the reaction mixture was subsequently dialysed and lyophilised. The product (non-reduced periodate-oxidised heparin; non-reduced IO4-Hep) was then degraded in an alkaline solution (pH 12) at room temperature for 30 min, and the degraded product was recovered after dialysis and lyophilisation as non-reduced periodate-oxidised, alkaline-degraded (non-reduced IO4-LMW-) Hep. To prepare reduced IO4-Hep and reduced IO4-LMW-Hep as control compounds in order to compare with NAC-HCPS, both non-reduced IO4-Hep and non-reduced IO4-LMW-Hep were reduced by mixing them with 0.2 M sodium borohydride in 0.25 M sodium bicarbonate for 3 h at 4°C. The excess borohydride in both reactions was destroyed by adding acetic acid (pH 5). The reduced IO4-Hep and reduced IO4-LMW-Hep were then recovered after neutralising with NaOH, dialysis and lyophilisation.
The non-reduced IO4-LMW-Hep (500 mg) and p-styrenemethylamine (250 mg) were dissolved in 20 ml of 50 mM N,N,N′,N′-tetramethyl-ethylenediamine (pH 4.75), after which 1 ml of 0.8 mM NaCNBH3 was added. The reaction mixture was stirred for 24 h at room temperature, dialysed and lyophilised to yield a white powder (heparin-styrene monomer). This powder (100 mg) and 2 mg of potassium peroxodisulphate were dissolved in 1 ml of distilled water and the polymerisation was carried out at 60°C for 24 h under dried N2 gas. The reaction solution was then slowly poured into an excess amount of ethanol to yield a polymeric precipitate. Water-soluble impurities were separated from the precipitate using ultra-filtration and finally the NAC-HCPS was obtained as a white powder after lyophilisation (Ishihara et al, 2000a). The weight fraction of NAC-Hep (non-reduced IO4-LMW-Hep) component in the NAC-HCPS was estimated to be 92% using a carbazole assay (Ishihara et al, 2001).
Anti-coagulant activity
Blood plasma was drawn from a femoral artery of a male New Zealand white rabbit (3 kg, Kitayama Labs Inc., Japan) anaesthetised with an intramuscular injection containing xylazine (12 mg) and ketamin (40 mg). The indicated concentration of native Hep, IO4-Hep, IO4-LMW-Hep or NAC-HCPS was added to 10 ml of plasma, and the activated partial thromboplastin time (APTT) and prothrombin time (PT) were determined.
Cell culture
Lewis lung cancer cells (3LL) were obtained from the Cancer Cell Repository (CCR) Institute of Development, Aging and Cancer Tohoku University, Sendai, Japan. B16 melanoma cells (B16) were obtained from the RIKEN Cell Bank, Saitama, Japan. These malignant cells and fibroblasts (human dermal fibroblast, Takara Biochemical Corp. Ohtsu, Japan) were grown in Dulbecco's modified Eagle's medium (DMEM, Life Technologies Oriental Inc., Tokyo, Japan) supplemented with 10% heat-inactivated feotal bovine serum (FBS), antibiotics (100 U ml−1 penicillin G and 100 μg ml−1 streptomycin) under the atmosphere of 5% CO2 in air and 100% relative humidity. Human microvascular endothelial cells (HMVEC, Takara Biochemical Corp., Ohtsu, Japan) were grown in medium 199 (Life Technologies Oriental Inc., Tokyo, Japan) supplemented with 10% heat-inactivated FBS, antibiotics (100 U ml−1 penicillin G and 100 μg ml−1 streptomycin) and 10 ng ml−1 fibroblast growth factor-2 (FGF-2, R&D Systems, Minneapolis, MN, USA). The cells used in this study were between the 4th and 8th passage.
Cell growth assay in vitro
Fibroblasts, 3LL and B16 cells (5 × 103 per well) were seeded on 96-well tissue culture plates (Falcon) in 100 μl of DMEM containing the same FBS and antibiotics as mentioned above, as well as the indicated concentration of either Hep, IO4-Hep, IO4-LMW-Hep or NAC-HCPS, and grown for 3 days. Human microvascular endothelial cells (5 × 103 per well) were seeded on 96-well tissue culture plates in 100 μl of medium 199, containing (i) the same FBS and antibiotics as mentioned above, (ii) the indicated concentration of either Hep, IO4-Hep, IO4-LMW-Hep or NAC-HCPS, and (iii) one of the growth factors (either 4 ng ml−1 of VEGF165, 10 ng ml−1 of FGF-2 or 20 ng ml−1 of HGF), and grown for 5 days. After incubation, the depleted medium was replaced with 100 μl of fresh medium including 10 μl of WST-1 reagent (Cell Counting Kit, Dojindo, Kumamoto, Japan) was added to each well, and the optical density (OD) was read at 450 nm in an Immuno Mini plate reader (Nunc InterMed Japan, Tokyo) after 1 h incubation at 37°C. Results are expressed as percentage, using the mean value of controls (without any heparinoid).
