Abstract
Hypospadias, one of the most common congenital abnormalities of the male external genitalia with elusive etiology, are caused by a defect in the normal development of the urethra, foreskin and ventral aspect of the penis. Evidences indicate that BMP4 and BMP7, two of those major factors in a signaling cascade involved in controlling the embryonic urethral development, play central roles in the normal development of the urethra, and that HOXA4 and HOXB6 play important roles in the development of skin in various tissues at the time course of the urethral development. We directly sequenced all these exons and exon–intron boundaries of the four genes in 90 unrelated Chinese patients with hypospadias. Thirteen different heterozygous nucleotide variations were identified for the first time in the four genes in 14 of 90 cases. Of the 13 variations, eight are missense: c.619C>G (p.H207D), c.668G>A (p.R223H), c.751C>T (p.H251Y) in BMP4; c.907C>T (p.R303C) in BMP7; c.385G>T (p.G129C), c.869C>G (p.S290C) in HOXA4; c.124C>A (p.P42T), c.367T>C (p.C123R) in HOXB6. None of these variations were found in 380 control chromosomes. Amino-acid sequence alignments showed most of these changed amino acids are conserved across various vertebrate species. In a word, these findings, together with the indicated roles of the four genes, imply that it should not be random events for so many nucleotide variations found in the present study. Further functional studies are required to make the associations clear between these variants and hypospadias.
Similar content being viewed by others
Introduction
Hypospadias (MIM# 146450) is one of the most common congenital anomalies occurring in 1 out of 300 to 1 out of 125 infant males in different ethnic populations.1, 2 It can be defined as a defect in the normal development of the urethra, foreskin and ventral aspect of the penis, and may be classified as simple (glandular or penile) and severe (scrotal or perineal) on the basis of the anatomical location of the urethral meatus. The cause of hypospadias is complex, and still elusive to date, especially in mild cases. Hypospadias is probably a complex disorder caused by both genetic and environmental influences, either alone or in a combination.2, 3
Because the formation of the male urethra is fully androgen-dependent, it seems that a more reasonable theory to explain hypospadias is an abnormality in the pathway of the androgen metabolism. Indeed, those defects in some molecules involved in the pathway, like SRY, SOX9, AR, SRD5A2 and WT1, might contribute to the abnormal male development including a subset of hypospadias.2 The modes of inheritance of hypospadias might vary. For example, the inheritance of AR defects, is X-linked recessive, and SRD5A2 defects autosomal recessive.4, 5 However, all these defects only account for no more than 30% of cases.6 Thus, the fact that the causes have not yet been identified for a large number of cases highlights the importance of seeking other possible genetic explanations for the congenital defect.
Knowledge about molecular mechanisms of the normal formation of the male urethra, including the glandular urethra might help to elucidate the etiology of hypospadias. To a great extent, the development of the male urethra is similar to those of palate and limbs. During the formation of these organs, tissue phenotypic transformations always occur. The classic mechanism of the phenotypic transformation is an epithelial-to-mesenchymal cell change or a mesenchymal-to-epithelial transformation. The transformation involves a signaling cascade composed of Hedgehog, TGFβ signaling pathway as well as HOX molecules and so on. These molecules always act as the mediators of morphogenetic cell–cell interactions.3, 7, 8 This signaling cascade is conserved throughout organisms from Drosophila to humans and in many tissues, including skeleton, limb, lung, gut and genitalia. Among these signaling molecules of the cascade, SHH, HOXA13, BMP4, BMP7, FGF8 FGF10 and so on are major ones.7, 9 Studies in mice have already shown that defects or loss of functions of these molecules could result in an altered genital phenotype including hypospadias, either alone or in a combination.7, 8, 9, 10, 11
As mentioned above, the development of the penile shaft skin and the preputial skin is also fundamental stages in the formation of the male urethra. Any disturbance in these stages may also cause hypospadias.1, 12 Although no direct evidence in the urogenital system, experimental evidences have suggested that HOXB6 (former Hox2.2) and HOXA4 play important roles in the development of skin of various tissues at week 10–17 of gestation, and that the time course of the development of the penile shaft skin and the preputial skin is just at week 10–17 of gestation.13, 14 In addition, mice and chicken models also show that HOXB6 gene products are involved in controlling pattern formation in developing limbs.15, 16
Based on the above knowledge, we hypothesized that mutations in SHH, HOXA13, BMP4, BMP7, FGF8 and FGF10 genes might result in an altered genital phenotype including hypospadias. However, there have already been evidences excluding HOXA13 and some of the FGFs as candidate genes for isolated hypospadias.6, 8 In the present study, we attempt to investigate whether there are some nucleotide alternations in BMP4 and BMP7, two downstream molecules of the above signaling cascade, and in HOXA4, HOXB6 in hypospadias.
