Key Points
-
Provides evidence that smoking is a major risk factor in the progression of periodontitis.
-
Only 6% of referred patients are aware of the damage smoking causes to their periodontal health.
-
Emphasises the undervalued role of dental practitioners in providing smoking cessation counselling to their patients.
-
Highlights the ineffectiveness of public health campaigns in educating patients that smoking increases the risks of their teeth 'falling out' by more than 300%.
Abstract
Objective To investigate patients' knowledge of the effects of smoking on periodontal health.
Design Patient answered questionnaires, which were anonymous.
Setting Patients who attended GKT Dental Institute, King's College, London for dental treatment.
Subjects One thousand patients attending Restorative Consultant Clinics and Primary Dental Care
Results Seventy-eight per cent of patients were aware that smoking had a negative impact on health. However, 52% of these patients who were aware could not state what the negative effects were on oral health. Seven per cent of patients stated that smoking affected the gums but did not state how it affected the gums. Only 6% of respondents knew specifically of the link between smoking and periodontal disease. The only statistically significant factors associated with increased awareness were smoking status, ie being a non-smoker and being registered with a general dental practitioner. Non-smokers and those registered with GDPs were more likely to be aware of the association between smoking and periodontal diseases.
Conclusions This study highlights patients' lack of awareness of the relationship between smoking and periodontal diseases, with only 6% of respondents knowing of the link between tobacco and periodontal diseases.
Similar content being viewed by others
Main
A WHO report released in early 2004 stated that oral diseases such as periodontitis are a global health issue in both industrialised and increasingly in developing countries. It is a particular problem amongst poorer communities. The report went on to say that 'globally, most children show signs of gingivitis and among adults, the initial stages of periodontal disease are prevalent. Severe periodontitis, which may result in tooth loss, is found in 5-15% of most populations.'
It is well known that smoking is a significant risk factor for periodontal disease and many studies have confirmed this. This study assessed patients' knowledge of the effects of smoking on the periodontal tissues. It was implemented following an observation by the restorative team at King's College of the lack of knowledge of the relationship between smoking and periodontal diseases. Patient answered questionnaires were devised and 1,000 completed questionnaires were collated. The results were statistically analysed. Only 7% of respondents stated that they were aware that tobacco affected the periodontal tissues in some way, but did not specifically write 'gum disease'. Only 6% of respondents knew of the link between tobacco and periodontal disease. The only statistically significant factors that were associated with increased awareness were smoking status ie being a non-smoker and being registered with a general dental practitioner (GDP).
Background
It was observed that patients, referred by their general dental practitioners (GDPs) to a restorative consultant clinic, lacked awareness of the relationship between smoking and periodontal diseases. It was perceived that GDPs might not be relaying this essential information to their patients in an effective way. It was decided that an investigation should be conducted to assess a sample of 1,000 patients for their level of awareness of the effects of smoking on oral health and, in particular, on periodontal diseases.
A prospective investigation was conducted over a three month period from September to November 2003, which involved questionnaires being completed by referred patients attending clinics for restorative treatment. These anonymous questionnaires asked them about their awareness of the oral/dental effects of smoking as well as enquiring about their age, gender and ethnic origins. The questions included whether patients were registered with a GDP and if they smoked. If the patient had ceased smoking, they were asked for their reasons and timing for this. Ethical approval was deemed unnecessary by King's College Hospital Research Ethics Committee. The aim was to obtain 1,000 completed questionnaires and analyse the data for any trends.
Statement of the problem
Periodontal diseases can affect the quality of life of patients by affecting the function of the dentition and the dental appearance. It can also lead to the loss of teeth in susceptible patients. Smoking has long been known to be a strong risk factor for periodontal diseases resulting in accelerated onset, severity and progression of the disease1,2 partly by creating a more favourable habitat for periodontal pathogens.3
In susceptible patients, the clinical effects of smoking are dependent on the number of cigarettes smoked daily and the duration of the habit.4 The consequences may involve the vascular effect of nicotine5 and the enhanced production of inflammatory cytokines.6 It has been reported that smokers respond less well to periodontal therapy7,8,9 and this may be related to the fact that smoking compromises periodontal ligament (PDL) cell adhesion to root planed surfaces, resulting in the decreased likelihood of regeneration.10
Nicotine has cytotoxic effects on periodontal ligament fibroblasts.11 It also has inhibitory effects on periodontal cell proliferation and protein synthesis which result in impaired wound healing.11 Smoking results in changes to vascular,12 inflammatory,13,14 immune15 and healing responses.10,11 There is considerable scientific evidence of its harmful long term effects on periodontal diseases.16
Grossi et al.17,18 stated that the odds ratio of smokers developing adult periodontitis was greater than the relationship between periodontitis and the gram-negative anaerobic bacteria that causes this.
