Abstract
Molecular diagnosis makes a substantial contribution to precise diagnosis, subclassification, prognosis, and selection of therapy. Mutations in the PDS (SLC26A4) gene are known to be responsible for both Pendred syndrome and nonsyndromic hearing loss associated with enlarged vestibular aqueduct, and the molecular confirmation of the PDS gene has become important in the diagnosis of these conditions. In the present study, PDS mutation analysis confirmed that PDS mutations were present and significantly responsible in 90% of Pendred families, and in 78.1% of families with nonsyndromic hearing loss associated with enlarged vestibular aqueduct. Furthermore, variable phenotypic expression by the same combination of mutations indicated that these two conditions are part of a continuous category of disease. Interestingly, the PDS mutation spectrum in Japanese, including the seven novel mutations revealed by this study, is very different from that found in Caucasians. Of the novel mutations detected, 53% were the H723R mutation, suggesting a possible founder effect. Ethnic background is therefore presumably important and should be noted when genetic testing is being performed. The PDS gene mutation spectrum in Japanese may be representative of those in Eastern Asian populations and its elucidation is expected to facilitate the molecular diagnosis of a variety of diseases.
Similar content being viewed by others
Introduction
The Pendred syndrome is defined as an autosomal recessive disorder characterized by congenital sensorineural hearing loss and goiter.1 It is supposed that Pendred syndrome, the most common form of syndromic deafness, is as frequent as 7.5–10 per 100 000 persons and accounts for about 10% of hereditary hearing impairment.2,3 In spite of such a high frequency, the precise clinical diagnosis has long been hampered by the variable phenotypes, the degree of involvement of goiter, appearance from congenital to complete absence, and the perchlorate discharge test which is nonspecific to Pendred syndrome.3 However, the recent identification of the PDS gene4 as being responsible for Pendred syndrome enables us to perform molecular evaluation of this syndrome. Simultaneously, the PDS gene has also been reported to cause ‘nonsyndromic hearing loss with enlarged vestibular aqueduct (EVA)’,5 suggesting that the PDS gene may cover a wider range of diseases from typical Pendred syndrome to nonsyndromic hearing loss with EVA. Therefore, molecular genetic testing is becoming more important to diagnose this category of disease caused by the PDS gene.
The frequencies and nature of mutations are known to be influenced by ethnic differences and geographic isolation. Although much is known regarding the association of PDS mutations with deafness in populations of European descent, data about the ethnic groups that form the majority of the world's population is scarce. In the present study, screening of PDS mutations was carried out to confirm their contribution to the deafness in patients diagnosed with Pendred syndrome or nonsyndromic hearing loss with EVA, and to reveal the spectrum of the PDS gene in Japanese.
Materials and methods
A total of 10 Japanese families, in which some individuals had been diagnosed with Pendred syndrome, and 32 Japanese families, in which some individuals had bilateral sensorineural hearing loss associated with EVA but without goiter, participated in the current study. We defined Pendred syndrome patients as those having either a palpable goiter or abnormal perchlorate discharge. Computerized tomography scan was used to diagnose EVA patients (according to the criteria of EVA: a diameter greater than 1.5 mm at the midpoint between the common crus and the external aperture), and they were clinically well characterized by repeated auditory examinations and long follow-up periods. Briefly, the EVA patients had congenital, high frequency involved, fluctuating, sometimes progressive, sensorineural hearing loss.6,7 There were no cases of Mondini malformation (cochlear hypoplasia) of the inner ear in the current subjects.
DNA samples from 96 unrelated Japanese, who had normal hearing, were used as controls. All participants gave informed consent for genetic analysis.
Mutation analysis
Intronic polymerase chain reaction (PCR) amplification primers flanking each exon4 were used to detect mutations. Exons 1–21 of PDS were amplified from genomic DNA samples by PCR. A 5-min denaturation at 95°C was followed by 37 three-step cycles (95°C for 30 s, 55°C for 1 min, 72°C for 1 or 3 min), followed by 72°C for 10 min, and ending with a holding period at 4°C in a Perkin-Elmer thermal cycler. The PCR products were directly sequenced after removal of unincorporated dNTPs and primers by incubation at 37°C for 30 min with 50–100 ng PCR product with 0.1 μl exonuclease I (Amersham Life Science, Cleveland, USA) and 1 μl shrimp alkaline phosphatase (Amersham Life Science). The enzymes were heat-inactivated at 80°C for 15 min. An aliquot of 6 pmol of either the forward or the reverse primer was used in standard cycle sequencing reactions with ABI Big Dye terminators, and run on an ABI 377 sequencer.