Cell adhesion onto Matrigel-coated plate
Human microvascular endothelial cells (1 × 105 cells per well) were plated on a Matrigel (20 μl of 0.5% DMEM solution per well, Collaborative Biomedical Products, Two Oak Park, Bedford, MA, USA) coated 24-well tissue culture plate in 1 ml of medium 199, containing the same FBS, antibiotics and the indicated concentration of either Hep, IO4-Hep, IO4-LMW-Hep or NAC-HCPS without 10 mg ml−1 FGF-2. Similarly B16 and 3LL cells (1 × 105 cells per well) were plated on the Matrigel-coated 24-well tissue culture plate in DMEM, containing the same FBS, antibiotics and the indicated concentration of either Hep, IO4-Hep, IO4-LMW-Hep or NAC-HCPS. After 1 h incubation, the used medium was removed and the Matrigel-coated wells were gently rinsed five times with PBS to remove non-binding cells. The fresh medium (450 μl) and 50 μl of WST-1 reagent (cell counting kit; Dojindo) was added to each well, and the optical density (OD) of the medium was measured at 450 nm in the Immuno Mini plate reader after 1 h incubation at 37°C.
Tubular formation of HMVECs
Human microvascular endothelial cells (5 × 104 cells per well) were seeded on a Matrigel- (50 μl of 1% DMEM solution per well) coated 96-well tissue culture plate in 100 μl of medium 199, containing the same FBS, antibiotics without 10 ng ml−1 FGF-2, and the indicated concentration of either Hep, IO4-Hep, IO4-LMW-Hep or NAC-HCPS as given above. After 8 h incubation, the formation of tube-like structures by HMVEC was examined microscopically and photographed at × 100 magnification. These micrographs were scanned with a film scanner and analysed using an image analyser (NIH Image, Ver. 1.60, NIH, Bethesda. MD, USA). The total length of a tube-like structure was expressed as percentage of the mean value and related to control without any heparinoid.
Tumour cell invasion assay
The effect of NAC-HCPS on the invasion activity of tumour cells was also evaluated using a growth factor-reduced Matrigel invasion chamber (for a 24-well plate, 8 μm pore size, Becton Dickinson Labware, Bedford, MA, USA) according to the method described by Albini et al (1987) with some minor modifications. Briefly, fresh media (DMEM, 0.75 ml) containing 0.1wt% BSA, 10wt% FBS as a chemo-attractant, and the indicated concentration of either Hep, IO4-Hep, IO4-LMW-Hep, or NAC-HCPS were added to the wells of the plate (the lower chamber). The upper chamber had been pre-coated with Matrigel by the manufacturer. Tumour (3LL or B16) cells were suspended in DMEM containing 0.1% BSA and the indicated concentration of either Hep, IO4-Hep, IO4-LMW-Hep or NAC-HCPS at a cell density of 5 × 104 cells ml−1, and the cell suspensions (0.5 ml) were added into the upper chamber. After 18 h incubation, non-invading cells were gently removed from the upper surface of the membrane by wiping with a cotton swab. The invaded cells to the lower side of the membrane were stained with 0.4% Trypan blue solution and counted through microscopic observation. Invasion rates were calculated according to the following equation:

Tumour growth in vivo
Male C57BL/6 mice (6-7 weeks old) were purchased from Clea Japan Inc., Tokyo, Japan. Tumour (3LL or B16) cells were trypsinised and suspended in Hanks' balanced salt solution (HBSS). Tumour cells (1 × 107) in 100 μl of HBSS were implanted into the dorsal subcutis of the mice. After tumours had reached to a volume of 100∼200 mm3 around 14 days (defined as day 1), 200 μl of IO4-Hep, IO4-LMW-Hep or NAC-HCPS (each 10 mg ml−1 of PBS solution) was subcutaneously administered around the tumour daily for another 6 days. Control mice were administered the same volume of only PBS (200 μl per injection). The size of a tumour on day 1 and day 8 was measured with calipers and tumour volume was estimated as length × width × height × π/6. The growth rate of a tumour was then calculated as volume (day 8)/volume (day 1). The 3LL and B16 tumour volumes of control on day 8 were 3200±400 and 4300±500 mm3, respectively. Each experimental group was composed of eight mice. Data were compared with the mean volume of the PBS treated group (represented as 100%).
