Abstract
Data sources
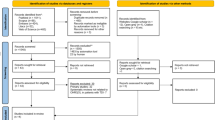
Cochrane Library, Embase, PubMed, Scopus, Web of Science, LILACS/BBO, PsycINFO, ClinicalTrials, ISRCTN registry, UK National Institute for Health and Care Excellence, International Clinical Trials Registry Platform, ProQuest and OpenGrey.
Study selection
Two independent and calibrated reviewers selected randomised controlled trials investigating cognitive behavioural therapy use in dentally anxious children.
Data extraction and synthesis
Risk of bias was assessed by two independent reviewers according to the Cochrane Collaboration tool. Clinical and methodological heterogeneity were assessed to determine whether a meta-analysis could be performed but the data were not similar enough and therefore a narrative synthesis is provided.
Results
Six studies were included, all written in English between 1980 and 2017. Two were completed in the United States, one in Jamaica, one in Iran, one in Sweden and one in Norway and included 269 patients in total ranging from 41 months to 18 years. Two studies had high risk of bias. In five studies, CBT patients showed significantly reduced levels of anxiety. In three studies improvement was observed in cooperation/behaviour. In two studies, avoidance behaviours improved.
Conclusions
CBT has been shown in published literature to have a positive effect on childrens anxiety and co-operation; however the quality of evidence for this is low. There is no current consensus on which outcome measure/s should be used, which prevents meta-analysis of results. Further randomised controlled studies are required, ideally using the same outcome measures, to develop evidence based guidance on the use of CBT in dentally anxious children.
Similar content being viewed by others
Commentary
Dental anxiety is common among children and adolescents, affecting over 50% of 12- to 15-year olds in the United Kingdom.1 It is therefore essential that dental practitioners have an awareness of the psychological interventions that are available for these patients. Cognitive Behavioural Therapy (CBT) is a type of therapy used to help patients manage their own problems, in this case their dental anxiety, by changing the negative way they think and behave.2 CBT is widely used within medicine (particularly in the field of mental health) and a recent Cochrane review by James and colleagues showed it to be effective in managing anxiety disorders in children and adolescents.3 The aim of this current review was to assess the latest evidence on the effectiveness of CBT in reducing dental anxiety in children.
An extensive literature search was conducted, with no restriction on publication date or language. This should have ensured all relevant publications were identified, however only randomised controlled trials (RCTs) were included. The risk of bias was assessed independently using the Cochrane Collaborations Tool for Assessing Bias in Randomised Trials. Two studies were determined to be at high risk of performance bias (blinding). The small sample sizes and generally short data collection periods suggest that the overall quality of evidence for the use of CBT to reduce dental anxiety in children is currently low. In order to improve the evidence base, the authors recommended that future studies should assess the long-term effects of CBT on dental anxiety, and for these studies to use consistent outcomes and outcome measures. This would enable comparison and combination of the results of different studies and make meta-analysis possible.
The evidence base for the use of CBT for children with dental anxiety continues to grow, and there are many different formats in which it can be applied, with increasing use of digital technology – guided self-help,4 dental professional-led or psychologist-led, depending on the severity of the anxiety. Indeed, studies by Rodd and colleagues5 and Shahnavaz and colleagues6 published since this review suggest that the reduction in dental anxiety following CBT can be maintained over time. The review alludes to the likely cost effectiveness of using CBT, and it can be theorised that the initial cost of providing the therapy may be offset by preventing a child from developing into a dentally anxious adult who is reliant on pharmacological approaches for dental treatment. This is not yet proven, but should be investigated in future studies.
References
Health and Social Care Information Centre. Children's Dental Health Survey 2013. London: Health and Social Care Information Centre, 2015.
Cognitive behavioural therapy (CBT) 2018 Available at www.nhs.uk/conditions/cognitive-behavioural-therapy-cbt/ (accessed October 2018).
James AC, James G, Cowdrey FA, Soler A, Choke A . Cognitive behavioural therapy for anxiety disorders in children and adolescents. Cochrane Database Syst Rev 2015; 2: CD004690.
Porritt J, Rodd H, Morgan A, et al. Development and testing of a Cognitive Behavioral Therapy resource for children's dental anxiety. JDR Clin Trans Res 2017; 2: 23–37.
Rodd H, Kirby J, Duffy E, et al. Children's experiences following a CBT intervention to reduce dental anxiety: one year on. Br Dent J 2018; 225: 247–251.
Shahnavaz S, Hedman-Lagerlöf E, Hasselblad T, Reuterskiöld L, Kaldo V, Dahllöf G . Internet-Based Cognitive Behavioral Therapy for children and adolescents with dental anxiety: Open Trial. J Med Internet Res 2018; 20: e12.
Author information
Authors and Affiliations
Additional information
Address for correspondence: Professor Luciane Rezende Costa, Faculdade de Odontologia, Universidade Federal de Goiás, Av. Universitária Esquina com 1a Avenida s/n, Setor Universitário CEP: 74605-220 – Goiânia, Goiás, Brazil. E-mail: lucianecostaufg@gmail.com
Gomes HS, Viana KA, Batista AC, Costa LR, Hosey MT, Newton T. Cognitive behaviour therapy for anxious paediatric dental patients: a systematic review. Int J Paediatr Dent 2018; doi: 10.1111/ipd.12405. [Epub ahead of print] PubMed PMID: 29984460.
Rights and permissions
About this article
Cite this article
Noble, F., Marshman, Z. The effectiveness of Cognitive Behavioural Therapy in the reduction of dental anxiety in children. Evid Based Dent 19, 104 (2018). https://doi.org/10.1038/sj.ebd.6401339
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ebd.6401339