In spite of this overwhelming evidence, patients attending these consultant clinics often seemed genuinely surprised that they had not been informed of the adverse impact of smoking on their periodontal health.
Method
This prospective study was conducted from September to November 2003 at King's College Dental Institute, Denmark Hill Campus by the use of anonymous, patient completed, questionnaires. These were distributed by members of staff to the patients attending consultant clinics and were completed in the waiting room. Once completed the questionnaires were returned immediately. Two pages of mainly close-ended questions with options in simple English (Table 1) were completed by these patients. The only open ended questions were (1) the number of cigarettes smoked, (2) the number of years the patient had smoked, (3) their knowledge about how smoking or using tobacco affects the inside of the mouth and (4) if they used just cigarettes or any other form of tobacco (pipes, cigars etc). The personal details included were age, gender and ethnic group.
Results
Univariate analysis was used to assess the association of each variable with awareness. The association with the categorical variables was examined with chi-square test (Pearson, Fisher's exact test or trend); for continuous variables t-test or Mann-Whitney tests were used, as appropriate. In a second step multiple logistic regression was undertaken to see the combined association of all the variables.
Profile of the respondents (Table 2)
There were 1,071 respondents. The mean age was 38 (95% c.i. 36.9, 38.6) and 49% were male. The majority of the sample were either White British (37%), Black Caribbean (24%) or Black African (14%). Only 60% of the respondents were registered with a GDP. A total of 463 (43%) respondents were current smokers. The mean duration of smoking was 16 years (95% c.i. 14.5, 16.6) for this group, with a mean daily number of smoked cigarettes/cigars/marijuana of 12 (95% c.i. 10.8, 12.2). Of these, 93% smoked cigarettes, 9% marijuana and 3% smoked cigars. Some smokers used a combination of two or three of these options. One hundred and forty-seven non-smokers were past smokers, comprising 14% of the overall sample. The mean period of time elapsed since smoking cessation was 10 years (95% c.i. 8.1, 11.5). Forty-six per cent of ex-smokers stopped for reasons other than medical and financial.
Patient awareness that tobacco affects oral/dental health (Table 3)
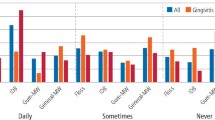
Seventy-eight per cent (832) of the total sample were aware that tobacco affects oral health. A univariate statistical analysis showed there to be no significant association between gender and awareness of tobacco on the effects oral health (p = 0.75); the proportion was similar for males and females (78%). Overall, the level of awareness was similar in all ethnic groups. Minor differences between the ethnic groups did not reach statistical significance.
In contrast to the demographic characteristics, there was a very significant association between being registered with a GDP (p = 0.0001) and smoking status ie whether they were smokers or non-smokers (p = 0.04) of respondents being aware that tobacco affects oral health. While 82% of the registered patients were aware of the association, only 71% of the unregistered were. Seventy-five per cent of the smokers were aware of this association, but in the non-smoking group 80% were. There were no significant differences between what was smoked (cigarettes, cigars, pipes or marijuana) and being aware that smoking affected oral health. This may be due to the small numbers of respondents that smoke pipes and cigars.
Eighty-two per cent of people who had ceased smoking believed tobacco affects oral health. There was a significant association between 'reason to quit' and being aware of tobacco affecting oral health (p = 0.03). Within the smoking cessation group, 34% had stopped for medical and 17% had ceased for financial reasons.