Vascularity of the tumour
The NAC-HCPS-treated and control tumours of 3LL cells on day 8 were fixed in 10% neutral buffered formaldehyde, and embedded in paraffin for immuno-histochemical study. To evaluate the microvessel density of the tumour, CD34 as an endothelial cell (vessel) marker was stained by an indirect method (Tomisawa et al, 1999; Oshika et al, 2000). After each section (4 μm thick) was dehydrated and treated with 0.6% hydrogen peroxide in methanol for 45 min, slides were autoclaved for antigen retrieval (121°C 15 min). Slides were then incubated with 5% normal goat serum for 60 min and reacted with rat anti-murine CD34 monoclonal antibody (1 : 20, Hycult Biotechnology, Uden, The Netherlands) at 4°C, overnight. Peroxidase-conjugated anti-rat IgG (1 : 200, Amersham Life Science, Buckinghamshire, UK) was used as the second antibody at room temperature for 60 min and the interactions were visualised with 3,3′-diaminobenzidine-chromogen (DAKO Japan, Kyoto). Finally, nuclear counterstaining was carried out with Mayer's haematoxylin. In each section, five randomised areas (microscopic fields, × 100 magnificant) that were considered to show the largest vessel density, were photographed, and CD34-stained vessels were counted. Each experimental group was composed of six mice. Data have been compared with the average value in PBS treated tumours, defined as 100%.
Experimental metastasis
Mice were injected intravenously with 3 × 105 cells of either 3LL or B16 cells in 100 μl PBS through a lateral tail vein. From day 1 to day 7, either IO4-Hep, IO4-LMW-Hep or HCPS (1 mg per 100 μl PBS) or 100 μl of PBS only was administered intraveneously once a day. All mice were sacrificed day 14 after the tumour cells were injected, and the lungs of each mouse were removed. Lungs were then fixed in Bouin's solution overnight and the surface tumour nodules were counted under a stereoscopic microscope. The numbers of 3LL and B16 tumour nodules in control (PBS-treated) were 250±50 per mouse and 180±30 per mouse, respectively. Each experimental group was composed of eight mice. Data were evaluated against the mean values of the PBS treated group (represented as 100%).
Statistical analysis
All summarised data are expressed as the mean value±s.e. Comparisons between means of multiple groups were analysed by one-way analysis of variance and Scheffe's multiple comparisons test. All statistical analyses were carried out using the StatView (version 5.0) statistical package (Abacus Concepts Inc., Berkeley, CA, USA). All animal experiments have been carried out with ethical committee approval of the National Defense Medical College, Tokorozawa, Saitama, Japan. The ethical guidelines that were followed meet the standards required by Cancer Research UK guidelines (Workman et al, 1998).
Results
Anti-coagulant activity of NAC-HCPS
Addition of each Hep, IO4-Hep, IO4-LMW-Hep, and NAC-HCPS prolonged the coagulation time of rabbit plasma in a dose-dependent manner (Figure 2A, APTT). APTT of the rabbit plasma without any heparinoids was about 30 s. At a concentration of 100 μg ml−1, Hep greatly prolonged APTT to about 800 s, while IO4-Hep, IO4-LMW-Hep and NAC-HCPS prolonged APTT to about 300, 160 and 160 s, respectively. As shown in Figure 2B, the PT of rabbit plasma without any heparinoid is about 7 s. While Hep strongly prolonged PT to about 27 s at the concentration of 100 μg ml−1, IO4-Hep, IO4-LMW-Hep and NAC-HCPS only prolonged the PT to 8 to 10 s. Since the periodate oxidation of Hep is known to destruct a penta-saccharide structure which interacts with antithrombin III (Conrad and Guo, 1991), the remainder of the anticoagulant activities of IO4-Hep, IO4-LMW-Hep and NAC-HCPS may result from interactions with other anticoagulant factors, such as heparin co-factor II (Bourin and Lindahl, 1993).
Effect of NAC-HCPS on cell growth in vitro
Human microvascular endothelial cells were able to grow in medium in the presence of 10% FBS without addition of a specific growth factor. When VEGF165, FGF and HGF were added to the culture medium, the growth rate of HMVEC increased to 1.2–1.7-fold when compared to the control. Horizontal lines in Figure 3A,B,C show the level of cell growth in DMEM containing 10% FBS in the absence of exogenous growth factors. While addition of low concentrations (below 8 μg ml−1) of Hep, IO4-Hep or IO4-LMW-Hep to the medium did not influence the growth of HMVEC in the presence of each growth factor, high concentrations (more than 32 μg ml−1) slightly inhibited the growth in a dose-dependent manner (Figure 3A,B,C). On the other hand, NAC-HCPS inhibited the growth factor-induced HMVEC growth in a dose-dependent manner, even at low concentrations (<2 μg ml−1).
Effect of NAC-HCPS on growth factor-stimulated HMVEC growth. (A) VEGF165, (B) FGF-2, (C) HGF. Cell growth incubated with a growth factor in the absence of heparinoid was defined as 100% growth, and the data were calculated as a percentage. The horizontal line in each panel represents the level of cell growth obtained in the absence of both growth factor and heparinoid. The results represent the mean±s.e. in triplicate.