Results
Table 1 5,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23 summarizes all reported PDS mutations including the 18 mutations detected in the affected families in this study, which were 10 missense mutations, one stop mutation, four frameshift mutations, and three splice site mutations. The evolutionary conservation of the amino acids affected by the missense mutations, on the basis of the alignment of the closely related mouse pendrin protein and rat pendrin protein, are shown in Table 1 and Figure 1. All 10 missense mutations had occurred at the conservative residues among humans, mice, and rats (Figure 1). Mutations were identified in nine out of the 10 typical Pendred families (90%) and 25 out of the 32 families with sensorineural hearing loss associated with EVA (78.1%). Mutations were either homozygous, compound heterozygous, or heterozygous but with no other mutations detectable (Table 2).
Multiple-sequence alignment of selected proteins with significant sequence homology to human pendrin. The amino-acid sequence of human pendrin (hum-pendrin) is aligned relative to the sequences of the mouse pendrin (mse-pendrin) and rat pendrin (rat-pendrin). Positions exhibiting absolute identity among the three proteins are shown with a black background. The black background regions lead evolutionary conservation. The regions with asterisks (*) denote the missense mutations detected in our study.
Missense mutations
The 10 missense mutations detected were: P123S (367C>T in exon 4); M147V (439A>G in exon 5); K369E (1105A>G in exon 9); A372V (1115C>T in exon 9); N392Y (1174A>T in exon 10); C565Y (1694G>A in exon 15); S657N (1970G>A in exon 17); S666F (1997C>T in exon 17); T721M (2162C>T in exon 19), and H723R (2168A>G in exon 19).
Stop mutation
An 1829C>A substitution was found in exon 17, leading to S610X.
Frameshift mutations
Four frameshift mutations were detected: 322delC in exon 4 causing a frameshift at codon 108 and leading to a stop codon at position 139; 917delT in exon 7 causing a frameshift at codon 307 and leading to a stop codon at position 308; 1652insT in exon 15 causing a frameshift at codon 551 and leading to a stop codon at position 556; and a small 2111 insertion of GCTGC in exon 19 causing a frameshift leading to an amino-acid sequence change from codon 704, followed by a stop at codon 722.
Splice site mutations
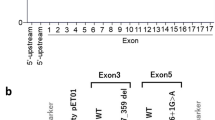
The three splice site mutations found were: IVS5-1G>A (exon 6 acceptor splice site); IVS7-2A>G (exon 8 acceptor splice site); and IVS8+1G>A (exon 8 donor splice site).
Mutations found in unaffected controls
Of the 18 mutations identified in the Pendred syndrome and EVA families, only the H723R mutation was found in a single control subject (one out of 192 alleles).
Differences between Japanese and those with Caucasoid ancestry
Figure 2 shows a schematic representation of the PDS gene and the approximate positions of mutations found in Japanese, and those found in families with European ancestry.
Differences in PDS mutation spectrums between Japanese and the populations with European ancestry. Shaded arrows indicate approximate localization of PDS mutations found in the Caucasoid populations, filled arrows are localization of mutations found in Japanese and white arrows are the mutations that have been reported in both Caucasoid and Japanese families.
Genotype–phenotype correlation
Table 2 summarizes phenotype–genotype correlation. One mutation, IVS5-1G>A, was found in the Pendred syndrome family, whereas 11 mutations, P123S, M147V, K369E, C565Y, S657N, S666F, S610X, 322delC, 917delT, IVS7-2A>G, and IVS8+1 G>A were detected in families with nonsyndromic hearing loss associated with EVA. The other six mutations, A372V, N392Y, T721M, H723R, 1652insT, and 2111ins5bp, were found in both EVA and Pendred syndrome families.
Discussion
Recent advances in molecular genetics as well as radiology have provided reliable diagnostic criteria for Pendred syndrome. After identification of the gene responsible for Pendred syndrome, PDS,4 it has become possible to diagnose this syndrome from the molecular genetic viewpoint. This is noteworthy because of the possible molecular diagnostic applications for affected individuals. Furthermore, mutations in PDS were found in nonsyndromic hearing loss associated with EVA, suggesting that this gene may give rise to different pathologic phenotypes.5
The appearance of EVA by CT/MRI is demonstrated to be a reliable radiological marker, and has become one of the reliable diagnostic criteria for Pendred syndrome.24 According to Phelps et al,24 EVA was found in a majority of Pendred syndrome patients, but Mondini deformity, which had been thought to be a characteristic radiological feature of Pendred syndrome, was not found. Based on molecular genetics and radiological evaluation, Pendred syndrome and nonsyndromic hearing loss associated with EVA are currently thought to be a continuum of disease caused by PDS mutations; that is, hearing loss associated with EVA with/without goiter.
