Abstract
Mitochondrial myopathy in progressive external ophthalmoplegia (PEO) has been associated with POLG1 mutations. POLG1 encodes the catalytic α subunit of polymerase γ and is the only polymerase known to be involved in mtDNA replication. It has two functionally different domains, one polymerase domain and one exonuclease domain with proofreading activity. In this study we have investigated whether mtDNA point mutations are involved, directly or indirectly, in the pathogenesis of PEO. Muscle biopsy specimens from patients with POLG1 mutations, affecting either the exonuclease or the polymerase domain, were investigated. Single cytochrome c oxidase (COX)-deficient muscle fibers were dissected and screened for clonally expanded mtDNA point mutations using a sensitive denaturing gradient gel electrophoresis analysis, in which three different regions of mtDNA, including five different tRNA genes, were investigated. To screen for randomly distributed mtDNA point mutations in muscle, two regions of mtDNA including deletion breakpoints were investigated by high-fidelity PCR, followed by cloning and sequencing. Long-range PCR revealed multiple mtDNA deletions in all the patients but not the controls. No point mutations were identified in single COX-deficient muscle fibers. Cloning and sequencing of muscle homogenate identified randomly distributed point mutations at very low frequency in patients and controls (<1:50 000). We conclude that mtDNA point mutations do not appear to be directly or indirectly involved in the pathogenesis of mitochondrial disease in patients with different POLG1 mutations.
Similar content being viewed by others
Introduction
Whereas single mitochondrial DNA (mtDNA) point mutations are usually maternally inherited and single mtDNA deletions are usually sporadic, a group of disorders with multiple mtDNA deletions display a Mendelian trait of inheritance.1, 2, 3, 4 Mutations in the nuclear gene POLG1 (MIM# 174763), encoding the catalytic subunit of mitochondrial DNA polymerase γ (Pol γ), have been reported in both autosomal dominant (ad) and autosomal recessive (ar) progressive external ophthalmoplegia (PEO) with multiple deletions in mtDNA.1, 5 Pol γ is the only known polymerase for mitochondrial replication.6 The gene consists of 23 exons and has two functional domains; one polymerase (pol) domain in the carboxy-terminal region and one 3′–5′ exonuclease (exo) domain in the amino-terminal region with proofreading activity.7 The mechanism for the secondary accumulations of mtDNA deletions caused by the primary nuclear gene defects is presently unknown. Deletions have been shown to expand clonally within muscle fiber segments and thereby cause mitochondrial myopathy with cytochrome c oxidase (COX)-deficient muscle fibers.8 It has also been demonstrated that mutated Pol γ has reduced fidelity and gives rise to error-prone DNA synthesis with increased frequency of base substitutions in cultured human cells9 as well as in transgenic mice.10 A model for large-scale deletions to occur secondary to base substitutions near direct repeats in mtDNA in patients with POLG1 mutations has been proposed.11 In this study, we investigated, in PEO patients with POLG1 mutations, whether point mutations, like deletions, are clonally expanded in muscle fibers and thus contribute to the pathogenesis in PEO. We also studied whether point mutations appear near direct repeats in mtDNA, and thus may contribute to the formation of large-scale deletions. Since POLG1 contains different functional domains, patients with mutations affecting either the polymerase or the exonuclease part of Pol γ were selected.
Materials and methods
Patients
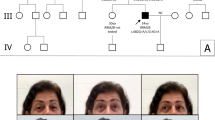
Three female patients (P1–P3) from a Swedish family with adPEO and a POLG1 mutation were included in the single fiber study (Table 1). For the cloning/direct sequencing analysis, one female and one male patient from the same adPEO family were selected (P3–P4), together with a 75-year-old man (P5) with apparently sporadic PEO and POLG1 mutations. A more detailed description of the adPEO patients is given elsewhere,8 where P1–P4 correspond to IV:5, IV:8, IV:2 and IV:4. The clinical features of P5 related to the mtDNA disease were restricted to severe ophthalmoplegia and ptosis, which appeared insidiously and had been present clinically since the age of 55. Muscle biopsy at age 68 revealed mitochondrial myopathy, as well as muscle inflammation with granulomas. Subsequent investigations confirmed that the patient suffered from sarcoidosis. At that time, the patient had developed a mild generalized muscle weakness that responded well to prednisolone treatment. Subsequent biopsies revealed only mitochondrial myopathy. Family members of P5 were not available. As controls, we used muscle biopsies from two individuals aged 75 and 78, with no sign of neuromuscular disease.
