Abstract
Data sources
PubMed, Scopus, Web of Science, Virtual Health Library (VHL), Cochrane Library, Clinical Trials and OpenGrey.
Study selection
Randomised controlled trials comparing the clinical effectiveness of Class II restorations performed with conventional (C-GIC) or resin-modified glass ionomer cement (RM-GIC) and composite resin (CR) in primary molar teeth. No date of publication or language restrictions.
Data extraction and synthesis
Study selection was carried out independently by two reviewers, with abstracted data and risk of bias assessment being performed using the Cochrane tool. Data on the restorations were dichotomised as acceptable' (restorations without need of replacement or repair) or ‘unacceptable’ (restorations presenting failures or requiring repair or replacement) after which a number of meta-analyses were conducted.
Results
Ten studies were included in qualitative synthesis, and nine contributing to the meta-analyses. Six studies used a split-mouth design and four a parallel design. Seven studies used USPHS criteria, two applied the FDI criteria and one used their own. Seven studies reported restorations were placed under rubber dam isolation with the other three using cotton roll isolation. Six studies were at low risk of bias and four unclear risk of bias. GIC and CR presented similar failure patterns (Risk Difference [RD] = -0.04 (95%CI; -0.11 to 0.03) p=0.25, I2 = 51%), irrespective of follow-up period, type of GIC used, method of isolation or criteria used for assessment. GICs exhibited significantly lower values of secondary carious lesions ([RD] = 0.06 (95%CI; 0.0 to 0.10), p=0.008, I2 = 0%).
Conclusions
GICs and CRs have comparable clinical performance in Class II restorations in primary molars. GICs did show superior performance in the occurrence of secondary carious lesions, especially when RM-GIC under rubber dam isolation was used.
Similar content being viewed by others
Commentary
Dental caries remains a prevalent disease in the primary dentition with 25%1 of five year olds experiencing tooth decay, leading to problems such as sleepless nights, missed days from school and reduced social interactions with peers.2
Amalgam has good longevity,3 however its use has declined over the past decade due to concerns over toxicity relating to potential mercury release.4 This brought about a recent change in EU regulations (European Union Regulations 2017/852) which state that as of 1st July 2018, dental amalgam shall not be used for the dental treatment of primary teeth. This change is likely to have a significant impact in the provision of dental care across the UK and Europe. In light of these concerns, this systematic review and meta-analyses looked to address the clinical performance of glass ionomer cements (both conventional and resin modified) when compared to composite resins for the restoration of Class II carious lesions in primary molar teeth.
A robust and thorough search strategy was adopted for this systematic review. An electronic database search of PubMed, Scopus, Web of Science, Virtual Health Library (VHL), Clinical Trials and Cochrane Library was carried out with specific search strategies for each database presented as a table in the paper. The authors made a conscious effort to find unpublished data by including ongoing studies from clinicaltrials.gov as well as including grey literature using the OpenGrey database. Hand searching of specific dental journals or the reference lists of included studies was not carried out. Strict inclusion/exclusion criteria are provided having been derived by using the PICOS approach. Only randomised control trials, where Class II cavities were restored with GIC (conventional or resin-modified) compared to composite resin, were included. There were no restrictions on the date or the language of publication.
The primary outcome of percentage failure of the restorations is clearly defined and is appropriate for the research question. Further outcome measures (secondary carious lesions, marginal discolouration, marginal adaptation, longevity, retention/wear of restorative material, and the anatomical form) to help provide reasons for failure were provided. The type of GIC used and isolation technique used were collected to address the secondary outcomes of the review.
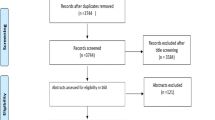
Data extraction was independently done by two reviewers and followed the recognised PRISMA approach. A flowchart provides the reader with a level detail regarding the number of studies identified, that were eligible and included in the review. Reasons for exclusion of eligible studies are given. Methodological quality and risk of bias were assessed by the same reviewers, using the Cochrane tool for analysis of risk of bias. Interestingly, the authors deviate from Cochrane by excluding blinding procedures within each study. They report that studies are considered as ‘low-risk’ of bias if there was adequate randomisation and allocation concealment as well as no incomplete data and selective reporting. The authors provide a rationale as to why they have adopted this approach suggesting that the differences in operative technique and clinical aspects of the materials are so distinct that blinding would not influence results. However, you could argue that blinding study evaluators at follow-up would be essential to include in an overall bias as if the evaluators were aware of the treatments, then this would have an overall impact. A third reviewer was used to resolve any disagreements throughout the process that were not resolved by discussion between the reviewers.