In the present study, causative mutations have been identified in 90% of typical Pendred families and 78.1% of those with sensorineural hearing loss associated with EVA. The results confirmed a new category of disease caused by mutations in PDS, encompassing a range from ‘classic’ Pendred syndrome to nonsyndromic hearing loss associated with EVA.
To date, 66 mutations causing Pendred syndrome and nonsyndromic hearing loss with EVA have been reported in the PDS gene (Table 1). We have previously reported seven mutations, K369E, A372V, T721M, H723R, 917delT, 1652insT, and 2111ins5bp, in Japanese families with nonsyndromic hearing loss with EVA or Pendred syndrome.5,22 Kitamura et al25 reported the T410M mutation in a family with nonsyndromic hearing loss with EVA. The present study added 12 mutations including seven novel PDS mutations: 322delC, P123S, M147V, IVS5-1G>A, S610X, S657N, and S666F. It is likely that these are pathologic mutations rather than rare or functionally neutral polymorphic changes because: (1) none of the novel mutations represented here were found in any of the controls, (2) these mutations were highly associated with affected subjects in which mutations were found to be homozygous or compound heterozygous, also indicating that they may be disease-causing mutations, and (3) all of the missense mutations found in our study had occurred at amino-acid residues that were conserved in the rat and the mouse (Figure 1). The present study revealed a unique spectrum of PDS mutations quite different from that found in the populations with European ancestry. Of the 19 mutations found in Japanese, only five mutations were also found in European populations (Figure 2), further suggesting a founder effect of these mutations as demonstrated in frequent mutations in GJB2.26,27 In the Caucasoid populations, three frequent mutations, L236P (16%), T416P (15%), and IVS8+1G>A (14%), account for nearly half of all PDS mutant alleles.8 In contrast, these mutations are rare in Japanese (L236P, 0%; T416P, 0%; and IVS8+1G>A, 2%), whereas H723R accounted for 53% of PDS mutations. A recent report suggested that the cause of the frequent mutation (H723R) was the existence of a common ancestor rather than a mutational hot spot.16 The spectrum of PDS mutations revealed by the present study will facilitate the effective molecular diagnosis of a category of disease caused by the PDS gene.
Pendrin, the transmembrane protein encoded by the PDS gene, is expressed in the inner ear, thyroid gland, and kidney.4,19,28 In Xenopus oocytes and Sf9 cells, it has been demonstrated that pendrin transports chloride and iodine, and mediates the exchange of chloride and formate.19,29 The mutations associated with Pendred syndrome showed complete loss of pendrin-induced chloride and iodide transport, whereas alleles associated with nonsyndromic sensorineural hearing loss with EVA showed partial transport function, which may be sufficient to maintain thyroid function and eliminate goiter.19 With regard to genotype–phenotype correlation, four mutations, P123S, S610X, S666F, and H723R, were found to be homozygous (Table 2). In these cases, the phenotype would reflect the function of the respective mutations. The former three mutations caused nonsyndromic sensorineural hearing loss with EVA, and therefore may have residual transport function. However, the homozygous H723R mutation caused either Pendred syndrome or nonsyndromic sensorineural hearing loss with EVA, making the story more complex. Actually, patient #38 showed a huge goiter and tracheostomy was necessary because of dyspnea,30 whereas three out of eight patients did not show any goiter. Phenotypic variability has also been reported in two families carrying the same PDS missense mutation (L445W).31 A modifier gene or environmental factor (iodine uptake, nutrition, etc.) may contribute to such variability.
In the present study, one out of 10 families with Pendred syndrome and seven out of 32 families with nonsyndromic hearing loss associated with EVA did not show any mutations. This suggests that mutations possibly exist in the activate cryptic splice sites in the introns or that they occur in the promoter region, which was not analyzed in this study. An alternative explanation may be that other genes were responsible for those families without PDS mutations. According to Hulander et al,32 Foxi1 is an upstream regulator of pendrin, and defective pendrin-mediated chloride ion resorption in the endolymphatic duct/sac epithelium accounts for the phenotype seen in Foxi1-null mice. Therefore, it is possible that mutations in FOXI1 cause Pendred syndrome in humans.