Morphological analysis
Muscle biopsy specimens were obtained from m. quadriceps femoris from patients and controls. Morphological and enzyme histochemical analyses were performed as described.12
Analysis of POLG1 mutations
Mutations in POLG1 were identified by direct sequencing of genomic DNA, using an ABI Prism 377 DNA sequencer, and the Big Dye Terminator Kit v.1.1. (Applied Biosystems, Foster City, CA, USA). We used a set of primers that amplified all the exons with flanking intronic sequences of POLG1, except the nontranslated exon 1 (primers and PCR conditions available on request).
Analysis of mtDNA deletions
Total DNA was extracted from frozen muscle tissue using the DNA Extraction Kit (Qiagen, Hilden, Germany). Long expand polymerase chain reaction (LX-PCR) was performed as described.13 Using this method, a 10.8 kb fragment of mtDNA, including the ‘major arc’, is amplified. The PCR products were separated on a 0.6% agar gel stained with GelStar® and visualized on a Dark Reader Blue light transilluminator (Clare Chemical Research, Dolores, CO, USA).
Analysis of clonal expansion of mtDNA mutations in single muscle fibers
Single COX-deficient muscle fiber segments from patients P1–P3 were dissected with a tungsten needle and subjected to alkaline lysation as described.8 Since mtDNA mutations causing COX deficiency usually affect tRNA genes, point mutations were searched for in three different regions of mtDNA, containing five mitochondrial tRNA genes, tRNALeu(UUR), tRNAIle, tRNAGln, tRNAMet and tRNALys (Table 2). PCR analysis with Pwo polymerase and denaturing gradient gel electrophoresis (DGGE) were performed as described,14, 15 using the DcCodeTM Detection System (Bio-Rad Laboratories AB, Sundbyberg, Sweden) for gel casting and migration. The conditions for DGGE are described in Table 2.
Analysis of mtDNA point mutations in muscle homogenate
Two mtDNA regions adjacent to deletion breakpoints13, 16 were amplified from patients P3–P5 and controls. Primers F8197–8216 and R8558–8537 were used to amplify a 362-bp fragment including the 5′ breakpoint of the ‘common deletion’ (ie position 8469). Primers F15791–15810 and R16150–16130 were used to amplify a 360 bp fragment, which includes a cluster of predominant 3′ deletion breakpoints, associated with PEO, at nucleotide position 16069–78. This fragment also contains part of the D-loop and the hypervariable segment 1 (HV1). In addition, within the PCR products, three tRNA genes are also amplified: tRNALys (nt 8295–8364), tRNAThr (nt 15888–15953) and tRNAPro (nt 15955–16023). The numbering of mtDNA is according to the revised Cambridge sequence.17 The thermocycling reactions were performed in a 50 μl volume containing approximately 50 ng of total DNA, 2.5 U of Pwo polymerase (Roche Diagnostics GmbH, Mannheim, Germany), 0.8 mM dNTP mix, 1–1.5 mM MgSO4, and 1 × PCR-buffer without MgSO4 supplied by the manufacturer. The PCR parameters were as follows: initial 94°C for 3 min, 35 cycles of 94°C/1 min, 57°C/1 min, 72°C/1 min, and a final extension step at 72° for 7 min. Purified PCR products were ligated into a pCR®-Blunt II-TOPO® vector using the Zero Blunt TOPO PCR cloning kit (Invitrogen, Carlsbad, CA, USA) and transformed into Escherichia coli. Bacterial colonies were grown on selective Kan® plates for 24–48 h. For screening, colonies were resuspended in aliquots of ReddyMix™ PCR Master Mix (ABgene®House, Surrey, UK), together with M13 Forward and Reverse primers, 10 pmol of each. Verifications for the presence of inserted fragments were made on a 1% agarose gel. Plasmids positive for inserts were sequenced and analyzed with MacVector® software 7.1.1. All PCR amplifications were performed with a GeneAmp PCR system 2700 (Applied Biosystems, Foster City, CA, USA).