After removing duplicates, 2937 studies were screened for eligibility. Twenty-five full-texts were assessed with ten studies included for qualitative synthesis and nine for meta-analyses. Overall risk of bias was reported with six studies being of ‘low risk’ of bias and four of ‘unclear’ risk of bias. Six studies used a split-mouth design and four used a parallel design with length of follow-up varying between studies with a range of six to 48 months. The majority of studies had a length of follow-up far longer than six months, which is important when assessing longevity and failure rate of restorative materials. Variation in the number of children and restorations per study was reported with an overall age range of children treated being three to 11. Including children aged ten and over in some of these studies is surprising as you may expect the primary molars would have been close to exfoliation by this point. Further breakdown by age may have been interesting to help adjust for this potential confounder.
Criteria to evaluate clinical parameters varied between studies, however of note, only two studies used radiographic examination to assess failures, which is surprising as several national guidelines would advocate their use to assess restoration success. The authors explicitly report they dichotomised data from the nine studies that reported the main parameters (failure, marginal adaptation and discolouration, anatomical form and secondary caries) as ‘acceptable’ and ‘not acceptable’ to allow for meta-analyses. Prevalence of unacceptable events and the total number of restorations were used to calculate the risk difference at a confidence interval of 95%. A random effects model was applied and heterogeneity was evaluated using the I2 index.
The pooled effect of failure of GIC compared to CR was not statistically significant, as shown by a forest plot, with a risk difference (RD) of -0.04(95%CI: -0.11 to 0.03; p = 0.25, I2 = 51%) being reported. Further meta-analyses were undertaken and the results were reported in both a table and forest plots. The statistically significant findings found from the meta-analyses reported less secondary caries of GICs compared to CR in all studies (p = 0.008), when followed-up for >24 months (p = 0.02), when RM-GICs were used (p = 0.008), and placed under rubber-dam (p = 0.02). GICs were less likely to fail, overall, when placed under rubber dam (p = 0.03) and compared to CR.
This systematic review and meta-analyses appear to highlight the potential benefits of using less technique sensitive restorative materials such as C-GIC and RM-GIC for restoration of primary molars with success comparable to composite resins. Chisini et al.5 similarly reported RM-GIC superiority over composite resins (93.6%5 vs 79.3%5 success rates over four years).5 Preformed metal crowns (PFMCs) however showed an even higher success rate of 96.1%5 when compared to any direct restorative material used in primary molars.5 These findings concur with the Cochrane Review carried out by Innes et al.6 who concluded that primary molars restored with PFMCs are less likely to develop problems or cause pain in the long term, compared to fillings.6 Due to the range of patient factors that can affect restorative success (for example isolation, access, cooperation) the evidence would suggest that neither GICs nor CRs outperform PFMCs for Class II cavities in primary molars.
Practice point
-
Glass ionomer cements (resin-modified and conventional) and composite resins are comparable materials for restoring Class II cavities in primary molars, however, neither outperform pre-formed metal crowns.
-
Resin modified GICs placed under rubber dam have less secondary caries risk when compared to composite resin restorations in Class II cavities in primary molars.
References
Public Health England. Health matters: Child Dental Health 2017. London. Available at https://www.gov.uk/government/publications/health-matters-child-dental-health/health-matters-child-dental-health (accessed July 2018).
Sheiham A . Oral health, general health and quality of life. Bull World Health Organ 2005; 83: 644.
Wong YJ . Low-quality evidence suggests that amalgam has increased longevity compared with resin-based composite in posterior restorations. J Am Dent Assoc 2016; 147:905–906.
Weldon JC, Yengopal V, Siegfried N, Gostemeyer G, Schwendicke F, Worthington HV . Dental filling materials for managing carious lesions in the primary dentition. Cochrane Database Syst Rev 2016; 10. Art. No. CD004483. DOI: 10.1002/14651858.CD004483.pub3
Chisini LA, Collares K, Cademartori MG, et al. Restorations in primary teeth: a systematic review on survival and reasons for failures. Int J Paediatr Dent 2018; 28:123–139.
Innes NP, Ricketts D, Chong LY, Keightley AJ, Lamont T, Santamaria RM . Preformed crowns for decayed primary molar teeth. Cochrane Database Syst Rev 2015; 12: Art. No. CD005512.
Author information
Authors and Affiliations
Additional information
Address for correspondence: Sao Paulo State University (Unsep), School of Dentistry, Aracatuba, Department of Paediatric Dentistry and Public Health, Rua Jose Bonifacio, 1193, 16015-050 Aracatuba, SP, Brazil. E-mail: jpessan@foa.unesp.br
Dias AGA, Magno MB, Delbem ACB, Cunha RF, Maia LC, Pessan JP. Clinical performance of glass ionomer cement and composite resin in Class II restorations in primary teeth: A systematic review and meta-analysis. J Dent 2018; 73: 1–13. pii:S0300-5712(18)30073-3. doi:10.1016/j.jdent.2018.04.004. [Epub ahead of print] Review. PubMed PMID: 29649506.
Rights and permissions
About this article
Cite this article
Jones, G., Taylor, G. Glass ionomer or composite resin for primary molars. Evid Based Dent 19, 86–87 (2018). https://doi.org/10.1038/sj.ebd.6401328
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ebd.6401328