In conclusion, the present study confirmed that a range of disease from ‘classical’ Pendred syndrome to nonsyndromic hearing loss associated with EVA is dependent on the PDS mutations. Our findings also represented a unique spectrum of the PDS gene in Japanese, which is distinct from that found in the populations with European ancestry. The present study clearly indicates that the establishment of databases for different populations will facilitate the molecular diagnosis of a clinically complex disease.
References
Pendred V : Deaf mutism and goitre. Lancet 2 1896; 532.
Fraser GR : Association of congenital deafness with goitre (Pendred's syndrome): a study of 207 families. Ann Hum Genet 1965; 28: 411–422.
Reardon W, Coffey R, Phelps PD et al: Pendred syndrome: 100 years of underascertainment? Q J Med 1997; 90: 443–447.
Everett LA, Glaser B, Beck JC et al: Pendred syndrome is caused by mutations in a putative sulphate transporter gene (PDS). Nat Genet 1997; 17: 411–422.
Usami S, Abe S, Weston MD et al: Non-syndromic hearing loss associated with enlarged vestibular aqueduct is caused by PDS mutations. Hum Genet 1999; 104: 188–192.
Valvassori GE, Clemis JD : The large vestibular aqueduct syndrome. Laryngoscope 1978; 88: 723–728.
Abe S, Usami S, Shinkawa H : Three familial cases of hearing loss associated with enlargement of the vestibular aqueduct. Ann Otol Rhinol Laryngol 1997; 106: 1063–1069.
Campbell C, Cucci RA, Prasad S et al: Pendred syndrome, DFNB4, and PDS/SLC26A4: identification of eight novel mutations and possible genotype–phenotype correlations. Hum Mutat 2001; 17: 403–411.
Lopez-Bigas N, Melchionda S, de Cid R et al: Identification of five new mutations of PDS/SLC26A4 in Mediterranean families with hearing impairment. Hum Mutat 2002; 18: 548.
Kopp P, Arseven OK, Sabacan L et al: Phenocopies for deafness and goiter development in a large inbred Brazilian kindred with Pendred's syndrome associated with a novel mutation in the PDS gene. J Clin Endocrinol Metab 1999; 84: 336–341.
Coyle B, Reardon W, Herbrick JA et al: Molecular analysis of the PDS gene in Pendred syndrome. Hum Mol Genet 1998; 7: 1105–1112.
Reardon W, O Mahoney CF, Trembath R et al: Enlarged vestibular aqueduct: a radiological marker of Pendred syndrome, and mutation of the PDS gene. Q J Med 2000; 93: 99–104.
Van Hauwe P, Everett LA, Coucke P et al: Two frequent missense mutations in Pendred syndrome. Hum Mol Genet 1998; 7: 1099–1104.
Lopez-Bigas N, Rabionet R, de Cid R et al: Splice-site mutation in the PDS gene may result in intrafamilial variability for deafness in Pendred syndrome. Hum Mutat 1999; 14: 520–526.
Adato A, Raskin L, Petit C et al: Deafness heterogeneity in a Druze isolate from the Middle East: novel OTOF and PDS mutations, low prevalence of GJB2 35delG mutation and indication for a new DFNB locus. Eur J Hum Genet 2000; 8: 437–442.
Park HJ, Shaukat S, Liu XZ et al: Origins and frequencies of SLC26A4 (PDS) mutations in east and south Asians: global implications for the epidemiology of deafness. J Med Genet 2003; 40: 242–248.
Coucke PJ, Van Hauwe P, Everett LA et al: Identification of two different mutations in the PDS gene in an inbred family with Pendred syndrome. J Med Genet 1999; 36: 475–477.
Yong AM, Goh SS, Zhao Y et al: Two Chinese families with Pendred's syndrome: radiological imaging of the ear and molecular analysis of the pendrin gene. J Clin Endocrinol Metab 2001; 86: 3907–3911.
Scott DA, Wang R, Kreman TM : Functional differences of the PDS gene product are associated with phenotypic variation in patients with Pendred syndrome and non-syndromic hearing loss (DFNB4). Hum Mol Genet 2000; 9: 1709–1715.
Li XC, Everett LA, Lalwani AK et al: A mutation in PDS causes non-syndromic recessive deafness. Nat Genet 1998; 18: 215–217.
Bogazzi F, Raggi F, Ultimieri F et al: A novel mutation in the pendrin gene associated with Pendred's syndrome. Clin Endocrinol (Oxf) 2000; 52: 279–285.
