Abstract
Human cancers with a high frequency microsatellite instability phenotype develop due to defects in DNA mismatch repair genes. Silencing of a DNA mismatch repair gene, hMLH1 gene, by promoter hypermethylation is a frequent cause of the microsatellite instability-H phenotype. Using methylation specific PCR we investigated the methylation status of the hMLH1 gene promoter in 17 solitary gastric cancers (12 microsatellite instability-H and five microsatellite stable tumours from 17 patients), and 13 multiple gastric cancers (eight microsatellite instability-H, one low frequency microsatellite instability-L and four microsatellite stable tumours from five patients) and also examined non-cancerous gastric mucosa both adjacent to and distant from each tumour. Expression of hMLH1 protein was evaluated by immunohistochemistry. All microsatellite instability-H tumours (20 out of 20) had evidence of methylation of hMLH1 promoter, whereas only one out of 10 microsatellite instability-L and microsatellite stable tumours did (P<0.0000005), and the methylation status correlated with hMLH1 protein expression (P<0.000003). Furthermore, methylation of the hMLH1 promoter was detected in 50% (6 out of 12) and 63% (5 out of 8) of non-cancerous gastric mucosa samples adjacent to, and in 33% (4 out of 12) and 40% (2 out of 5) of those obtained from distant portion of, solitary and multiple cancers with microsatellite instability-H. Thus both solitary and multiple gastric cancers with microsatellite instability-H have evidence of similar high levels of hMLH1 promoter hypermethylation in the surrounding non-cancerous tissue. Hypermethylation of the hMLH1 promoter occurs in non-cancerous gastric mucosa of microsatellite instability-H tumours and may increase the risk of subsequent neoplasia.
Similar content being viewed by others
Main
Microsatellite instability (MSI) due to defects in mismatch repair genes such as hMLH1 and hMSH2 is now widely recognized as an important mechanism in tumorigenesis (Aaltonen et al, 1993; Ionov et al, 1993; Thibodeau et al, 1996; Fleisher et al, 1999; Kang et al, 1999; Leung et al, 1999; Suzuki et al, 1999; Toyota et al, 1999a). MSI is reportedly present in 15–33% of solitary gastric cancers, although mutations of the hMLH1 or hMSH2 genes are rare in sporadic gastric cancers (Chong et al, 1994; Mironov et al, 1994; Strickler et al, 1994; Tamura et al, 1996). Hypermethylation of promoter region CpG islands is a common mechanism by which tumour suppressor or tumour-related genes, and DNA mismatch repair genes are inactivated (Herman et al, 1995, 1998; Kane et al, 1997; Baylin et al, 1998; Jones and Laird, 1999). Aberrant DNA methylation of promoter region CpG islands of several genes, including retinoblastoma (Rb), von Hippel-Lindau (VHL), p16, p15, APC, E-cadherin and hMLH1 has been reported in human cancers, and silencing of hMLH1 by promoter hypermethylation is the major causative event in the development of human cancers with MSI phenotype, including gastric cancers (Graff et al, 1997; Kane et al, 1997; Herman et al, 1998; Fleisher et al, 1999; Kang et al, 1999; Leung et al, 1999; Suzuki et al, 1999; Tamura et al, 2000; Tsuchiya et al, 2000).
To clarify the role of hypermethylation of the hMLH1 gene promoter in the development of multiple gastric cancers, we compared both the methylation status and expression of the hMLH1 gene, in solitary and multiple gastric cancers with and without MSI. In addition, we examined the methylation status of the hMLH1 gene in non-cancerous gastric mucosa adjacent to and distant from each tumour.
Materials and methods
Samples and DNA extraction
Thirty gastric adenocarcinomas, including 17 solitary tumours from 17 patients and 13 multiple tumours from five patients were studied. The patients ranged in age from 59 to 84 years (average 72 years). We also examined non-cancerous gastric tissue both adjacent to (at a distance of 2 mm) and distant from (at a distance of 5 cm or surgical margin) each tumour. The tumours were histologically differentiated adenocarcinomas comprising 28 early cancers (depth of invasion limited to the mucosa or submucosa) and two advanced cancers. Specimens were fixed in 10% buffered formalin. The carcinomas were cut serially into 5 mm slices in parallel with the lesser curvature and then embedded in paraffin. From one block that included the maximum diameter of the tumour, we prepared two sets of 3 and 10 μm thick serial sections. The 3 μm thick sections were used for haematoxylin-eosin and immunohistochemical stainings, and each set of the 10 μm thick sections for DNA extraction of cancerous or non-cancerous DNA. To avoid contamination, either of cancerous or non-cancerous the area was carefully dissected using disposable scalpels by a reference to the serial haematoxylin-eosin stained sections under the microscope. DNA extraction was as described by Goelz et al (1985). All samples had been previously screened for MSI using 12 microsatellite markers, i.e. D2S115, D4S404, D5S178, IL9, D6S265, D7S490, D11S900, MYH6, TP53, D17S1176, D18S46, and D21S1407, and defined as MSI-H if there were more than 30% unstable loci, MSI-L less than 30% unstable loci, and microsatellite stable (MSS) no unstable loci (Ohmura et al, 2000; Ogata et al, 2001). Our samples constituted of 20 (12 solitary and eight multiple) MSI-H tumours, 1 MSI-L tumour and nine (five solitary and four multiple) MSS tumours.