Results
Morphological analysis
Muscle biopsies from all patients displayed mitochondrial myopathy with numerous COX-negative fibers and ragged red fibers (Figure 1). Biopsies from the two normal controls contained no COX-negative fibers.
Analysis of POLG1 mutations
In patients from the adPEO family, the sequencing of exon 18 identified a heterozygous A2864G transition, leading to amino-acid substitution Y955C in the polymerase domain of Pol γ (Figure 2). In the sporadic case (P5), all the coding exons of POLG1 were sequenced and revealed three heterozygous mutations: C752T in exon 3, C1760T in exon 10 and G2542A in exon 16, leading to amino-acid substitutions T251I, P587L and G848S, respectively (Figure 2). T251 is located between the exonuclease motifs I and II, while P587 and G848 reside in the spacer tract between the two functional domains. Numbering is according to the reference sequence (NM_002693).
The upper part illustrates the map of human Pol γ with its different functional domains. Sequencing analysis of the 22 coding exons of POLG1 revealed one heterozygous mutation in individuals from the adPEO family (black box) and three presumably recessive mutations in the sporadic PEO case (white boxes).
Analysis of mtDNA deletions
All patients had multiple mtDNA deletions in muscle tissue. Most deletions described in PEO reside within the ‘major arc’ between the origins of replications in the heavy and light chains of mtDNA, which is amplified with the LX-PCR method used here. Separation with gel electrophoresis revealed that, in addition to a normal 10.8-kb band, several smaller bands corresponding to multiple deleted fragments of mtDNA were visible in PCR-products from patients but not in the normal controls. LX-PCR products from P4 and P5 are illustrated in Figure 3.
GelStar® staining of Long PCR amplifications separated on a 0.6% agar gel, which illustrates a normal 10.8 kb amplified fragment from two of the PEO patients, P4 (adPEO) and P5 (arPEO). Several smaller bands, corresponding to multiple deleted mtDNA fragments, are present in patients. NC=normal control (50 years).
Analysis of clonal expansion of mtDNA mutations in single muscle fibers
Among 136 analyzed COX-deficient fibers from adPEO patients P1–P3, no fibers with point mutations were detected with the DGGE method.
Analysis of mtDNA point mutations in muscle homogenate
In total, 323 plasmids containing one of the regions (8197–8558) and 309 plasmids with the other region (15791–16150) were sequenced, which corresponds to 228 166 bp of mtDNA. In the colonies from the patient with sporadic PEO, P5, two unique mutations were identified, T8240C and C8532A, in two separate colonies. These mutations are novel and not reported elsewhere. In addition, this patient had three other variants in mtDNA compared with the revised Cambridge sequence:17 two homoplasmic variants (G8251A, A15924G) and one heteroplasmic variant (G16129A). They are reported to be common polymorphisms among populations, even the heteroplasmic variant in HV1. In P3, a single A → G transition at position 16070 was found in one colony. This variant is reported as a polymorphism. The same polymorphism as in P5, the homoplasmic A15924G substitution, was present in P3 and was also present as the only variant in P4. In the control samples there was one single base substitution, A15923C, and one of the controls had a homoplasmic polymorphic G15928A transition. The results are summarized in Table 3. Single mutations were confirmed by resequencing the same insert by analyzing an additional sample of the colony.
Discussion
PEO (MIM# 157640) is associated with multiple mtDNA deletions in postmitotic tissues such as skeletal muscle and brain. The deletions are clonally expanded in single muscle fibers.8 The identification of mutations in POLG1 in patients with PEO has raised the question of whether mtDNA point mutations contribute to the pathogenesis of the disease.