The doubling times of fibroblast and 3LL cell growth in DMEM containing 10% FBS and antibiotics were 25 and 17 h, respectively, and the cell growth was not influenced upon addition of either Hep, IO4-Hep, IO4-LMW-Hep or NAC-HCPS up to 500 μg ml−1 (Figure 4A,B). However, only NAC-HCPS inhibited B16 cell growth in a dose-dependent manner (Figure 4C). The doubling time of B16 cell growth in the control culture and 500 μg ml−1 NAC-HCPS containing culture were 18 and 23 h, respectively.
Effect of NAC-HCPS on tubular formation of HMVECs
Human microvascular endothelial cells are well known to form capillary-like tubular structures when seeded on Matrigel (Collen et al, 2000). The effect of NAC-HCPS in culture media on this tubular formation of HMVEC was compared to that of Hep, IO4-Hep and IO4-LMW-Hep. Figure 5A shows representative microphotographs of tubular formation of HMVEC cultured in the presence of respectively 2 or 32 μg ml−1 of NAC-HCPS, Hep, IO4-Hep and IO4-LMW-Hep. While Hep, IO4-Hep, and IO4-LMW-Hep showed a low inhibitory effect on the tubular formation up to concentrations of 100 μg ml−1 (Figure 5B), NAC-HCPS exhibited a strong inhibition on the tubular formation, even at low concentration (2 μg ml−1, Figure 5A,B).
Effect of NAC-HCPS on tubular formation of HMVEC. (A) Photomicrographs (original magnification: × 100) of the tubular formation of HMVEC cultured with 2 or 32 μg ml−1 of NAC-HCPS, Hep, IO4-Hep and IO4-LMW-Hep for 8 h on Matrigel-coated plates. Results are representatives of three independent experiments. (B) The quantitative evaluations of tubular formation of HMVEC cultured with various concentrations of NAC-HCPS, Hep, IO4-Hep and IO4-LMW-Hep.
Effect of NAC-HCPS on tumour cell invasion
The inhibitory effect of NAC-HCPS on the migration and invasion of tumour cells (3LL and B16) was examined using a Matrigel invasion chamber (Albini et al, 1987). When 3LL and B16 cells were cultured on the Matrigel invasion chamber without any heparinoid, about 200 and 80 cells were invaded into the lower side of the membrane, respectively. While both cell types showed a slightly enhanced invasive activity in the presence of 4 μg ml−1 of Hep, IO4-Hep, and IO4-LMW-Hep, the invasive activities were reduced in the presence of high concentrations (100 μg ml−1) of Hep, IO4-Hep, and IO4-LMW-Hep (Figure 6A,B). On the other hand, the invasive activity of both cell types in the presence of NAC-HCPS was strongly inhibited, even at a low concentration (4 μg ml−1). Therefore, it is suggested that NAC-HCPS possesses an anti-invasive activity for tumour cells.
Effect of NAC-HCPS on tumour cell invasion. Tumour cells (3LL (A) and B16 (B)) were seeded on a 8 μm pore size membrane coated with Matrigel. After 18 h incubation, invaded cells were stained and counted. The invasion rates were calculated as described in Materials and Methods. Results represent the mean±s.e. of four independent determinations.
Effect of NAC-HCPS on endothelial and tumour cell adhesions to Matrigel-coated plates
The adhesions of HMVECs and tumour cells (3LL and B16) to Matrigel-coated plates may be an important first step in the tubular formation of HMVECs on the Matrigel, as well as tumour cell invasion through the Matrigel invasion chamber, respectively. We examined the effect of NAC-HCPS on both HMVEC and tumour cell adhesion to Matrigel-coated plates. All HMVEC, 3LL and B16 cells adhered to the Matrigel-coated plates within 1 h in the absence of NAC-HCPS (Figure 7) showing spreading shapes on the surface. On the other hand, NAC-HCPS inhibited adhesion of all the HMVEC, 3LL and B16 cells to the Matrigel-coated plates in a concentration-dependent manner (Figure 7). Furthermore, almost all cells of these three cell types retained their spherical shapes in the presence of high concentrations of NAC-HCPS (20 and 100 μg ml−1) up to 5 h (data not shown). However, neither Hep, IO4-Hep nor IO4-LMW-Hep showed the cell shape-retaining effect.
Effect of NAC-HCPS on tumour growth in vivo
A measurable tumour (tumour volume: 100∼200 mm3) was formed 14 days after implantation of tumour cells (3LL or B16). As shown in Figure 8A, IO4-Hep and IO4-LMW-Hep reduced subcutaneous induced tumour growth of 3LL cells to various extents. NAC-HCPS more strongly inhibited tumour growth to about 40% of the PBS treated group (P= 0.0065, vs PBS) than IO4-Hep and IO4-LMW-Hep. On the other hand, while IO4-Hep and IO4-LMW-Hep did not significantly reduce the subcutaneous induced tumour growth of B16 melanoma (Figure 8B), NAC-HCPS significantly inhibited the tumour growth to about 10% of the PBS treated group (P<0.0001, vs PBS).