In a multiple logistic regression model that adjusts for all the variables, only smoking status and being registered with a GDP retained statistical significance. Age, sex and ethnic origin did not show any statistical significance. The odds of awareness for patients that were registered were approximately double those that were not registered (OR = 1.8, 95% c.i. 1.4 - 2.4; p = 0.0001). The odds of awareness for non-smokers were 50% higher than those for smokers (OR = 1.5; 95% c.i. 1.11 - 2.0).
Manner in which tobacco is believed to affect oral and dental health (Table 4)
Seventy-eight per cent of patients were aware that smoking had a negative impact on health. Fifty-two per cent of these patients could not state any negative effects.
Seven per cent of respondents stated that they were aware that smoking affected the gums but did not specifically write 'gum disease'. Only 6% of respondents knew of the link between tobacco and gum disease. Despite multiple and expensive oral cancer public awareness campaigns, it was disappointing that 12% of respondents stated that they were aware of the risks of oral cancer. Twenty-seven per cent gave stained teeth as an effect of smoking and 13% were conscious of halitosis, both of which are more of a social/cosmetic concern rather than a health risk. Over half (52%) were aware of some oral health issues but did not know how smoking affects oral health. The remaining reasons given were decay (2%), ulceration (2%), altered taste (2%) and impaired healing (1%).
Discussion
Our study showed two factors which led to an increased awareness about the oral problems caused by smoking: when the respondents were non-smokers and when they were registered with a GDP. In this study the odds of awareness for non-smokers were 50% higher than the odds of awareness for smokers (OR = 1.5; 95% c.i. 1.11 to 2.0). The odds of awareness for those that were registered with a GDP relative to those that were not registered were almost double (OR = 1.8, 95% c.i. 1.4 to 2.4). Respondents registered were more aware that tobacco has a negative effect on oral health. This suggests that non-smokers are perhaps more health conscious, and possibly because of this knowledge are less likely to start smoking and that having a GDP to impart appropriate information is important. Conversely, smokers were apparently less aware and maybe because of this lack of knowledge were less likely to stop.
This study highlights a general lack of awareness between smoking and periodontal diseases with only 6% of respondents knowing of this link. Seven per cent of respondents that were aware stated that smoking had a negative impact on periodontal health but were unable to state how. Of those patients that were aware, over half could not state what the negative effects were on oral/dental health. The fact that only 7% stated that smoking affected the gums and 6% stated specifically that smoking caused periodontal diseases should be of considerable concern in view of the devastating consequences of smoking.
Out of 56 million people, 13 million people smoke in Britain, of whom some 8 million apparently want to stop and 4 million make at least one attempt to do so each year.19 This leads to about 120,000 smokers, representing 1% of the total, allegedly stopping each year. In the UK, greater than 120,000 people die each year from smoking related diseases; which is equivalent to one in five deaths recorded.19 The adverse effects of smoking on periodontal disease progression is not understood by the vast majority of patients.
Relationship between smoking and periodontal disease
There are wide ranging and well publicised guidelines for the promotion of smoking cessation by health care professionals, in order to combat the adverse impact smoking has on the population's health. Sadly, it still seems to be poorly recognised by patients that one of the main risk factors in periodontal disease progression is smoking.