We investigated the hypothesis that point mutations associated with direct repeats contribute to the formation of multiple deletions. In a model for the formation of large-scale deletions, it was suggested that an enhanced base substitution error rate of Y955C Pol γ, in association with direct repeats in mtDNA, would promote deletions between such repeats, for example, the 4977-bp ‘common-deletion’ that is flanked by a 13-bp exact repeat on each side.11 We examined cloned PCR-products from two different regions in mtDNA, including the 5′-breakpoint for common deletion (mtDNA position 8469) and a cluster of 3′-deletion breakpoints in the D-loop (position 16069–16078) associated with PEO. All the patients in our study harbored the common deletion as well as deletions with breakpoints in the investigated part of the D-loop (Moslemi et al13 and unpublished results). The frequency of point mutations was very low in patients and controls. The two identified point mutations of 5.3 × 104 examined bases in P5 can be explained by the patient's age at the time of biopsy (75 years), in agreement with findings in normal elderly people, where clonally expanded point mutations in addition to large-scale deletions have been identified in COX-deficient fibers.15
To identify clonal expansions of mtDNA point mutations in COX-deficient single muscle fibers, we used a highly sensitive DGGE method.14, 15 In total, 136 COX-deficient fibers were analyzed, but no point mutations were identified in any of them. Since the whole mtDNA genome has not been examined, and thereby not all the regions associated with COX deficiency (ie COX genes and tRNA genes), pathogenic point mutations in the analyzed COX-deficient fibers cannot be excluded. It is, however, very unlikely that five of 22 tRNA genes would have been spared, if scattered point mutations were present in the mtDNA of adPEO patients. In addition, the cloned PCR products from muscle homogenate did not reveal any pathogenic point mutations in the amplified tRNA genes. Our findings support the concept that the clonal expansion of large-scale deletions and not point mutations account for the pathogenesis of mitochondrial myopathy in adPEO. This differs from the findings obtained in studies on COX-deficient fibers from normal elderly individuals15 and, therefore, the events leading to mitochondrial myopathy with COX-deficient fibers are probably different in adPEO and aging.
Wanrooij et al18 investigated in a recent study the levels of mtDNA point mutations in ad/arPEO patients with Twinkle or POLG1 mutations. They performed mutation analyses in both deleted and nondeleted mtDNA molecules and found an age-dependent increase of point mutations in patients specifically in the mtDNA control region. The deleted molecules did not prove to have higher mutation load than the nondeleted. Their results, as well as ours, do not support a generalized decrease in mtDNA replication fidelity in patients with POLG1 mutations. The authors proposed replication stalling as the principal cause of deletion formation. Another recently published study19 indicated a high load of point mutations in mtDNA amplified from the muscle tissue of PEO patients with POLG1 mutations, particularly in the exonuclease domain. Methodological differences can explain the discrepancy between the results, since we used a polymerase with proofreading activity, Pwo, which increases the fidelity of DNA synthesis compared with Taq polymerase at PCR.
Among the nuclear gene defects associated with either adPEO or arPEO, mutations in POLG1 appear to be the most frequent.5, 20 The dominant mutations in Pol γ described thus far are located in the polymerase domain of the enzyme, whereas recessive mutations are located mainly in the exonuclease part or in the spacer tract between the two functional domains. This might indicate differences in pathogenicity between dominant and recessive POLG1 mutations. Indeed, Y766A- and Y766S-substituted pol I in E. coli have been shown to enhance the formation of deletions between direct repeat sequences,21 and amino-acid sequence alignment reveals equivalence with the highly conserved Tyr-955 residue in the polymerase domain of Pol γ in humans.11 Moreover, the expression of Pol γ with abolished proofreading activity was shown to induce point mutations in cultured human cells9 and, in proofreading-deficient mtDNA ‘mutator-mice’, there was a substantial mtDNA mutation load already by 2 months of age.10 However, the first and most prominent features in mtDNA of these mice were deletions.
In patients with POLG1 mutations, similar hallmarks are observed despite clinical and genetic heterogeneity, that is, PEO and multiple deletions in mtDNA. These facts, together with our results, support the concept of similar pathogenic mechanisms in both adPEO and arPEO.