Materials and methods
Patients and controls
Ninety sporadic Chinese patients enrolled in our experiments were identified in the Hypospadias Treating Center of the Plastic Surgery Hospital, PUMC. All patients included were 46,XY. Clinical phenotypes, family histories and complications of the 90 patients were shown in previous report. Some known candidate genes for hypospadias such as SRD5A2, WT1 and AR have already been studied in the 90 patients and some of these patients parents.4 A total of 190 Chinese normal males with no history of any abnormalities in urogenitory system, limbs and palate, were recruited as a control group. The mean age of the control group was 27 years.4 Informed consent was obtained from all patients or their parents. Ethical approval for the study was obtained from the Ethical Committee of the National Center of Human Genome Research, Beijing.
Mutation detections and analysis
Polymerase chain reaction (PCR) amplification. Genomic DNAs were extracted from the peripheral leukocytes of the cases and controls using standard procedures. The sequences of Bmp4, Bmp7, HoxA4 and HoxB6 genes were obtained from http://www.ncbi.nlm.nih.gov or http://www.genome.ucsc.edu. PCR was employed to amplify all these exons and exon–intron boundaries of the four genes with primers designed using Premier 5.0 software. To facilitate their subsequent sequencing, some exons were divided to make PCR products less than 500–600 bp in length generally. PCR was performed in a 50 μl volume and thermal cycling was performed in a GeneAmp PCR System 2700 (Perkin-Elmer, Applied Biosystems, Foster City, CA, USA) (detailed PCR conditions and sequences of primer sets are available upon request).
Sequencing and sequence analysis. PCR products were purified using a MultiScreen-PCR plate (Millipore Corporation, Bedford, USA). Sequencing was completed bi-directionally on an ABI 3730XL DNA analyzer (Applied Biosystems) using the amplification primers described above. When finding some nucleotide variations in some fragments of the cases, we also analyzed the corresponding fragments in controls using the same methods used in the cases. Sequence data were analyzed against respective reference sequence from NCBI or UCSC database (BMP4: NM_130851; BMP7: NM_001719; HOXA4: NM_002141; HOXB6: NM_156037) and compared to the normal controls using the Phred/Phrap/Consed software (University of Washington, Seattle, USA). All nucleotide changes were confirmed by repeating the PCR and sequencing reactions.
Multiple amino-acid sequence alignments of the four human genes with respective vertebrate orthologs were done with online ClustalW program (http://www.ebi.ac.uk/clustalw/).
Results
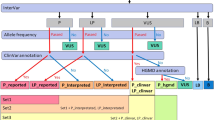
In the study, we found 13 different heterozygous nucleotide sequence variations, including three in BMP4, six in BMP7, two in HOXA4 and two in HOXB6, in all these exons and exon–intron boundaries of the four genes in 14 of the 90 patients. Of these variations, eight (c.619C>G, c.668G>A, c.751C>T; c.907C>T; c.385G>T, c.869C>G; c.124C>A, c.367T>C) are missense variations. The other five variations, c.597G>A, c.1465T>A (3′UTR), c.1567A>G (3′UTR), c.612-33C>T, c.1146+39C>T are silent because c.597G>A does not cause amino-acid change, whereas, c.1465T>A, c.1567A>G are located in the 3′UTR, and c.612-33C>T, c.1146+39C>T are in introns (Table 1, Figure 1).
Linear diagrams showing exons (all boxes) and introns of BMP4, BMP7, HOXA4 and HOXB6 genes (accession number NM_130851, NM_001719, NM_002141, NM_156037, respectively), and the variation chromatograms of the four genes. All the coding regions are highlighted light green. Some important domains are shown by different boxes, which are explained below each of the linear diagrams. All the variations in the study are indicated by a black arrow above the linear diagrams and by a red arrow above the sequence chromatograms, respectively. Figures are drawn roughly to scale.