Many studies have been undertaken to highlight the link between smoking and periodontal diseases,20,21 with many authors stressing that the effects on periodontal diseases and periodontal therapy are heavily influenced by smoking. The NHANES (National Health and Nutritional Examination Survey) III study (2000) in the United States,16 reported that approximately 40% of periodontitis cases (6.4 million cases in the US adult population) were attributable to patients' smoking habits with a further 10% (1.7 million cases) being attributable to former smoking. This equates to half of these adult periodontitis cases being associated with a smoking habit. Among current smokers, approximately 75% of their periodontitis was attributed to smoking.16 The extent of periodontal diseases within this population appears to be largely due to this addictive risk factor. The data from NHANES III showed that smokers were four times more likely to have periodontitis. Furthermore, the greater the number of cigarettes smoked, the greater the probability of suffering from periodontitis,16,22 emphasising a dose-response relationship. Former smokers were 1.7 times more likely to have periodontitis than 'never smokers' with their risk continuing to reduce the longer they had abstained from smoking. It appears that former smokers had an intermediate risk status between current smokers and non-smokers. In terms of periodontal treatment there was a poorer prognosis for treatment success especially when periodontal surgery was carried out on smokers.9
Ismail1 and Haber et al.20 drew attention to the dose-response relationship between smoking and periodontitis-positive patients (ie the more smoked the more severe the periodontitis). These authors found that heavy smokers were 14.4 times more likely to suffer from periodontitis than non-smokers, with light smokers only 3.4 times more likely to have this problem. Other studies have highlighted smoking as a significant risk factor for the development of early onset periodontitis.23
It has long been acknowledged that acute necrotising ulcerative gingivitis (ANUG, AUG, Vincent's disease, trench mouth) is mostly found in smokers.24 Of even greater clinical importance to patients and oral health practitioners is that up to 90% of cases of refractory periodontitis cases are found in smokers13,25 with most refractory patients being heavy smokers.13 Refractory periodontitis is defined as periodontitis having a poor response to treatment despite the patient having good plaque control. Smoking cessation is therefore recommended prior to periodontal therapy.26
As long ago as 1983, Ismail et al.1 found that smoking and poorer levels of oral hygiene were linked. They acknowledged that while poor interdental oral hygiene remained an important factor in the onset of periodontitis, smoking appeared to be directly related to periodontitis, independent of other factors such as age, sex, race, oral hygiene or socio-economic status.27,28
Salvi et al.27 concluded that smoking was an independent risk factor for periodontitis, with cigarette smokers more than five times more likely to develop severe periodontitis than non-smokers. The level of risk was proportional to the number of pack-years (pack-years refers to the number of packs per week multiplied by 52 multiplied by the number of years of smoking). Other studies reported that about half of those suffering from periodontitis under the age of 33 had 'smoking induced disease'. The risk ratio for the presence of periodontitis and smoking being equal or greater than 14.29
Smoking is associated with alveolar bone loss. Jansson and Lavstedt30 showed a positive correlation with smoking and marginal bone loss, with former smokers having less bone loss than those who had carried on smoking during the 20 year study period. In a 10 year prospective study, Bergstrom, Eliasson and Dock31 showed that smoking was associated with an increase in periodontal pocketing with bone loss, compared with non-smokers and former smokers where periodontal health remained approximately the same over the 10 year study period. These studies illustrate a dose-response relationship and highlight the benefits of smoking cessation.
Smokers and their dentists, however, may not recognise the early symptoms of periodontitis due to the vasoconstrictive effect of nicotine, which effectively masks gingival inflammation. Increased calculus deposition has been noted in smokers32 and this in itself has been blamed for increased risk of periodontitis due to its plaque retaining features. It has been noted that attachment loss is usually more severe in the maxillary palatal regions.33,34 This would make sense because this is where the smoke first makes contact with the periodontal tissues.
Smokeless tobacco users, while a minority, also risk inducing oral health complications. Localised gingival recession and attachment loss at specific sites have been attributed to the use of chewable tobacco products.27,35 There is also a link between smokeless tobacco with leukoplakia35,36 and oral carcinomas.37
No differences in periodontal indices could be found between periodontitis sufferers and the method of smoking.1,38 Many smokers of cigars and pipes seem to feel that because the smoke is not inhaled it is fundamentally 'safer'. They seem to be unaware of the effects that strong unfiltered tobacco smoke has on the health of their oral tissues. This might be of less significance in prevalence terms, in the authors' opinion, because of the alleged decrease in the popularity of cigars and pipes in some societies.
Smoking cessation advice
It has long since been recognised that dental health professionals have a key role in educating and informing their patients about the health risks of smoking and also supporting smokers in the cessation of this habit. The importance of dentists and their teams in terms of advising and supporting their patients in smoking cessation is considerable due to the relative regularity of patient-dentist contact. Practitioners' roles should be to help to identify those patients who would like to stop smoking and refer them to specialist smoking cessation advice centres.