Namba A, Abe S, Shinkawa H et al: Genetic features of hearing loss associated with ear anomalies: PDS and EYA1 mutation analysis. J Hum Genet 2001; 46: 518–521.
Fugazzola L, Mannavola D, Cerutti N et al: Molecular analysis of the Pendred's syndrome gene and magnetic resonance imaging studies of the inner ear are essential for the diagnosis of true Pendred's syndrome. J Clin Endocrinol Metab 2000; 85: 2469–2475.
Phelps PD, Coffey RA, Trembath RC et al: Radiological malformations of the ear in Pendred syndrome. Clin Radiol 1998; 53: 268–2273.
Kitamura K, Takahashi K, Noguchi Y et al: Mutations of the Pendred syndrome gene (PDS) in patients with large vestibular aqueduct. Acta Otolaryngol 2000; 120: 137–141.
Van Laer L, Coucke P, Mueller RF et al: A common founder for the 35delG GJB2 gene mutation in connexin 26 hearing impairment. J Med Genet 2001; 38: 515–518.
Ohtsuka A, Yuge I, Kimura S et al: GJB2 deafness gene shows a specific spectrum of mutations in Japan, including a frequent founder mutation. Hum Genet 2003; 112: 329–333.
Royaux IE, Wall SM, Karniski LP et al: Pendrin, encoded by the Pendred syndrome gene, resides in the apical region of renal intercalated cells and mediates bicarbonate secretion. Proc Natl Acad Sci USA 2001; 98: 4221–4226.
Scott DA, Wang R, Kreman TM et al: The Pendred syndrome gene encodes a chloride–iodide transport protein. Nat Genet 1999; 2: 440–443.
Ishinaga H, Shimizu T, Yuta A et al: Pendred's syndrome with goiter and enlarged vestibular aqueducts diagnosed by PDS gene mutation. Head Neck 2002; 24: 710–713.
Masmoudi S, Charfedine I, Hmani M et al: Pendred syndrome: phenotypic variability in two families carrying the same PDS missense mutation. Am J Med Genet 2000; 90: 38–44.
Hulander M, Kiernan AE, Blomqvist SR et al: Lack of pendrin expression leads to deafness and expansion of the endolymphatic compartment in inner ears of Foxi1 null mutant mice. Development 2003; 130: 2013–2025.
Acknowledgements
We thank all the subjects who participated in the present project. We also thank Dr Kyoko Nagai (Gunma University School of Medicine), Dr Satoshi Iwasaki (Hamamatsu University School of Medicine), Dr Tatsuo Matsunaga (International University of Health and Welfare), Drs Noriko Minami and Yumiko Hosoya (Iwate Medical University), Drs Hajime Ishinaga and Atsushi Yuta (Mie University), Dr Tetsuya Tono (Miyazaki Medical College), Dr Yukihiko Kanda (Nagasaki University School of Medicine), Dr Hitoshi Sato (Niigata University School of Medicine), Drs Tatsuhiko Harada and Ryuichi Osanai (Saitama Medical School), Drs Hitome Kobayashi and Yasuya Nomura (Showa University), and Dr Tatsuya Yamasoba (Tokyo University) for sending the samples of their patients. This work was supported by the Ministry of Health and Welfare, Japan (SU), and a Grant-in-Aid for Scientific Research from the Ministry of Education, Science and Culture of Japan (SU).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tsukamoto, K., Suzuki, H., Harada, D. et al. Distribution and frequencies of PDS (SLC26A4) mutations in Pendred syndrome and nonsyndromic hearing loss associated with enlarged vestibular aqueduct: a unique spectrum of mutations in Japanese. Eur J Hum Genet 11, 916–922 (2003). https://doi.org/10.1038/sj.ejhg.5201073
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ejhg.5201073
Keywords
This article is cited by
-
Enlarged vestibular aqueduct and Mondini Malformation: audiological, clinical, radiologic and genetic features
European Archives of Oto-Rhino-Laryngology (2021)
-
A novel genotyping technique for discriminating LVAS-associated high-frequency variants in SLC26A4 gene
AMB Express (2020)
-
Comprehensive genetic testing of Chinese SNHL patients and variants interpretation using ACMG guidelines and ethnically matched normal controls
European Journal of Human Genetics (2020)
-
Next-generation sequencing-based mutation analysis of genes associated with enlarged vestibular aqueduct in Chinese families
European Archives of Oto-Rhino-Laryngology (2020)
-
Mutation analysis of SLC26A4 (Pendrin) gene in a Brazilian sample of hearing-impaired subjects
BMC Medical Genetics (2018)