How multiple mtDNA deletions arise are not known, but Nishigaki et al22 made speculations concerning mtDNA deletion formation in a recent study on patients with mitochondrial neurogastrointestinal encephalomyopathy (MNGIE). MNGIE is caused by mutations in the nuclear gene encoding thymidine phosphorylase (TP) and is also associated with secondary mtDNA deletions.3 In addition to slipped mispairing or illegitimate elongation models, a homologous recombination mechanism was discussed. Homologous recombination can occur in nonreplicating mtDNA and generate deleted molecules lacking OH. This mechanism can also cause branch migration within imperfectly homologous sequences and explain features like microdeletions. It appears that the pattern of deletion breakpoints is similar in conditions with impaired mtDNA maintenance due to mutations in different nuclear genes such as POLG1,13 Twinkle18 and TP,22 but to make detailed comparisons, mapping of deletion breakpoints should be performed with the same method for all conditions.
The Y955C substitution identified in the adPEO family was first described in a large Belgian family in 20011 and was subsequently found in several families with adPEO.5 The mutation is fully penetrant and associated with a severe phenotype. In P5, there were three heterozygous mutations leading to previously described amino-acid substitutions; T251I,5, 23 P587L23, 24 and G848S.5 The precise role of the three mutations acting together remains to be further evaluated.
Our results indicate that it is very unlikely that point mutations in mtDNA contribute to the pathogenesis of the mitochondrial myopathy in PEO associated with POLG1 mutations, which is characterized by accumulation of multiple large-scale deletions of mtDNA. To understand the molecular mechanism for causing these deletions, it is important to develop tools to study the functional effects of different POLG1 mutations.25 Furthermore, it would be of interest to compare the spectrum of mtDNA deletion breakpoints in PEO associated with mutations in different nuclear genes to investigate whether such nuclear gene mutations act by common mechanisms causing multiple mtDNA deletions.
References
Van Goethem G, Dermaut B, Lofgren A, Martin JJ, Van Broeckhoven C : Mutation of POLG is associated with progressive external ophthalmoplegia characterized by mtDNA deletions. Nat Genet 2001; 28: 211–212.
Kaukonen J, Juselius JK, Tiranti V et al: Role of adenine nucleotide translocator 1 in mtDNA maintenance. Science 2000; 289: 782–785.
Nishino I, Spinazzola A, Hirano M : Thymidine phosphorylase gene mutations in MNGIE, a human mitochondrial disorder. Science 1999; 283: 689–692.
Spelbrink JN, Li FY, Tiranti V et al: Human mitochondrial DNA deletions associated with mutations in the gene encoding Twinkle, a phage T7 gene 4-like protein localized in mitochondria. Nat Genet 2001; 28: 223–231.
Lamantea E, Tiranti V, Bordoni A et al: Mutations of mitochondrial DNA polymerase gammaA are a frequent cause of autosomal dominant or recessive progressive external ophthalmoplegia. Ann Neurol 2002; 52: 211–219.
Clayton DA : Replication of animal mitochondrial DNA. Cell 1982; 28: 693–705.
Ropp PA, Copeland WC : Cloning and characterization of the human mitochondrial DNA polymerase, DNA polymerase gamma. Genomics 1996; 36: 449–458.
Moslemi AR, Melberg A, Holme E, Oldfors A : Clonal expansion of mitochondrial DNA with multiple deletions in autosomal dominant progressive external ophthalmoplegia. Ann Neurol 1996; 40: 707–713.
Spelbrink JN, Toivonen JM, Hakkaart GA et al: In vivo functional analysis of the human mitochondrial DNA polymerase POLG expressed in cultured human cells. J Biol Chem 2000; 275: 24818–24828.
Trifunovic A, Wredenberg A, Falkenberg M et al: Premature ageing in mice expressing defective mitochondrial DNA polymerase. Nature 2004; 429: 417–423.