Although many dentists believe in the importance of helping their patients to quit or reduce smoking,39 unfortunately, there are barriers to this occurring effectively. These barriers may include insufficient time to provide this help (especially when this valuable time is not remunerated), lack of training or possibly a fear of interfering with the dentist-patient relationship.40,41,42
In recent research43 that looked at dentists' attitudes and practices with regard to smoking cessation from 1996-2001, 50% of dentists wanted more training in smoking cessation advice. A majority believed that dentists should encourage smokers to give up their smoking habit.43 The same study also highlighted the fact that dentists are much more likely to discuss smoking with patients with poor periodontal status than those with no major oral health problems, with 60% of dentists thinking that oral health problems were of major importance in motivating patients to stop smoking. Our study showed a lack of awareness in patients of the effects of smoking on the periodontal tissues in both smokers and non-smokers. A health awareness programme should, therefore, tackle both smokers and non-smokers. Targeted education should lead to a lot more people knowing about the effects of smoking on the probability of losing their teeth due to periodontitis. For example, non-smokers may know friends/ relatives who are smokers and might well be able to relay this important information to them in a supportive, non-critical, persistent, and, perhaps, more effective way.
A model which is useful for helping patients to stop smoking in the dental environment is known as the 'four As' which are Ask, Advise, Assist and Arrange follow-up.44 That is Ask about smoking at every opportunity, Advise smokers to stop, Assist the smokers in stopping (setting a quit date, recommending support from GPs, referral to specialist cessation service and use of Nicotine Replacement Therapy) and Arranging a follow-up appointment.
There are two main approaches for smoking cessation: counselling and pharmacotherapy. Specific medication eg bupropion (Zyban) may increase the abstinence rate to approximately 30%. Nicotine replacement therapy (NRT) has been shown to double the chances of quitting.45 It is important for those involved in smoking cessation advice to have a good knowledge of NRTs available. One study46 showed that less than 10% of dentists reported a good knowledge of NRT or Bupropion (Zyban). Therefore, a lack of training/education may be the most significant barrier.
NICE guidelines recommend that NRT or bupropion should be prescribed only for a smoker who commits to a quit date. The initial supply of smoking cessation therapy should be sufficient to last only for two weeks after the quit date. Only if the smoker demonstrates a continuing attempt to stop smoking can a second prescription be issued. However, if the attempt to quit is unsuccessful, the NHS would not normally fund a further attempt within six months. There is currently insufficient evidence to recommend the combined use of nicotine replacement therapy and bupropion.
One study47 investigated patients' views regarding dentists' smoking cessation advice showed that most patients (61%) would not change dentists if questioned about their smoking status regularly. This could allay any fears dentists might have of alienating patients or interfering with the dentist-patient relationship. This study demonstrated a reluctance among dentists to provide smoking cessation advice, with sadly few patients recalling any advice given to them in this regard.
Smith et al.'s48 study showed that within a general practice setting, a smoking cessation rate of 11% was achieved. Consideration should be given to adequately recognising and remunerating the dental team in this essential task, rather than simply rewarding them for undertaking just mechanical periodontal therapy and reinforcing oral hygiene with effective interdental brushes. All three of these aspects deserve recognition and appropriate remumeration.
The incidence of oral cancer in the UK in 2000 was 4,374.49 While this is a serious condition, it is rare. Conversely, it has been estimated that between 10-20% of the population are affected by severe forms of periodontal disease.50 Therefore 12 million people in the UK are likely to be affected by periodontal diseases. From a statistical viewpoint, very many more patients will be affected by periodontitis than will ever be affected by oral cancer. Public health campaigns and dental teams must continue to inform patients of the well established risks of smoking in relation to periodontal diseases.
References
Ismail AI, Burt BA, Eklund SA . Epidemiologic patterns of smoking and periodontal disease in the United States. J Am Dent Assoc 1983; 106: 617–621.
Amarasena N, Ekanayaka AN, Herath L, Miyazaki H . Tobacco use and oral hygiene as risk indicators for periodontitis. Comm Dent Oral Epidemiol 2002; 30: 115–123.
Eggert FM, McLeod MH, Flowerdew G . Effects of smoking and treatment status on periodontal bacteria: evidence that smoking influences control of periodontal bacteria at the mucosal surface of the gingival crevice. J Periodontol 2001; 72: 1210–1220.
Calsina G, Ramon JM, Echeverria JJ . Effects of smoking on periodontal tissues. Clin Periodontol 2002; 29: 771–776.
Mavropoulos A, Aars H, Brodin P . Hyperaemic response to cigarette smoking in healthy gingiva. J Clin Periodontol 2003; 30: 214–221.