Methylation-specific PCR
hMLH1 gene promoter methylation patterns were determined by methylation specific PCR (MSP), as described previously (Fleisher et al, 1999). MSP distinguishes unmethylated from methylated alleles of a given gene based on sequence changes that are produced following bisulfite treatment of DNA, which converts unmethylated cytosines to uracils, while leaving methylated cytosines unaffected. Subsequent PCR using primers specific to sequences that correspond to either methylated or unmethylated hMLH1 gene promoter DNA was performed. The primer sequences of hMLH1 for the unmethylated reaction were 5′-TTT TGA TGT AGA TGT TTT ATT AGG GTT GT-3′ (sense) and 5′-ACC ACC TCA TCA TAA CTA CCC ACA-3′ (antisense), whereas for the methylated reaction they were 5′-ACG TAG ACG TTT TAT TAG GGT CGC-3′ (sense) and 5′-CCT CAT CGT AAC TAC CCG CG-3′ (antisense) (Fleisher et al, 1999). Briefly, 2 μg of genomic DNA was denatured by treatment with NaOH and modified by sodium bisulfite. DNA samples were then purified using a Wizard DNA purification resin (Promega, Madison, WI, USA), treated with NaOH, precipitated with ethanol, and resuspended in 30 μl water. Modified DNA was amplified in a total volume of 20 μl using GeneAmp PCR Gold Buffer (PE Applied Biosystems, Foster City, CA, USA) containing 1.0 mM MgCl2, 20 μM of each primer, 0.2 mM dNTPs, and 1 unit of Taq polymerase (AmpliTaq Gold DNA Polymerase, PE Applied Biosystems). After activation of the Taq polymerase at 95°C for 10 min, PCR was performed in a thermal cycler (GeneAmp 9700, PE Applied Biosystems) for 35 cycles, each cycle consisting of denaturation at 95°C for 15 s, annealing at 55°C for 15 s, and extension at 72°C for 30 s, followed by a final 7 min extension at 72°C. The PCR products were then loaded onto a non-denaturing 6% polyacrylamide gel, stained with ethidium bromide, and visualized under UV illumination.
Immunohistochemistry
Immunohistochemistry was performed on formalin-fixed, paraffin embedded sections using a standard labelled streptavidin-biotin system (Nichirei, Tokyo, Japan). Mouse monoclonal antibody to the hMLH1 gene product, G168-728 (PharMingen, San Diego, CA, USA), was used at 1 : 50 dilution after antigen retrieval by microwave.
Statistical analysis
Statistical comparisons were performed using Fisher's exact test. P values <0.05 were considered significant.
Results
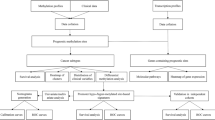
Hypermethylation of the hMLH1 gene promoter was detected in all solitary (12 out of 12) and multiple (8 out of 8) gastric cancers with MSI-H (Figure 1 and Table 1). Methylated alleles were found in none (0 out of 5) of solitary and 20% (1 out of 5) of multiple MSI-L and MSS tumours (Table 1). The MSI-L tumour did not have methylated hMLH1 gene promoter alleles. The methylation status of the hMLH1 promoter was significantly correlated with MSI status (P<0.0000005). Methylated hMLH1 alleles were also present in 50% (6 out of 12) and 63% (5 out of 8) of samples of non-cancerous gastric mucosa adjacent to, and in 33% (4 out of 12) and 40% (2 out of 5) samples of non-cancerous gastric mucosa distant from solitary and multiple gastric cancers with MSI-H (Table 1). In contrast, methylated alleles were infrequently present in none (0 out of 5) of non-cancerous mucosa adjacent to, and in 20% (1 out of 5) of non-cancerous mucosa distant from solitary gastric cancers with MSS (Table 1). Most of the methylated tumours (12 out of 12 solitary tumours and 7 out of 9 (78%) of multiple tumours) showed an apparent loss of hMLH1 protein expression (Figure 2). All nine unmethylated tumours (five solitary and four multiple tumours) and their surrounding non-cancerous mucosa had a normal expression level of hMLH1 protein. The methylation status of the hMLH1 promoter was significantly correlated with protein expression in solitary and multiple tumours (P<0.000003, Table 2).
