Key Points
-
Provides an insight into how general anaesthetic extraction services for children have changed.
-
Shows that DGA extraction services are now more fully directed towards 'pre-cooperative' children.
-
Suggests that improved assessment and caries diagnosis has led to increased numbers of extractions.
-
Questions whether 'extraction' only services under general anaesthesia should ultimately be augmented by GA services that provide restorative treatment.
Abstract
Objective To report on the changing profile of children attending for Dental General Anaesthetic extractions (DGA) at the same centre in 1998 and again in 2004 compared to 1991.
Design Prospective clinical.
Setting Glasgow Dental Hospital DGA service during August 1999 and August/September 2004.
Subjects and method Children presenting for DGA extractions. Data recorded: age, gender, number of teeth extracted and level of behaviour using the Frankl scale.
Results In 1999: 190 children (97 boys) mean age five years. In 2004: 106 children (55 boys) mean age five years. There was a significant increase in the mean number of teeth extracted (p < 0.001), 4.2 (1-16) and 7.8 (1-17) in 1999 and 2004 respectively, compared to 3.7 in 1991. Twenty-six per cent of children had between six and 16 teeth extracted in 1999 compared to 74% in 2004. Significantly fewer children demonstrated 'definitely positive' behaviour compared to 1991. Children were in the poorest socioeconomic groups, reflecting the geographic area.
Conclusion Over half of the children were aged five years and under. Fewer highly co-operative children were treated. More teeth were extracted per child, suggesting that there should be greater opportunities to carry out restorations, not just extractions under general anaesthesia.
Similar content being viewed by others
Introduction
The Poswillo Report1 published in 1990, reported that general anaesthesia in the dental setting 'should be avoided wherever possible' and also concluded 'sedation should be used in preference to general anaesthesia'. High profile cases involving the deaths of children while under general anaesthesia for dental extractions (DGA) have led to the development of a number of key changes to the control of its use. In 1999, the General Dental Council2 placed the obligation on the referring general dental practitioner to give a clear justification for the use of general anaesthesia (GA), to explain the risks to the family, and to outline alternative methods of treatment. Moreover, the Royal College of Anaesthetists published guidance, particularly in respect of the appropriate level of training of an anaesthetist administering a GA for dental purposes, leading to a further restriction on the number of centres able to provide a DGA service.3 Following proposals by the Department of Health in A Conscious Decision (2000) the use of general anaesthesia in dentistry is now limited to the hospital setting.4
There is likely to always be a need for the use of GA in the dental treatment of children. As many as 55% of children in Scotland have experienced dental caries by five years of age, 5 and with dental registration rates being low, particularly in the most deprived communities,6 it is inevitable that by the time some of these children present for dental treatment they will already be in pain.
The guidelines for provision of DGA services have been continually changing but the impact of these changes upon the profile of the children referred for this type of treatment needs to be monitored. Have the changes led to fewer potentially co-operative children receiving an 'avoidable' DGA? It is clearly important to regularly review the characteristics of those children referred for DGA extractions. Grant et al.7 reported that the mean and modal age had decreased from 7.7 years to 6.0 years in 1989 and to 5.7 years and 4.0 years in 1997. Holt et al.8 reported that more teeth were extracted per child when they are referred via a specialist paediatric dentistry DGA assessment service.
Shortly after the publication of the Poswillo1 recommendations, Burns et al.9 (1992) reported that the mean age of the children referred for GA extractions at Glasgow Dental Hospital and School was five years, 60% co-operated positively or very positively with anaesthetic induction and that 40% of children had only one or two teeth removed. The authors concluded that the demand for DGA could be further reduced if it was reserved for those requiring multiple extractions.
The aim of this study was to report on the profile of children attending for DGA at Glasgow Dental Hospital and School in respect to their age, gender and number of teeth extracted and their level of co-operation at anaesthetic induction. Similar methodology to the study by Burns et al.9 was used to facilitate a comparison between post-GDC and post- A Conscious Decision. DGA patient cohorts attending the same DGA service.