Effect of NAC-HCPS on subcutaneous induced tumour growth of 3LL (A) and B16 (B) cells in mice. Tumour cells (1 × 107) were implanted into the dorsal subcutis of mice. After tumours reached a measurable size (100∼200 mm3), 2 mg per 200 μl PBS of NAC-HCPS, IO4- Hep, IO4-LMW-Hep or PBS (200 μl) only was daily administered subcutaneously in the vicinity of the tumour for 7 days. Growth rates were calculated as described in Materials and Methods. Data were compared with the average tumour volume of the PBS treated group, defined as 100%.
Effect of NAC-HCPS on vascularity of the tumour in vivo
To evaluate the effect of NAC-HCPS on anti-angiogenesis, immuno-histochemical staining of murine CD34 of NAC-HCPS treated and control tumours of 3LL cells were carried out (Tomisawa et al, 1999; Oshika et al, 2000). Representative microphotographs of CD34 immuno-localisation in controls (PBS-treated) and NAC-HCPS treated subcutaneous induced tumours are shown in Figure 9A,B. In PBS treated mice, many CD34 positive stained vessels were diffusely located and clearly formed tube-like structures in the tumour. On the other hand, CD34 positive stained vessels were nearly absent in the NAC-HCPS treated tumours and tube-like structures were not observed. As shown in Figure 9C, NAC-HCPS significantly reduced the number of CD34 positive vessels (P=0.0031), suggesting that NAC-HCPS significantly inhibited angiogenesis in tumours.
Effect of NAC-HCPS on 3LL-tumour vascularisation. Vascularisation of the 3LL-tumour, evaluated immuno-histochemically with anti-murine CD34, markedly decreased in NAC-HCPS treated 3LL-tumours (B) when compared with PBS treated 3LL-tumours (A). The quantitative evaluation of the vascularisation (C) was carried out as described in Materials and Methods.
Effect of NAC-HCPS on experimental metastasis
To evaluate the inhibitory effect of NAC-HCPS on lung colony formation of tumour cells (3LL or B16), IO4-LMW-Hep, IO4-Hep and NAC-HCPS (each 1 mg per 100 μl PBS) was intravenously injected daily for 7 days after injection of the tumour cells. Therefore, Hep was excluded in this study. As shown in Figure 10A, IO4-LMW-Hep, IO4-Hep and NAC-HCPS inhibited lung colonisation of 3LL cells. Similarly in Figure 10B, all IO4-LMW-Hep, IO4-Hep and NAC-HCPS also showed lung colonisation inhibition of B16 cells. Furthermore, in IO4-LMW-Hep, IO4-Hep and PBS treated mice, a number of 3–20 tumour colonies of 3LL or B16 cells in liver were always observed in each mouse, while in NAC-HCPS treated mice, no colony formation of tumour cells in liver was observed (data not shown). Thus, NAC-Heps, especially NAC-HCPS, possess significant anti-metastasis activity of 3LL and B16 cells.
Effect of NAC-HCPS on lung colonisation of 3LL cells (A) and B16 cells (B) in mice. Both tumour cells (3 × 105) were intraveneously injected through the lateral tail vein. From day 1 to day 7, either NAC-HCPS, IO4-Hep, IO4-LMW-Hep (1 mg per 100 μl of PBS) or 100 μl of PBS only was daily administered intraveneously through the lateral tail vein, and colony numbers on the lung surface in each mouse were counted on day 14.
Discussion
Heparin is clinically used as an antithrombotic agent, but its high dose use has been limited by its strong intrinsic anti-coagulant property itself, causing severe bleeding complications (Levine et al, 1989). If Hep could be modified to minimise its anti-coagulant property and to enhance its activities to inhibit tumour growth and metastasis, then such a modified Hep would be a very useful drug in treating malignant diseases. Periodate-oxidised (IO4-) Hep and periodate-oxidised, alkaline-degraded low molecular weight (IO4-LMW-) Hep (Fransson and Carlstedt, 1974; Fransson, 1978) are known for not having a specific pentasaccharide structure to interact with antithrombin III (Conrad and Guo, 1991), and therefore its anti-coagulant activity (APTT and PT) is much lower than Hep (Figure 2). We previously reported the preparation of NAC-HCPS using the IO4-LMW-Hep (Ishihara et al, 2000a). In this study, we have demonstrated that NAC-HCPS inhibits subcutaneously induced tumour growth and metastasis to lung of B16 melanoma and 3LL (Lewis lung cancer) cell line.