Giannopoulou C, Kamma JJ, Mombelli A . Effect of inflammation, smoking and stress on gingival crevicular fluid cytokine level. J Clin Periodontol 2003; 30: 145–153.
Grossi SG, Zambon J, Machtei EE et al. Effects of smoking and smoking cessation on healing after mechanical periodontal therapy. J Am Dent Assoc 1997; 128: 599–607.
Grossi S, Skrepcluski F, DeCaro T et al. Response to periodontal therapy in diabetes and smokers. J Periodontol 1996; 67: 1094–1102.
Scabbia A, Cho KS, Sigurdsson TJ et al. Cigarette smoking negatively affects healing response following flap debridement surgery. J Periodontol 2001; 72: 43–49.
Gamal AY, Bayomy MM . Effect of cigarette smoking on human PDL fibroblasts attachment to periodontally involved root surfaces in vitro. J Clin Periodontol 2002; 29: 763–770.
Chang YC, Huang FM, Tai KW et al. Mechanisms of cytotoxicity of nicotine in human periodontal ligament fibroblast cultures in vitro. J Periodontal Res 2002; 37: 279–285.
Baab DA, Oberg PA The effect of cigarette smoking on gingival blood flow in humans. J Clin Periodontol 1987; 14: 418–424.
MacFarlane GD, Herzberg MC, Wolff LF, Hardie NA . Refractory periodontitis associated with abnormal polymorhonuclear leukocyte phagocytosis and cigarette smoking. J Periodontol 1992; 63: 908–913.
Seow WK, MacFarlane GD, Thong YH, Herzberg MC . Nicotine effects on PMN chemotaxis and phagocytosis. J Dent Res 1992: 71: 178.
Costabel U, Bross KJ, Reuter C et al. Alterations in immunoregulatory T-cell subsets in cigarette smokers. A phenotypic analysis of bronchoalveolar and blood lymphocytes. Chest 1986; 90: 39–44.
Tomar SL, Asma S . Smoking-attributable periodontitis in the United States: Findings from NHANES III. J Periodontol 2000; 71: 743–751.
Grossi SG, Zambon JJ, Ho AW . et al. Assessment of risk for periodontal disease. I. Risk indicators for attachment loss. J Periodontol 1994; 65: 260–267.
Grossi SG, Genco RJ, Machtei EE et al. Assessment of risk for periodontal disease. II. Risk indicators for alveolar bone loss. J Periodontol 1995; 66: 23–29.
Department of Health. www.doh.gov.uk Accessed 1 December 2003.
Haber J, Wattles J, Crowley M et al. Evidence for cigarettes smoking as a major risk factor for periodontitis. J Periodontol 1993; 64: 16–23.
Stoltenberg RL, Osborn JB, Pihlstrom BL et al. Association between cigarette smoking, bacterial pathogens, and periodontal status. J Periodontol 1993; 64: 1225–1230.
Tonetti MS . Cigarette smoking and periodontal diseases: etiology and management of disease. Annals of Periodontol 1998; 3: 88–101.
Koertge TE, Gunsolley C, Lake K, Schenkein H . Prevelence of smoking in early onset periodontitis subjects. J Dent Res 1994; 73: 187.
Kowolik MJ, Nisbet T . Smoking and acute ulcerative gingivitis. Br Dent J 1983; 154: 241–242.
Bergstrom J, Blomlof L . Tobacco smoking major risk factor associated with refractory periodontal disease. J Dent Res 1992; 71: 297.
Haber J . Smoking is a major risk factor for periodontitis. Current Opinion Periodontol 1994; 12–18.
Salvi GE, Lawrence HP, Offenbacher S, Beck JD . Influence of risk factors on the pathogenesis of periodontitis. Periodontol 2000 1997; 14: 173–201.
Page RC, Beck JD . Risk assessment for periodontal diseases. Int Dent J 1997; 47: 61–87.
Linden GJ, Mullally BH . Cigarette smoking and periodontal destruction in young adults. J Periodontol 1994; 65: 718–723.
Jansson L, Lavstedt S . Influence of smoking on marginal bone loss and tooth loss – a prospective study over 20 years. J Clin Periodontol 2002; 29: 750–756.