Method
The local area dental ethics committee granted ethical approval in 1998 and again in 2004 for the recruitment of children at the time when they presented for DGA extractions at Glasgow Dental Hospital and School. Parents were approached in the DGA waiting room by a final year dental student (JB, PH) and invited to give their consent to participate in the study. Data were collected from consecutive children, service throughput permitting, during the month of August in 1999 (JB) and during August and September in 2004 (PH). The later extension into September 2004 was to augment the 2004 data sample since the DGA service provision had been reduced due to staffing shortages, resulting in fewer children being treated each week during August. The raw data from the 1991 study9 were available for statistical analysis (NB M.T. Hosey is M.T. Burns).
The age, gender and number of teeth extracted for each child was recorded and the behaviour of the children at anaesthetic induction was scored, using the Frankl Behaviour Scale,10 by the consultant anaesthetists in collaboration with the dental student. The Frankl Scale is commonly used as a selection tool in paediatric dental sedation studies.11 For the purpose of this study, DEPCAT (Deprivation Category) scores relating to the partial postcode of each child were obtained using the Carstairs Index.12 This index is often used in Scotland and is a scale of deprivation based on information collected in the national census every 10 years. It describes the social characteristics of those residents living in a particular postcode sector. DEPCAT scores are calculated based on the percentage of unemployed males, over-crowded households, households without cars and people from social classes IV and V. The scale ranges from DEPCAT 1 (most prosperous) to DEPCAT 7 (least prosperous).
Results
In 1999, a total of 190 children participated; there were 97 boys (51.5%) and 93 girls (48.5%), mean age 5.4 years (range 1-11 years). In 2004, 106 children participated; there were 55 boys (51.9%) and 51 girls (48.1%), mean age 5.3 years (range 3-10 years). The detailed comparisons with the 1991 study in respect to age, gender, deprivation category and number of teeth extracted are shown in Table 1
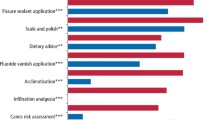
The mean number of teeth extracted in 1999 was 4.2 (median 3, range 1-16); in 2004 this had increased to 7.4 (median 8, range 1-17). This increase from 1991 was highly significant (p < 0.001), irrespective of whether means (one-way ANOVA) or medians (Kruskal-wallis) were used in the statistical analysis, and can be seen clearly in Figure 1. In 1999, 13% of children had one tooth extracted; 25% had two; 14% had three; 16% had four; 6% had five and 26% had between six and 16 teeth extracted. In 2004, 3% of children had one tooth extracted; 4% had two; 2% had three; 11% had four; 6% had five and 74% had between six and 16 teeth extracted.
The Frankl behaviour ratings for 1999 and 2004, compared to 1991 are shown in Table 2. The chi-squared test confirmed that there was a significant change in the behaviour of the children at anaesthetic induction (p < 0.001). In 2004, two patients did not cooperate sufficiently at the induction phase of treatment. These patients were referred to the Royal Hospital for Sick Children, Yorkhill so that treatment could be completed facilitated by pre-medication.
In relation to social status, there has been little change; in 2004, 89.6% were in the poorest socio-economic groups (DEPCAT 4-7) compared to 85.1% in 1999.
Discussion
The gender distribution of the children in 1991, 1999 and in 2004 remained similar, with almost equal numbers of boys and girls. The reduced number of children in the 2004 sample was due to reduction in the GA service provision due to staffing problems rather than a reduction in referrals. These problems continued into the extended sampling frame period (September). The mean age of children referred for DGA extractions remained the same, though this continues to be lower than comparable studies.7,8 Approximately half of the children treated have been aged five years and under; this is doubtless a reflection of the poor dental health of this population in Scotland. The eldest child in the 1999 sample was just 11 years old compared with 17 years old in 1991 and the youngest in 2004 was aged three years compared to one year of age previously. This reflected a change in policy in the DGA service where the cut-off age was lowered to age 11 years and, since the year 2000, those patients requiring dental treatment under general anaesthesia who are outwith the age range of 3-10 years old are referred to Royal Hospital for Sick Children, Yorkhill.