In the present study, NAC-HCPS when compared to Hep, IO4-Hep and IO4-LMW-Hep, has strong anti-angiogenic properties. This inhibitory effect of NAC-HCPS can not be ascribed to cytotoxicity, since it has been found that NAC-HCPS in concentrations up to 500 μg ml−1 do not inhibit the HMVEC growth in the absence of those growth factors (data not shown). NAC-HCPS inhibited the adhesion of HMVECs and tumour cells to the Matrigel-coated plate, as well as the tubular formation of HMVEC on Matrigel. The inhibitory effect of NAC-HCPS is probably due to inhibition of the cell adhesion to the Matrigel as well as inhibition of heparin-binding growth factors. Moreover, endothelial cells in the extracellular matrix need binding to adhesive proteins to initiate invasion and migration (McCathy et al, 1990). Heparins, especially NAC-HCPS, can effectively bind to various adhesive proteins such as fibronectin, laminin and collagen, and thus may affect cell adhesion and tubular formation. Finally, NAC-HCPS markedly reduced the number of CD34-positive vessels (a marker of microvascular endothelial cells) in subcutaneous 3LL tumours (Tomisawa et al, 1999; Oshika et al, 2000). The above results demonstrate that NAC-HCPS with its reduced anticoagulant property has a strong anti-angiogenesis. This anti-angiogenesis activity may be the explanation for the observed in vivo inhibition of experimental subcutaneous tumour growth.
In this study, it has been demonstrated that NAC-HCPS inhibits the adhesion of tumour cells to Matrigel-coated plates, probably due to the Hep-clustering effect of NAC-HCPS (Figure 7). In addition, immobilization of Hep onto Matrigel was important for the inhibitory effect of NAC-HCPS on tumour cell adhesion to Matrigel. As we reported previously, NAC-HCPS is effectively adsorbed to various polymeric surfaces (Ishihara et al, 2000a), collagen (type I)-substratum (Ishihara et al, 2001) and Matrigel (data not shown) through a hydrophobic interaction between the hydrophobic surface and polystyrene core of NAC-HCPS. And cell adhesion of tumour cells (B16 and 3LL) were similarly inhibited by immobilisation of NAC-HCPS on the Matrigel (data not shown).
Invasive properties are characteristic of malignant cells, and essential to tumour growth. Tumour cells use specific enzymes to solubilise extracellular matrix during tumour invasion. This degradation of the extracellular matrix takes place at highly localised regions in close vicinity to the cancer, where active proteolytic enzymes outbalance natural protease inhibitors present in the extracellular environment (Basbaum and Werb, 1996). These proteases are produced by either inflammatory cells, stromal cells or the tumour cell themselves (Liotta, 1992). Heparin, chemically modified heparins and related sulphated polysaccharides are known to be effective inhibitors for heparanase (Irimura et al, 1986; Vlodavsky et al, 1994; Lapierre et al, 1996) and various matrix metalloproteases (MMPs) including MMP-1, -2, -3 and -9 (Kenagy et al, 1994; Gogly et al, 1998). MMP-2 and -9 are suggested to play a major role in metastasis (Kugler, 1999; Westermarck and Kahari, 1999). Heparanase activity has also been found to correlate with the metastatic potential of various types of cancer cells (Nakajima et al, 1988). In this study the dose-dependent inhibition of NAC-HCPS on the invasion of tumour cells into Matrigel has been observed (Figure 6). It is possible that an enhanced inhibition of active proteolytic enzymes, as well as inhibition of adhesion of tumour cells to Matrigel by NAC-HCPS result in the strong inhibition of the tumour cell invasions. Tumour cell adhesion to sub-endothelial matrix and the subsequent invasion into the matrix are common pathways for tumour cells to escape from blood flow. The observed inhibition of metastasis by NAC-HCPS seems to be caused through the inhibition of adhesion and invasion of tumour cells (B16 and 3LL).
Our additional studies also have revealed that IO4-LMW-Hep and NAC-HCPS have about a 10-fold smaller anticoagulant activity (APTT) than native Hep. The residual anticoagulant activity of NAC-HCPS is probably mediated by interaction with heparin co-factor II, and not antithrombin III (Conrad and Guo, 1991; Lapierre et al, 1996). In many tumour types, fibrin is a major component of the initial stroma (Costantini and Zacharski, 1992). Fibrin provides a scaffold for both invasive cancer and endothelial cells, thereby contributing to tumour growth and neo-vascularisation (Dvorak et al, 1987). The structure and mechanical properties of the fibrin matrix play a regulating role in the formation of capillary-like tubular structures (Nehls and Herrmann, 1996). Hep with its anticoagulant activity is thus expected to inhibit the formation of fibrin and microthrombi. Whether the low anticoagulant activity of NAC-HCPS contributes to its anti-tumour and anti-angiogenesis properties remains to be determined.