None of these variations found in the study were found in 380 control chromosomes. Amino-acid sequence alignments of the four human genes with respective vertebrate orthologs available from NCBI show that p.H207, p.R223 and p.H251 in BMP4; p.Q199 and p.R303 in BMP7 are highly conserved across all their respective vertebrate orthologs available from NCBI database. p.G129 and p.S290 in HOXA4, p.P42 and p.C123 in HOXB6 are partly conserved across all their respective vertebrate orthologs available from NCBI database (Figure 2).
Amino-acid sequence alignments of BMP4, BMP7, HOXA4 and HOXB6 from respective vertebrate species. The changed residues are highlighted light gray and indicated by an asterisk (*). Amino-acid numbers are shown at the left of each of the selected regions. ‘-//-’ represents those residues omitted in every line, ‘…’ denotes that no corresponding residues were published in the NCBI protein databases.
Discussion
Insights into possible important roles of some molecules of HOX and BMP families in urogenital and limb development provoked our investigation involvement of BMP4, BMP7, HOXA4 and HOXB6 genes in patients with hypo-spadias. To our knowledge, the genetic alterations of the four genes have not been previously described in humans.
In this study, we found a comparatively large amount of nucleotide variations (16%) in the four genes in our 90 patients. None of these variations were found in 380 control chromosomes. Eight missense variations appeared highly or partly conserved across all their respective vertebrate orthologs available from NCBI database. In addition, some animal models have already indicated that the four molecules are involved in the normal male urethral formation, or showed that the loss or defects of functions of these molecules could cause an altered genital phenotype including hypospadias elsewhere.1, 7, 11, 12, 13, 14, 15, 16 Summing up these aspects, we believe it is possible that these variants, especially these eight missense ones, are associated with their phenotypes. However, those five silent variations are unlikely to have a major impact on their phenotypes. Of course, further functional studies are required to identify these possible associations in the future.
In addition, among the 14 patients, three also carry some variations located outside the BMP4, BMP7, HOXA4 and HOXB6 (Table 1 and 2). Patient 16 carries the hemizygous p.A620V in MID1 (unpublished data), the heterozygous Q6X and G203S mutations in SRD5A2.4 Family studies found that, in the patient, the hemizygous p.A620V in MID1 is de novo. In addition, family studies also found that his mother, the carrier of the heterozygous p.P42T in HOXB6 and the heterozygous G203S in SRD5A2, and his father, the carrier of the heterozygous Q6X in SRD5A2, were all healthy.4 It is known that the G203S is pathogenic in patient 16.4 Because the defects in MID1 is X-linked inheritance, we speculate p.A620V in MID1 is also possibly pathogenic. If so, both G203S in SRD5A2 and p.A620V in MID1 might contribute to his phenotype. And the severity of patient 16 is due to the combined contribution of multi-mutations. But, owing to the unknown mode of inheritance of HOXB6 mutation in hypospadias and lack of functional data, we now cannot determine whether the p.P42T in HOXB6 also contributes to his phenotype. Patient 73 carries a known pathogenic homozygous mutation, R227Q in SRD5A2. Patient 65 carries a synonymous S159S mutation in WT1.4 Similarly, we also wonder if the p.S290C of HOXA4 and p.R303C of BMP7 in the present study have an effect on the phenotypes of patient 73 and 65, respectively. Likewise, these questions are also required for further functional identifications.
Also, based on the above idea of the combined effect, our samples in the present study are the same as those of our previous study, although some of the 90 patients have already got positive results in other known genes.
In conclusion, we have found 13 nucleotide sequence variations in 14 of 90 patients (16%) in the BMP4, BMP7, HOXA4 and HOXB6 genes. Among these nucleotide variations, eight are missense, and five are silent. Based their conservation data, the absences of all these variants in normal controls, and the roles of the four gene products in the formation of the male urethra indicated by other groups, we suggest that these variants in the present study are not random events in hypospadias, especially for the eight missense variations. However, further functional studies are required to make the associations clear between these variants and hypospadias. Our current work is a start in seeking the causes for hypospadias from development-related pathways. Future functional studies should include the assessment of the specific DNA-binding abilities for these HOXA4 and HOXB6 variants, and of the specific receptor-binding abilities for these BMP4 and BMP7 variants, or even the studies of all these variants by the transgenic animal models.