Representative results from methylation-specific PCR (MSP) of the hMLH1 gene promoter in multiple (A) and solitary (B) gastric cancers. The presence of PCR product in lanes marked M indicates hypermethylated hMLH1 product, lanes marked U indicate unmethylated hMLH1. T, Tumour DNA; A, normal mucosa adjacent to tumour; N, normal mucosa from the surgical margin; PC, positive control; NC, negative control; SM, size marker.
Immunohistochemical staining for hMLH1 protein expression in gastric cancers with unmethylated (A) or hypermethylated (B) gene promoters. (A) Nuclear staining of hMLH1 in a MSS tumour without promoter hypermethylation (intramucosal well differentiated tubular adenocarcinoma). (B) Loss of hMLH1 expression in a MSI-H tumour with promoter hypermethylation (left, intramucosal well differentiated tubular adenocarcinoma; right, intestinal metaplastic mucosa exhibiting hMLH1 expression).
Discussion
MSI is found in 15–33% of sporadic gastric cancers, a higher incidence than that seen in other types of sporadic human cancers (Chong et al, 1994; Mironov et al, 1994; Strickler et al, 1994; Tamura et al, 1996; Ohmura et al, 2000). Furthermore, multiple gastric cancers have a higher incidence of MSI than solitary gastric cancers, although few studies have focused on the relationship between multiple gastric cancers and MSI (Nakashima et al, 1995; Yamashita et al, 2000; Ogata et al, 2001). MSI has been observed in 58.3% (7 out of 12) – 80% (4 out of 5) of multiple gastric cancer patients, and in 30.3% (10 out of 33) – 71.4% (10 out of 14) of individual tumours (Nakashima et al, 1995; Yamashita et al, 2000; Ogata et al, 2001). These data suggest that MSI may play a more important role in the development of multiple rather than solitary gastric cancers. Recent studies suggest that silencing of the hMLH1 gene by promoter hypermethylation is a major causative event in the development of human gastric cancers with MSI (Fleisher et al, 1999, 2001; Kang et al, 1999; Leung et al, 1999; Suzuki et al, 1999). hMLH1 promoter hypermethylation was observed in 62.5–100% of sporadic gastric cancers with MSI-H (Fleisher et al, 1999, 2001; Kang et al, 1999; Leung et al, 1999; Suzuki et al, 1999). The majority of these tumours also exhibited loss of hMLH1 protein expression. In our present study, hMLH1 promoter hypermethylation occurred in both solitary (12 out of 12) and multiple gastric cancers (8 out of 8) exhibiting MSI-H, and all but two tumour samples also had an apparent loss of hMLH1 protein expression. Toyota et al (1999b) examined the methylation status of multiple CpG islands in the DNA from normal gastric mucosa adjacent to gastric tumours with a CpG island methylator phenotype, and found that hypermethylation was rarely detected. Similar findings of hMLH1 gene promoter were reported by other investigators (Suzuki et al, 1999; Leung et al, 2001). In our present study, however, methylation of the hMLH1 promoter was detected in non-cancerous mucosa adjacent to both solitary (6 out of 12, 50%) and multiple (5 out of 8, 63%) gastric tumours with MSI-H. Similarly to our present results, Guo et al (2001) has recently reported a high frequency (40%; 4 out of 10) of hMLH1 methylation in non-cancerous mucosa adjacent to gastric cancer showing MSI-H. The exact cause of these discrepancies among reports remains uncertain. However, because hypermethylation originates within the flanking regions of the CpG islands (Graff et al, 1997) and the more 3′ region of hMLH1 promoter than we studied displayed a higher degree of correlation with MSI status (Deng et al, 1999; Nakagawa et al, 2001), it is possible that hMLH1 promoter was not yet fully methylated (or silenced) in non-cancerous mucosa in which reduction of hMLH1 expression was inconspicuous. Alternatively, MSI-H gastric cancers may develop through clonal expansion of fully methylated cells showing loss of hMLH1. Such a finding has been previously reported in colorectal tissue (Kuismanen et al, 1999).