Compared with sulphated polysaccharides like Hep, NAC-HCPS has the advantage of exhibiting less toxicity due to its reduced anti-coagulant activity. The subcutaneous haemorrhages were never observed in mice injected with the same amount of NAC-HCPS, and the NAC-HCPS treated mice lived longer. Furthermore, when 1 mg of NAC-HCPS was intravenously injected daily for 7 consecutive days, only minor increases for the values of GOT (glutamic-oxaloacetic transaminase), GPT (glutamic-pyruvic transaminase), BUN (blood urea nitrogen), and Crea (creatinine) were observed, returning to normal values within 7 days after the final injection (data not shown). However, sufficient data are not yet available of the complete toxicity profile of NAC-HCPS, and standard toxicologic and metabolic studies should be carried out in more detail to confirm the clinical safety of NAC-HCPS.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Albini A, Iwamoto Y, Kleinman HK, Martin GR, Aaroson SA, Kozlowski JM, McEwan RN (1987) A rapid in vitro assay for quantitating the invasion potential of tumour cells. Cancer Res 47: 3239–3245
Basbaum CB, Werb Z (1996) Focalized proteolysis: Spatial and temporal regulation of extracellular matrix degradation at the cell surface. Curr Opin Cell Biol 8: 731–738
Bourin MC, Lindahl U (1993) Glycosaminoglycans and the regulation of blood coagulation. Biochem J 289: 313–330
Collen A, Smorenburg SM, Peters E, Lupu F, Koolwijk P, Von Noorden C, Hinsbergh VWM (2000) Unfractionated and low molecular weight heparin affect fibrin structure and angiogenesis in vitro. Cancer Res 60: 6192–6200
Conrad HE, Guo Y (1991) Structural analysis of periodate-oxidized heparin. In Heparin And Related Polysaccharides, Advances in Experimental Medicine and Biology 313 Lane DA, Bjork I, Lindahl U (eds) pp 31–36, New York: Plenum Publishing
Costantini V, Zacharski LR (1992) The role of fibrin in tumour metastasis. Cancer Metastasis Rev 11: 283–290
Dvorak HF, Harvey VS, Estrella P, Brown LF, McDonagh J, Dvorak AM (1987) Fibrin containing gels induce angiogenesis. Implications for tumour stroma generation and wound healing. Lab Invest 57: 673–686
Engelberg H (1999) Actions of heparin that may affect the malignant process. Cancer 85: 257–272
Fransson L-A, Carlstedt I (1974) Alkaline and Smith degradation of oxidized dermatan sulphate-chondroirin sulphate copolymers. Carbohyr Res 36: 349–358
Fransson L-A (1978) Periodate oxidation of the d-glucuronic acid residues in heparan sulphate and heparin. Carbohydr Res 62: 235–244
Gogly B, Hornebeck W, Groult N, Godeau G, Pellat B (1998) Influence of heparins on the interleukin-1-beta-induced expression of collagenase, stromelysin-1, and tissue inhibitor of metalloproteinase-1 in human gingival fibroblasts. Biochem Pharmacol 56: 1447–1454
Irimura T, Nakajima M, Nicolson GL (1986) Chemically modified heparins as inhibitors of heparan sulfate specific endo-beta-glucuronidase (heparanase) of metastatic melanoma cells. Biochemistry 25: 5322–5328
Ishihara M, Ono K (1998) Structure and function of heparin and heparan sulfate: Heparinoid library and modification of FGF-activities. Trends Glycosci Glycotechnol 10: 223–233
Ishihara M, Saito Y, Ono K, Ishikawa K, Hattori H, Akaike T, Kurita A (2000a) Heparin-carrying polystyrene to mediate cellular attachment and growth via interaction with growth factors. J Biomed Mater Res 50: 144–152
Ishihara M, Ono K, Ishikawa K, Hattori H, Saito Y, Yura H, Akaike T, Ozeki Y, Tanaka S, Mochizuki H, Kurita A (2000b) Enhanced ability of heparin-carrying polystyrene (HCPS) to bind to heparin-binding growth factors and to inhibit growth factor-induced endothelial cell growth. J Biochem 127: 797–803
Ishihara M, Sato M, Hattori H, Saito Y, Yura H, Ono K, Masuoka K, Kikuchi M, Fujikawa K, Kurita A (2001) Heparin-carrying polystyrene (HCPS)-bound collagen substratum to immobilize heparin-binding growth factors and to enhance cellular growth. J Biomed Mater Res 56: 536–544
Kenagy RD, Nikkari ST, Weigus HG, Clowes AW (1994) Heparin inhibits the induction of three matrix metalloproteases (stromelysin, 92kD gelatinase, and collagenase) in primate arterial smooth muscle cells. J Clin Invest 93: 1987–1993