References
Kurzrock EA, Baskin LS, Cunha GR : Ontogeny of the male urethra: theory of endodermal differentiation. Differentiation 1999; 64: 115–122.
Thai HT, Kalbasi M, Lagerstedt K, Frisen L, Kockum I, Nordenskjold A : The Valine allele of the V89L polymorphism in the five-alpha reductase gene confers a reduced risk for hypospadias. J Clin Endocrinol Metab 2005; 90: 6695–6698.
Baskin LS : Hypospadias and urethral development. J Urol 2000; 163: 951–956.
Wang Y, Li Q, Xu J et al: Mutation analysis of five candidate genes in Chinese patients with hypospadias. Eur J Hum Genet 2004; 12: 706–712.
Ferraz LF, Mathias Baptista MT, Maciel-Guerra AT, Junior GG, Hackel C : New frameshift mutation in the 5alpha-reductase type 2 gene in a Brazilian patient with 5alpha-reductase deficiency. Am J Med Genet 1999; 87: 221–225.
Utsch B, Kaya A, Ozburun A, Lentze MJ, Albers N, Ludwig M : Exclusion of WTAP and HOXA13 as candidates genes for isolated hypospadias. Scan J Urol Nephrol 2003; 37: 498–501.
Stadler HS : Modelling genitourinary defects in mice: an emerging genetic and developmental system. Nat Rev Genet 2003; 4: 478–482.
Haraguchi R, Suzuki K, Murakami R et al: Molecular analysis of external genitalia formation: the role of fibroblast growth factor (Fgf) genes during genital tubercle formation. Development 2000; 127: 2471–2479.
Podlasek C, Houston J, McKenna KE, McVary KT : Posterior Hox gene expression in developing genitalia. Evol Dev 2002; 4: 142–163.
Haraguchi R, Mo R, Hui C et al: Unique functions of Sonic hedgehog signaling during external genitalia development. Development 2001; 128: 4241–4250.
Morgan EA, Nguyen SB, Scottv V, Stadler HS : Loss of Bmp7 and Fgf8 signaling in Hoxa13-mutant mice causes hypospadia. Development 2003; 130: 3095–3109.
Baskin LS : Hypospadias. Adv Exp Med Biol 2004; 545: 3–22.
Stelnicki EJ, Komuves LG, Kwong AO et al: HOX homeobox genes exhibit spatial and temporal changes in expression during human skin development. J Invest Dermatol 1998; 110: 110–115.
Komuves LG, Shen WF, Kwong A et al: Changes in HOXB6 homeodomain protein structure and localization during human epidermal development and differentiation. Dev Dyn 2000; 218: 636–647.
Wedden SE, Pang K, Eichele G : Expression pattern of homeobox-containing genes during chick embryogenesis. Development 1989; 105: 639–650.
Schughart K, Bieberich CJ, Eid R, Ruddle FH : A regulatory region from the mouse Hox-2.2 promoter directs gene expression into developing limbs. Development 1991; 112: 807–811.
Acknowledgements
We thank all the patients and their parents for their participation in this study. This work was supported by the National Basic Research Program of China (Grant 2004CB518601) and Clinical Key Program of the Ministry of Health, China (Grant 20010409).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chen, T., Li, Q., Xu, J. et al. Mutation screening of BMP4, BMP7, HOXA4 and HOXB6 genes in Chinese patients with hypospadias. Eur J Hum Genet 15, 23–28 (2007). https://doi.org/10.1038/sj.ejhg.5201722
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ejhg.5201722
Keywords
This article is cited by
-
TGF-β1 relieves epithelial–mesenchymal transition reduction in hypospadias induced by DEHP in rats
Pediatric Research (2020)
-
Next-generation sequencing reveals genetic landscape in 46, XY disorders of sexual development patients with variable phenotypes
Human Genetics (2018)
-
Diagnostic Application of Targeted Next-Generation Sequencing of 80 Genes Associated with Disorders of Sexual Development
Scientific Reports (2017)
-
Sequencing of the DKK1 gene in patients with anorectal malformations and hypospadias
European Journal of Pediatrics (2015)
-
Mutations in 12 known dominant disease-causing genes clarify many congenital anomalies of the kidney and urinary tract
Kidney International (2014)