Multiple gastric cancers are frequently found in the elderly, and the incidence of gastric cancers with MSI-H also correlates with age (Esaki et al, 1987; Nakashima et al, 1995; dos Santos et al, 1996; Halling et al, 1999). Furthermore, hypermethylation of the promoters of several tumour-related genes is also increased with age (Ahuja et al, 1997, 1998; Kane et al, 1997; Veigl et al, 1998). Thus, age-related methylation has the potential to behave as a mutator process resulting in the simultaneous silencing of multiple tumour related genes in aging tissues (Lipkin, 1988; Issa, 2000). While the mechanism of age-related methylation is not known, it is clear that age-related methylation only affects a subset of genes, suggesting a gene-specific susceptibility to this process (Issa, 2000). Several factors have been suggested to modulate this process, such as exogenous carcinogens, endogenously generated reactive oxygen species, and genetic differences in individuals' susceptibility to age-related methylation (Issa, 2000). Although we found frequent hypermethylation of the hMLH1 gene promoter in non-cancerous mucosa adjacent to, or distant from solitary and multiple gastric cancers with MSI-H, methylated alleles were rarely detected in similar tissues from patients with solitary gastric cancer of the MSS phenotype. We conclude that hypermethylation of the hMLH1 gene promoter occurs in the non-cancerous mucosa which varies significantly among individuals and may lead to the development of MSI-H gastric cancer. Such methylation in non-cancerous mucosa may also increase the risk of subsequent neoplasia.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Aaltonen LA, Peltomaki P, Leach FS, Sistonen P, Pylkkanen L, Mecklin JP, Jarvinen H, Powell SM, Jen J, Hamilton SR, Petersen GM, Kinzler KW, Vogelstein B, de la Chapelle A (1993) Clues to the pathogenesis of familial colorectal cancer. Science 260: 812–816
Ahuja N, Mohan AL, Li Q, Stolker JM, Herman JG, Hamilton SR, Baylin SB, Issa JP (1997) Association between CpG island methylation and microsatellite instability in colorectal cancer. Cancer Res 57: 3370–3374
Ahuja N, Li Q, Mohan AL, Baylin SB, Issa JP (1998) Aging and DNA methylation in colorectal mucosa and cancer. Cancer Res 58: 5489–5494
Baylin SB, Herman JG, Graff JR, Vertino PM, Issa JP (1998) Alterations in DNA methylation: a fundamental aspect of neoplasia. Adv Cancer Res 72: 141–196
Chong JM, Fukayama M, Hayashi Y, Takizawa T, Koike M, Konishi M, Kikuchi-Yanoshita R, Miyaki M (1994) Microsatellite instability in the progression of gastric carcinoma. Cancer Res 54: 4595–4597
Deng G, Chen A, Hong J, Chae HS, Kim YS (1999) Methylation of CpG in a small region of the hMLM1 promoter invariably correlates with the absence of gene expression. Cancer Res 59: 2029–2033
dos Santos NR, Seruca R, Constancia M, Seixas M, Sobrinho-Simoes M (1996) Microsatellite instability at multiple loci in gastric carcinoma: clinicopathologic implications and prognosis. Gastroenterology 110: 38–44
Esaki Y, Hirokawa K, Yamashiro M (1987) Multiple gastric cancers in the aged with special reference to intramucosal cancers. Cancer 59: 560–565
Fleisher AS, Esteller M, Wang S, Tamura G, Suzuki H, Yin J, Zou TT, Abraham JM, Kong D, Smolinski KN, Shi YQ, Rhyu MG, Powell SM, James SP, Wilson KT, Herman JG, Meltzer SJ (1999) Hypermethylation of the hMLH1 gene promoter in human gastric cancers with microsatellite instability. Cancer Res 59: 1090–1095
Fleisher AS, Esteller M, Tamura G, Rashid A, Stine OC, Yin J, Zou TT, Abraham JM, Kong D, Nishizuka S, James SP, Wilson KT, Herman JG, Meltzer SJ (2001) Hypermethylation of the hMLH1 gene promoter is associated with microsatellite instability in early human gastric neoplasia. Oncogene 20: 329–335