With regards to the level of social deprivation, it was found that the majority of patients lived in the most socially deprived areas (DEPCATS 4-7). There was little change between 1999 and 2004 (this information was not recorded by Burns et al. in 1991). Despite this, children from deprived areas are probably not more likely to need DGA; instead this finding reflects the link between high caries risk and social deprivation13 in the Glasgow Dental Hospital and School DGA service referral area.14
The mean number of teeth extracted per patient in 2004 was significantly higher than previous years. The 1999 and 2004 data were skewed so medians should be used, even though the 1991 study reported means only. Therefore, we used both medians and means and analysed them separately, but the high level of significance was unchanged. The need for multiple extractions has been cited as a principal reason for DGA referral.15 This might be a reflection of the more rigorous pre-operative assessment that is now performed. A better assessment process favours the use of alternatives to DGA such as local anaesthesia and sedation and the present study suggests that more children who need only one or two teeth removed now have this performed without recourse to DGA. However, referral via a specialist paediatric dentistry screening service also leads to an increased number of extractions,8 hopefully resulting in a reduction in the need for a repeat DGA. The use of pre-operative radiographs as part of the DGA assessment process was introduced at Glasgow Dental Hospital and School, before the 2004 study, to augment the assessment process and this obviously resulted in improved caries diagnosis. Therefore teeth, which in the past may not have been diagnosed as carious, are now extracted. This more radical approach to managing early childhood caries, when general anaesthesia is used as the last resort, is in accordance with British Society of Paediatric Dentistry policy.16 It has been reported that between 23% and 31% of children subsequently require a further DGA and children below four years of age have the highest risk of needing repeat referral.15 Harrison and Nutting (2000) suggested that the failure to extract minimally carious teeth at the child's first DGA visit might be founded in a misplaced optimism to save these teeth later even though this approach may have accounted for 85% of repeat DGA referrals. Instead, the authors suggested that more children could be offered restorations under general anaesthesia rather than extraction alone.17 The primary method of treating children with caries in the UK is by extraction,18 this is supported by a culture that does not recognise the importance of restoring the primary dentition, demonstrated by the low Care Index (8.7%) found in this geographic sample.19 Moreover, DGA extraction services are more widely available and cheaper than carrying out restorative treatment under general anaesthesia. Nevertheless, it could be argued that restoration as opposed to extraction of primary teeth, especially those with only radiographic evidence of dentinal caries, might be a better treatment option, especially in respect to maintenance of masticatory function and prevention of space loss.
In respect to behaviour at anaesthetic induction, significantly fewer children in both 1999 and 2004 demonstrated 'definitely positive' behaviour compared to 1991. This suggests that the most highly co-operative children are no longer referred for DGA. However, it should be borne in mind that good behaviour at induction might not translate into co-operation for dental procedures under local anaesthesia. Moreover, the Frankl scale, though simple to administer and widely used, is a relatively crude behavioural measurement tool11 and different dental researchers were involved with the data collection at each time point, though all three studies had the same lead researcher (MTH). In 2004, 66% of children displayed 'positive' behaviour, higher than in 1999 and 1991 (63% and 46% respectively). There are several possible reasons for this. Firstly, this could be a limitation of the Frankl scale with insufficient sensitivity between 'positive' and 'definitely positive'. Secondly, improvements to the DGA service in respect to both the preparation of the children by the nursing staff and to the creation of a more child-friendly environment, may have resulted in the children in the 1999 and 2004 samples coping better with the DGA induction. In 1991, the parents were not allowed to accompany their child into the DGA theatre and no doubt the adverse behaviour in some of the younger children at that time was due to separation anxiety.20 This policy had changed by 1999; parents are now routinely invited to support their child during the anaesthetic induction. The two children who did not demonstrate sufficient cooperation at the induction stage of treatment in 2004 required pre-medication, supporting the results of a recent audit that reported that 1.37% of children refuse induction.21
Conclusion
This study suggests that DGA extraction referrals of potentially co-operative children have reduced and that the number of teeth extracted in each child has increased. Over half of the children are aged five years and under. Perhaps these 'pre-cooperative' children should have a greater opportunity for tooth restoration rather than extraction under general anaesthesia.
