Key Points
-
Highlights the importance of early referral of patients whose sole presenting complaint is altered sensation/numbness.
-
Encourages taking a thorough past medical history at the initial consultation.
-
Emphasises the importance of always sending surgical specimens for histopathology.
Abstract
This paper reports a patient with a history of breast cancer, who presented with altered sensation to the right lower lip and chin. An orthopantomogram showed a probable dentigerous cyst associated with an unerupted lower wisdom tooth, which was closely related to the inferior dental canal. The tooth and cyst were enucleated under general anaesthesia. The subsequent histopathology report concluded that the cyst contained metastatic adenocarcinoma from a primary breast tumour.
Similar content being viewed by others
Clinical relevance
Metastases to the jaw are uncommon. This report highlights the importance for general dental practioners to take into consideration the presence of jaw metastases. This is particularly relevant in patients with a history of malignant disease presenting with atypical symptoms such as altered sensation of the lower lip. In such cases early referral may prove crucial.
Case report
A 44-year-old Caucasian female was referred to the maxillofacial department by her general dental practitioner. Her presenting complaint was that of a tingling sensation over her right lower lip, chin and gums. She reported that the symptoms had come on overnight approximately a year ago and had remained constant and unchanged since. There was no associated swelling, pain or displacement of teeth.
Points of relevance in the patient's medical history include that seven years previously she had been diagnosed as having breast cancer. She was treated with radiotherapy and chemotherapy, but despite treatment developed bony metastases. She was taking a variety of drugs, including Prednisolone.
Social history found the patient to be a heavy smoker. She reported that for the last 10 years she smoked on average 20 cigarettes a day. Her alcohol consumption was low, and she stated that she drank only occasionally.
Examination revealed patchy hypoaesthesia of the right lip and chin, and tenderness of the right submandibular lymph nodes. There was no evidence of local infection within the oral cavity.
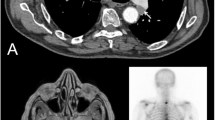
An orthopantomogram was taken (Fig. 1). This showed an unerupted horizontally impacted lower right wisdom tooth closely related to the inferior dental nerve canal. A unilocular radiolucent area associated with the crown of the tooth was noted and was felt to be compatible with the diagnosis of a dentigerous cyst.
However, the presence of altered sensation to the lower lip was of concern and arrangements were made to extract the lower right wisdom tooth and enucleate the associated cyst under general anaesthesia with appropriate steroid cover.
Surgery was uneventful and the cyst tissue was sent for histological examination. At operation the cyst lining was closely related to the inferior dental nerve. The microscopy report cited that: 'the cyst wall contained two areas of malignant acinar proliferation with moderate nucleur pleomorphism and tumour necrosis. The appearance was that of moderately differentiated adenocarcinoma with metastatic origin from a primary breast carcinoma. No vascular invasion was seen'. The conclusion was a metastatic adenocarcinoma arising in the wall of a dentigerous cyst.
The patient recovered well and is presently under review. The original complaint of hypoaesthesia to the lower right lip/chin has now resolved. Subsequent radiographs taken of the surgical site shows no signs of recurrence.
Discussion
This report highlights the importance of a thorough history and examination, especially in patients presenting with atypical symptoms such as altered sensation of the lip. Although the submandibular nodes were tender, there was no evidence of infection in relation to the wisdom tooth or cyst, which might have explained the patient's symptoms. The medical history was highly relevant, as the patient had a history of breast carcinoma with bony metastases. It also illustrates the importance of sending excised cystic tissue for histopathology.
Despite this, metastatic tumours of the jaw are uncommon and those to the oral mucosa are very rare.1 The exact incidence of jawbone metastases is difficult to assess accurately. This is because when assessing the extent of bony metastases in a patient, the jawbones are rarely included in any diagnostic tests, suggesting that the incidence could be more common than previously noted.2,3
Most metastatic primary tumours to the jawbone tend to be epithelial in origin,4 with adenocarcinomas being the most common.1
The sex distribution tends to be equal with a median age of 60 years.1 The most common primary sites for metastatic tumours to the jawbone in a female include: breast, adrenal, colo-rectum, female genital organs and the thyroid (listed in order of decreasing prevalence). In comparison, for men the most common primary sites include the lung, kidney, bone and adrenal (again listed in order of decreasing prevalence).4
The pathogenesis of the metastatic process in the jawbones is not clear, but as the distribution of metastatic spread to the jaw is uneven, it is unlikely to be a simple mechanical process. Bones with active marrow, such as the spine, ribs, skull, femur and humerus are the preferential sites for metastatic deposits. This is because they contain vascular spaces that are sinusoidal in nature and present a relatively easy barrier for tumour cells to penetrate.5,6 Furthermore the marrow contains growth factors and these may act to enhance colonisation of some metastatic tumours. In addition, inflammation has been shown to attract metastatic cells to an area.
Active bone marrow tends to be located in the posterior part of the mandible and maxilla explaining why metastatic tumours tend to be more prevalent in the molar and premolar area. The development and expansion of any cyst is complicated and involves growth factors and inflammatory mediators. This could help explain the presence of metastatic deposits in the dentigerous cyst lining.
References
Van der Waal R I F, Butler J, Van der Waal I . Oral Metastases: Report of 24 cases. Br J Oral Maxillofac Surg 2003; 41: 3–6.
Hatsiotis J C, Constantinidou H, Panayotou P H . Metastatic tumours of the oral soft tissues. Oral Surg Oral Med Oral Pathol 1973; 36: 544–550.
Okarinen V J, Calonius P E B, Sanio P . Metastatic tumours to the oral region. An analysis of cases in the literature. Proc Finn Dent Soc 1975; 71: 58–65.
Gardner A F . Metastatic neoplasms to the oral regions from distant primary sites. Calif State Dent Assoc 1964; 40: 498–503.
Hirshberg A, Leibovich P, Bochner A . Metastases to the oral mucosa: analysis of 157 cases. J Oral Pathol Med 1993: 22: 385–390.
Kricum M E . Red-yellow marrow conversion, its effect on the location of some solitary bone lesions. Skeletal Radiol 1985; 14: 10–19.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Chatterjee, M., Balaraman, K. & McDermott, P. Metastatic breast carcinoma discovered in a dentigerous cyst — a case report. Br Dent J 201, 349–350 (2006). https://doi.org/10.1038/sj.bdj.4814042
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4814042