Goelz SE, Hamilton SR, Vogelstein B (1985) Purification of DNA from formaldehyde fixed and paraffin embedded human tissue. Biochem Biophys Res Commun 130: 118–126
Graff JR, Herman JG, Myohanen S, Baylin SB, Vertino PM (1997) Mapping patterns of CpG island methylation in normal and neoplastic cells implicates both upstream and downstream regions in de novo methylation. J Biol Chem 272: 22322–22329
Guo RJ, Arai H, Kitayama Y, Igarashi H, Hemmi H, Arai T, Hanai H, Sugimura H (2001) Microsatellite instability of papillary subtype of human gastric adenocarcinoma and hMLH1 promoter hypermethylation in the surrounding mucosa. Pathol Int 51: 240–247
Halling KC, Harper J, Moskaluk CA, Thibodeau SN, Petroni GR, Yustein AS, Tosi P, Minacci C, Roviello F, Piva P, Hamilton SR, Jackson CE, Powell SM (1999) Origin of microsatellite instability in gastric cancer. Am J Pathol 155: 205–211
Herman JG, Merlo A, Mao L, Lapidus RG, Issa JP, Davidson NE, Sidransky D, Baylin SB (1995) Inactivation of the CDKN2/p16/MTS1 gene is frequently associated with aberrant DNA methylation in all common human cancers. Cancer Res 55: 4525–4530
Herman JG, Umar A, Polyak K, Graff JR, Ahuja N, Issa JP, Markowitz S, Willson JK, Hamilton SR, Kinzler KW, Kane MF, Kolodner RD, Vogelstein B, Kunkel TA, Baylin SB (1998) Incidence and functional consequences of hMLH1 promoter hypermethylation in colorectal carcinoma. Proc Natl Acad Sci USA 95: 6870–6875
Ionov Y, Peinado MA, Malkhosyan S, Shibata D, Perucho M (1993) Ubiquitous somatic mutations in simple repeated sequences reveal a new mechanism for colonic carcinogenesis. Nature 363: 558–561
Issa JP (2000) CpG-island methylation in aging and cancer. Curr Top Microbiol Immunol 249: 101–118
Jones PA, Laird PW (1999) Cancer epigenetics comes of age. Nat Genet 21: 163–167
Kane MF, Loda M, Gaida GM, Lipman J, Mishra R, Goldman H, Jessup JM, Kolodner R (1997) Methylation of the hMLH1 promoter correlates with lack of expression of hMLH1 in sporadic colon tumors and mismatch repair-defective human tumor cell lines. Cancer Res 57: 808–811
Kang GH, Shim YH, Ro JY (1999) Correlation of methylation of the hMLH1 promoter with lack of expression of hMLH1 in sporadic gastric carcinomas with replication error. Lab Invest 79: 903–909
Kuismanen SA, Holmberg MT, Salovaara R, Schweizer P, Aaltonen LA, de La Chapelle A, Nystrom-Lahti M, Peltomaki P (1999) Epigenetic phenotypes distinguish microsatellite-stable and -unstable colorectal cancers. Proc Natl Acad Sci USA 96: 12661–12666
Leung SY, Yuen ST, Chung LP, Chu KM, Chan AS, Ho JC (1999) hMLH1 promoter methylation and lack of hMLH1 expression in sporadic gastric carcinomas with high-frequency microsatellite instability. Cancer Res 59: 159–164
Leung WK, Yu J, Ng EKW, To KF, Ma PK, Lee TL, Go MYY, Chung SCS, Sung JJY (2001) Concurrent hypermethylation of multiple tumor-related genes in gastric carcinoma and adjacent normal tissues. Cancer 91: 2294–2301
Lipkin M (1988) Biomarkers of increased susceptibility to gastrointestinal cancer: new application to studies of cancer prevention in human subjects. Cancer Res 48: 235–245
Mironov NM, Aguelon MA, Potapova GI, Omori Y, Gorbunov OV, Klimenkov AA, Yamasaki H (1994) Alterations of (CA)n DNA repeats and tumor suppressor genes in human gastric cancer. Cancer Res 54: 41–44
Nakagawa H, Chadwick RB, Peltomaki P, Plass C, Nakamura Y, de la Chapelle A (2001) Loss of imprinting of the insulin-like growth factor II gene occurs by biallelic methylation in a core region of H19-associated CTCF-binding sites in colorectal cancer. Proc Natl Acad Sci USA 98: 591–596
Nakashima H, Inoue H, Mori M, Ueo H, Ikeda M, Akiyoshi T (1995) Microsatellite instability in Japanese gastric cancer. Cancer 75: 1503–1507