Bergstrom J, Eliasson S, Dock J . A 10-year prospective study of tobacco smoking and periodontal health. J Periodontol 2000; 71: 1338–1347.
Bergstrom J . Tobacco smoking and supragingival dental calculus. J Clin Periodontol 1999; 26: 541–547.
van der Weijden G A, de Slegte C, Timmerman M F, van der Velden U . Periodontitis in smokers and non-smokers: intra-oral distribution of pockets. J Clin Periodontol 2001; 28: 955–960.
Haffajee AD, Socransky SS . Relationship of cigarette smoking to attachment level profiles. J Clin Periodontol 2001; 28: 283–295.
Robertson PB, Walsh M, Greene J et al. Periodontal effects associated with the use of smokeless tobacco. J Periodontol 1990; 61: 438–443.
Creath CJ, Cutter G, Bradley DH et al. Oral leukoplakia and adolescent smokeless tobacco use. Oral Surg Oral Med Oral Pathol 1991; 72: 35–41.
Wray A, McGuirt F . Smokeless tobacco usage associated with oral carcinoma. Incidence, treatment, outcome. Arch Otolaryngol Head Neck Surg 1993; 119: 929–933.
Albandar JM, Streckfus CF, Adesanya MR, Winn DM . Cigar, pipe, and cigarette smoking as risk factors for periodontal disease and tooth loss. J Periodontol 2000; 71: 1874–1881.
Newton JT, Palmer RM . The role of the dental team in the promotion of smoking cessation. Br Dent J 1997; 182: 353–355.
Campbell HS, Macdonald JM . Tobacco counselling among Alberta dentists. J Can Dent Assoc 1994; 60: 223–226.
O'Keefe J, Lessio A, Kassirer B . A pilot smoking cessation program involving dental offices in the borough of East York, Ontario: an initial evaluation. J Can Dent Assoc 1995; 61: 65–67.
Gussy M, Newton JT, Palmer RM . The role of dental hygienists in the promotion of smoking cessation. Dental Health 1996; 35: 5–8.
John JH, Thomas D, Richards D . Smoking cessation intervention in the Oxford region: changes in dentists' attitudes and reported practices 1996-2001. Br Dent J 2003; 195: 270–275.
Lichtensein E, Wallack L, Pechacek TF . Introduction to the community intervention trial for smoking cessation (COMMIT). Community Health Educ 1990; 11: 173–185.
Imperial Cancer Research Fund General Practice Study Group. Randomised trial of nicotine patches in general practice: results at one year. Br Dent J 1993; 308: 1476–1477.
Clarke NG, Hirsch RS . Personal risk factors for generalized periodontitis. J Clin Periodontol 1995; 22: 136–145.
Rikard-Bell G, Donnelly N, Ward J . Preventive dentistry: what do Australian patients endorse and recall of smoking cessation advice by their dentists. Br Dent J 2003; 194: 159–164.
Smith SE, Warnakulasuriya KAAS, Feyerabend C et al. A smoking cessation programme conducted through dental practices in the UK. Br Dent J 1998; 185: 299–303.
Acknowledgements
The authors would like to acknowledge the assistance of Nora Donaldson and Chris Luca in the execution of this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Lung, Z., Kelleher, M., Porter, R. et al. Poor patient awareness of the relationship between smoking and periodontal diseases. Br Dent J 199, 731–737 (2005). https://doi.org/10.1038/sj.bdj.4812971
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4812971
This article is cited by
-
State-sponsored dental terrorism?
British Dental Journal (2017)
-
Opinions of Romanian Dental Students Toward Tobacco Use Interventions in the Dental Setting
Journal of Cancer Education (2016)
-
“I have never experienced any problem with my health. So far, it hasn’t been harmful”: older Greek-Australian smokers’ views on smoking: a qualitative study
BMC Public Health (2015)
-
Patients’ awareness of the potential benefit of smoking cessation. A study evaluating self-reported and clinical data from patients referred to an oral medicine unit
Clinical Oral Investigations (2012)
-
Patients' knowledge and views about the effects of smoking on their mouths and the involvement of their dentists in smoking cessation activities
British Dental Journal (2009)