Ponamarev MV, Longley MJ, Nguyen D, Kunkel TA, Copeland WC : Active site mutation in DNA polymerase gamma associated with progressive external ophthalmoplegia causes error-prone DNA synthesis. J Biol Chem 2002; 277: 15225–15228.
Oldfors A, Moslemi AR, Fyhr IM, Holme E, Larsson NG, Lindberg C : Mitochondrial DNA deletions in muscle fibers in inclusion body myositis. J Neuropathol Exp Neurol 1995; 54: 581–587.
Moslemi AR, Melberg A, Holme E, Oldfors A : Autosomal dominant progressive external ophthalmoplegia: distribution of multiple mitochondrial DNA deletions. Neurology 1999; 53: 79–84.
Sternberg D, Danan C, Lombes A et al: Exhaustive scanning approach to screen all the mitochondrial tRNA genes for mutations and its application to the investigation of 35 independent patients with mitochondrial disorders. Hum Mol Genet 1998; 7: 33–42.
Fayet G, Jansson M, Sternberg D et al: Ageing muscle: clonal expansions of mitochondrial DNA point mutations and deletions cause focal impairment of mitochondrial function. Neuromuscul Disord 2002; 12: 484–493.
Zeviani M, Servidei S, Gellera C, Bertini E, DiMauro S, DiDonato S : An autosomal dominant disorder with multiple deletions of mitochondrial DNA starting at the D-loop region. Nature 1989; 339: 309–311.
Andrews RM, Kubacka I, Chinnery PF, Lightowlers RN, Turnbull DM, Howell N : Reanalysis and revision of the Cambridge reference sequence for human mitochondrial DNA. Nat Genet 1999; 23: 147.
Wanrooij S, Luoma P, van Goethem G, van Broeckhoven C, Suomalainen A, Spelbrink JN : Twinkle and POLG defects enhance age-dependent accumulation of mutations in the control region of mtDNA. Nucleic Acids Res 2004; 32: 3053–3064.
Del Bo R, Bordoni A, Sciacco M et al: Remarkable infidelity of polymerase gammaA associated with mutations in POLG1 exonuclease domain. Neurology 2003; 61: 903–908.
Agostino A, Valletta L, Chinnery PF et al: Mutations of ANT1, Twinkle, and POLG1 in sporadic progressive external ophthalmoplegia (PEO). Neurology 2003; 60: 1354–1356.
Bell JB, Eckert KA, Joyce CM, Kunkel TA : Base miscoding and strand misalignment errors by mutator Klenow polymerases with amino acid substitutions at tyrosine 766 in the O helix of the fingers subdomain. J Biol Chem 1997; 272: 7345–7351.
Nishigaki Y, Marti R, Hirano M : ND5 is a hot-spot for multiple atypical mitochondrial DNA deletions in mitochondrial neurogastrointestinal encephalomyopathy. Hum Mol Genet 2004; 13: 91–101.
Van Goethem G, Schwartz M, Lofgren A, Dermaut B, Van Broeckhoven C, Vissing J : Novel POLG mutations in progressive external ophthalmoplegia mimicking mitochondrial neurogastrointestinal encephalomyopathy. Eur J Hum Genet 2003; 11: 547–549.
Filosto M, Mancuso M, Nishigaki Y et al: Clinical and genetic heterogeneity in progressive external ophthalmoplegia due to mutations in polymerase gamma. Arch Neurol 2003; 60: 1279–1284.
Graziewicz MA, Longley MJ, Bienstock RJ, Zeviani M, Copeland WC : Structure-function defects of human mitochondrial DNA polymerase in autosomal dominant progressive external ophthalmoplegia. Nat Struct Mol Biol 2004; 11: 770–776.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was supported by the Swedish Research Council (Project No. 7122 to AO and10823 to EH) and the Ländell foundation to AM.
Rights and permissions
About this article
Cite this article
Kollberg, G., Jansson, M., Pérez-Bercoff, Å. et al. Low frequency of mtDNA point mutations in patients with PEO associated with POLG1 mutations. Eur J Hum Genet 13, 463–469 (2005). https://doi.org/10.1038/sj.ejhg.5201341
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ejhg.5201341