Ogata S, Tamura G, Endoh Y, Sakata K, Ohmura K, Motoyama T (2001) Microsatellite alterations and target gene mutations in the early stages of multiple gastric cancer development. J Pathol 194: 334–340
Ohmura K, Tamura G, Endoh Y, Sakata K, Takahashi T, Motoyama T (2000) Microsatellite alterations in differentiated-type adenocarcinomas and precancerous lesions of the stomach with special reference to cellular phenotype. Hum Pathol 31: 1031–1035
Strickler JG, Zheng J, Shu Q, Burgart LJ, Alberts SR, Shibata D (1994) p53 mutations and microsatellite instability in sporadic gastric cancer: when guardians fail. Cancer Res 54: 4750–4755
Suzuki H, Itoh F, Toyota M, Kikuchi T, Kakiuchi H, Hinoda Y, Imai K (1999) Distinct methylation pattern and microsatellite instability in sporadic gastric cancer. Int J Cancer 83: 309–313
Tamura G, Sakata K, Nishizuka S, Maesawa C, Suzuki Y, Terashima M, Eda Y, Satodate R (1996) Allelotype of adenoma and differentiated adenocarcinoma of the stomach. J Pathol 180: 371–377
Tamura G, Yin J, Wang S, Fleisher AS, Zou T, Abraham JM, Kong D, Smolinski KN, Wilson KT, James SP, Silverberg SG, Nishizuka S, Terashima M, Motoyama T, Meltzer SJ (2000) E-Cadherin gene promoter hypermethylation in primary human gastric carcinomas. J Natl Cancer Inst 92: 569–573
Thibodeau SN, French AJ, Roche PC, Cunningham JM, Tester DJ, Lindor NM, Moslein G, Baker SM, Liskay RM, Burgart LJ, Honchel R, Halling KC (1996) Altered expression of hMSH2 and hMLH1 in tumors with microsatellite instability and genetic alterations in mismatch repair genes. Cancer Res 56: 4836–4840
Toyota M, Ahuja N, Ohe-Toyota M, Herman JG, Baylin SB, Issa JP (1999a) CpG island methylator phenotype in colorectal cancer. Proc Natl Acad Sci USA 96: 8681–8686
Toyota M, Ahuja N, Suzuki H, Itoh F, Ohe-Toyota M, Imai K, Baylin SB, Issa JP (1999b) Aberrant methylation in gastric cancer associated with the CpG island methylator phenotype. Cancer Res 59: 5438–5442
Tsuchiya T, Tamura G, Sato K, Endoh Y, Sakata K, Jin Z, Motoyama T, Usuba O, Kimura W, Nishizuka S, Wilson KT, James SP, Yin J, Fleisher AS, Zou T, Silverberg SG, Kong D, Meltzer SJ (2000) Distinct methylation patterns of two APC gene promoters in normal and cancerous gastric epithelia. Oncogene 19: 3642–3646
Yamashita K, Arimura Y, Kurokawa S, Itoh F, Endo T, Hirata K, Imamura A, Kondo M, Sato T, Imai K (2000) Microsatellite instability in patients with multiple primary cancers of the gastrointestinal tract. Gut 46: 790–794
Veigl ML, Kasturi L, Olechnowicz J, Ma AH, Lutterbaugh JD, Periyasamy S, Li GM, Drummond J, Modrich PL, Sedwick WD, Markowitz SD (1998) Biallelic inactivation of hMLH1 by epigenetic gene silencing, a novel mechanism causing human MSI cancers. Proc Natl Acad Sci USA 95: 8698–8702
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Sakata, K., Tamura, G., Endoh, Y. et al. Hypermethylation of the hMLH1 gene promoter in solitary and multiple gastric cancers with microsatellite instability. Br J Cancer 86, 564–567 (2002). https://doi.org/10.1038/sj.bjc.6600076
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6600076
Keywords
This article is cited by
-
Increased incidence of metachronous gastric neoplasm after endoscopic resection in patients with synchronous gastric neoplasm
BMC Gastroenterology (2020)
-
Clinicopathologic and Immunohistochemistry Characterization of Synchronous Multiple Primary Gastric Adenocarcinoma
Journal of Gastrointestinal Surgery (2007)
-
Stage IV early gastric cancer: two cases with microsatellite instability
Langenbeck's Archives of Surgery (2007)
-
Aberrant promoter methylation in human DAB2 interactive protein (hDAB2IP) gene in gastrointestinal tumour
British Journal of Cancer (2005)
-
Hypermethylation of Chfr and hMLH1 in gastric noninvasive and early invasive neoplasias
Virchows Archiv (2005)