References
Poswillo DE . General anaesthesia, sedation and resuscutation in dentistry. Report of an expert working party prepared for the Standing Dental Advisory Committee. London, 1990.
General Dental Council. Maintaining standards. Guidance to dentists on professional and personal conduct. 1997; modified May 1998.
The Royal College of Anaesthetists. Standards and guidelines for general anaesthesia for dentistry. London, 1999.
Department of Health. A Conscious Decision. 2000.
Scottish Executive. Towards better oral health. 2002.
Pavi E, Kay EJ, Stephen KW . The effect of social and personal factors on the utilisation of dental services in Glasgow, Scotland. Comm Dent Health 1995; 12: 208–215.
Grant SM, Davidson LE, Livesey S . Trends in exodontia under general anaesthesia at a dental teaching hospital. Br Dent J 1998; 185: 347–352.
Holt RD, Al lamki S, Bedi R et al. Provision of DGA for extractions in child patients at two centres. Br Dent J 1999; 187: 498–501.
Burns MT, Blinkhorn AS, Asbury AJ . An evaluation of the behaviour of children undergoing dental extraction under general anaesthesia. Anaesthesia 1992; 47: 1073–1074.
Frankl SN, Shiere FR, Fogels HR . Should the parent remain with the child in the dental operatory? J Dent Child 1962; 2: 150–163.
Hosey MT, Blinkhorn AS . An evaluation of four methods of assessing the behaviour of anxious child dental patients. Int J Paed Dent 1995; 5: 87–95.
McLoone P . Carstairs Scores for Scottish Postcode Sectors from the 1991 Census. Glasgow: Public Health Resource Unit, University of Glasgow, 1994.
Pitts NB . Inequalities in children's caries experience: the nature and size of the UK problem. Comm Dent Health 1998; Suppl 1: 296–300.
Sweeney PC, Nugent Z, Pitts NB . Deprivation and dental caries status of 5 year old children in Scotland. Comm Dent Oral Epid 1999; 2: 152–159.
MacCormac C, Kinirons M . Reasons for referral of children to a general anaesthetic service in Northern Ireland. Int J Paed Dent 1998; 8: 191–196.
British Society of Paediatric Dentistry: a policy document on oral health care in preschool children. Int J Paed Dent 2003; 13: 279–285.
Harrison M, Nutting L . Repeat general anaesthesia for paediatric dentistry. Br Dent J 2000; 189: 37–39.
Bolin AK . Children's dental health in Europe. An epidemiological investigation of 5- and 12-year old children in eight EU countries. Swedish Dent J 1997; 122:1–88.
Pitts NB, Nugent ZJ, Smith PA . Scottish Health Board's Dental Epidemiological Programme. Report of the Survey of 5-year old children. Dental Services Research Unit, University of Dundee, 1999/2000.
Guthrie A . Separation anxiety: an overview. Ped Dent 1997; 19: 486–490.
Sood S, Campbell C, Hosey MT . What happens to children who refuse dental GA induction? Abstract 20. Int J Paed Dent 2003; 13: 389.
Acknowledgements
The authors would like to thank the anaesthetists, the dental surgeons and the nursing staff of the Department of Oral Surgery at Glasgow Dental Hospital and School for their help with this project.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Hosey, M., Bryce, J., Harris, P. et al. The behaviour, social status and number of teeth extracted in children under general anaesthesia: A referral centre revisited. Br Dent J 200, 331–334 (2006). https://doi.org/10.1038/sj.bdj.4813347
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4813347
This article is cited by
-
Do paediatric patient-related factors affect the need for a dental general anaesthetic?
British Dental Journal (2022)
-
Providing sealants at the general anaesthetic assessment visit for children requiring caries-related dental extractions under general anaesthetic: a pilot randomised controlled trial
British Dental Journal (2021)
-
A rapid review of variation in the use of dental general anaesthetics in children
British Dental Journal (2020)
-
Socioeconomic and ethnic status of two- and three-year-olds undergoing dental extractions under general anaesthesia in Wolverhampton, 2011-2016
British Dental Journal (2019)
-
Post-operative pain and morbidity in children who have tooth extractions under general anaesthesia: a service evaluation
British Dental Journal (2019)