Kjellen L, Lindahl U (1991) Proteoglycans: Structure and interaction. Annu Rev Biochem 60: 443–475
Kugler A (1999) Matrix metalloproteinases and their inhibitors. Anticancer Res 19: 1589–1592
Lapierre F, Holme K, Lam L, Tressler RJ, Storm N, Wee J, Stack RJ, Castellot J, Tyrrell DJ (1996) Chemical modifications of heparin that diminish its anticoagulant but preserve its heparanase-inhibitory, angiostatic, anti-tumour and anti-metastatic properties. Glycobiology 6: 355–366
Levine MN, Hirsh J, Kelton JG (1989) Heparin-induced bleeding. In Heparin: Chemical and Biological Properties, Clinical Applications Lane DA, Lindahl U (eds) pp 517–531, Forida: CRC Press Inc
Lindahl U, Lidholt K, Spillmann D, Kjellen L (1994) More to “heparin” than anticoagulation. Thromb Res 75: 1–32
Liotta LA (1992) Cancer cell invasion and metastasis. Sci Am 266: 54–59
McCathy JB, Skubitz AP, Qi Z, Mickelson DJ, Klein DJ, Furcht LT (1990) RGD-independent cell adhesion to the carboxy-terminal heparin-binding fragment of fibronectin involves heparin-dependent and -independent activities. J Cell Biol 110: 777–787
Nakajima M, Irimura T, Nicolson GL (1988) Heparanases and tumour metastasis. J Cell Biochem 36: 157–167
Nehls V, Herrmann R (1996) The configuration of fibrin clots determined capillary morphogenesis and endothelial cell migration. Microvasc Res 51: 347–364
Oshika Y, Nakamura M, Tokunaga T, Ohnishi Y, Abe Y, Tsuchida T, Tomii Y, Kijima H, Yamazaki H, Ozeki Y, Tomaoki N, Yamazaki H (2000) Ribozyme approach to downregulate vascular endothelial growth factor (VEGF) 189 expression in non-small cell lung cancer (NSCLC). Eur J Cancer 36: 2390–2396
Smorenburg SM, Van Noorden C (2001) The complex effects of heparins on cancer progression and metastasis in experimental studies. Pharmacol Rev 53: 93–105
Tomisawa M, Tokunaga T, Oshika Y, Tsuchida T, Fukushima Y, Sato H, Kijima H, Yamazaki Y, Ueyama Y, Tamaoki N, Nakamura M (1999) Expression pattern of vascular endothelial growth factor isoform is closely correlated with tumour stage and vascularisation in renal cell carcinoma. Eur J Cancer 35: 133–137
Vlodavsky I, Mohsen M, Lider O, Svahn CM, Ekre HP, Vigoda M, Ishai-Michaeli R, Peretz T (1994) Inhibition of tumour metastasis by heparanase inhibiting species of heparin. Invasion Metastasis 14: 290–302
Westermarck J, Kahari VM (1999) Regulation of matrix metalloproteinase expression in tumour invasion. FASEB J 13: 781–792
Workman P, Twentyman P, Balkwill F, Balmain A, Chaplin D, Double J, Embleton J, Newell D, Raymond R, Stables J, Stephens T, Wallace J (1998) United Kingdom Co-ordinating Committee on Cancer Research (UKCCCR) Guidelines for Welfare of Animals in Experimental Neoplasia. (Second Edition) Br J Cancer 77: 1–10
Zacharski LR, Ornstein DL (1998) Heparin and cancer. Thromb Haemost 80: 10–23
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Ono, K., Ishihara, M., Ishikawa, K. et al. Periodate-treated, non-anticoagulant heparin-carrying polystyrene (NAC-HCPS) affects angiogenesis and inhibits subcutaneous induced tumour growth and metastasis to the lung. Br J Cancer 86, 1803–1812 (2002). https://doi.org/10.1038/sj.bjc.6600307
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6600307
Keywords
This article is cited by
-
Low molecular weight heparin and cancer survival: clinical trials and experimental mechanisms
Journal of Cancer Research and Clinical Oncology (2016)
-
Heparin–Paclitaxel Conjugates Using Mixed Anhydride as Intermediate: Synthesis, Influence of Polymer Structure on Drug Release, Anticoagulant Activity and In Vitro Efficiency
Pharmaceutical Research (2009)
-
Tumor Endothelial Cell Targeted Cyclic RGD-modified Heparin Derivative: Inhibition of Angiogenesis and Tumor Growth
Pharmaceutical Research (2008)
-
Combination Therapy of Heparin–Deoxycholic Acid Conjugate and Doxorubicin against Squamous Cell Carcinoma and B16F10 Melanoma
Pharmaceutical Research (2008)
-
Antiangiogenic and Apoptotic Properties of a Novel Amphiphilic Folate-Heparin-Lithocholate Derivative Having Cellular Internality for Cancer Therapy
Pharmaceutical Research (2007)