Key Points
-
Neurofibromatosis type 1 is one of the most common genetic diseases and oral manifestations of this disease are extremely common.
-
Dentists should be aware of the characteristics of this disease.
-
It is important that dentists conduct longterm follow-up because of the potential for local complications and the known risk of malignant tumours.
Abstract
The term neurofibromatosis (NF) is used for a group of genetic disorders that primarily affect the cell growth of neural tissues. Neurofibromatosis type 1 (NF1), also known as von Recklinghausen's disease, is the most common type of NF and accounts for about 90% of all cases. It is one of the most frequent human genetic diseases, with a prevalence of one case in 3,000 births. The expressivity of NF1 is extremely variable, with manifestations ranging from mild lesions to several complications and functional impairment. Oral manifestations can be found in almost 72% of NF1 patients. A case of a NF1 patient with a gingival neurofibroma in the attached gingiva of the lingual aspect of the lower central incisors is presented. The lesion was nodular, with sessile base, non-ulcerated, non-painful, with normal colour and measured 1 cm in diameter. An excisional biopsy of the oral lesion was performed. Histopathological and immunohistochemical analysis confirmed the clinical hypothesis of neurofibroma. Because NF1 is one of the most common genetic diseases and oral manifestations are very common, dentists should be aware of the characteristics of this disease.
Similar content being viewed by others
Main
The term neurofibromatosis (NF) is used to a group of genetic disorders that primarily affect the cell growth of neural tissues. There are two forms of NF: neurofibromatosis type 1 (NF1) and neurofibromatosis type 2 (NF2).1,2 These two forms of NF have few common features and they are caused by mutations on different genes.2
NF1, also known as von Recklinghausen's disease, is the most common type of NF and accounts for about 90% of all cases.1 It is one of the most frequent human genetic diseases, with a prevalence of one case in 3,000 births.3 There is no sex or race predilection. NF1 is an autosomal dominant disease caused by a spectrum of mutations that affect the gene located at 17q11.2 chromosome, known as NF1 gene.2 It has one of the highest spontaneous mutation rates among genetic diseases in human beings. Only 50% of NF1 patients have positive family history of the disease. The other 50% represent spontaneous mutations.4
The expressivity of the disease is extremely variable, with manifestations ranging from mild lesions to several complications and functional impairment.3,5 The penetrance, otherwise, is 100%.3
Neurofibromata constitute an important feature of NF1. Café-au-lait spots, axillary and inguinal freckling, optic glioma, Lisch nodules (pigmented hamartomas of the iris) and specific bone lesions are also common clinical features of NF1.2 Oral manifestations can be found in almost 72% of NF1 patients.4
We report a case of a NF1 patient with periodontal manifestation. A discussion about NF1 oral manifestations is presented.
Case description
A 59-year-old white female patient was referred to our clinic for a non-ulcerated, non-painful swelling in the gingiva at the lingual aspect of the lower central incisors. The patient was referred with a suspected periodontal abscess. Our first clinical examination was performed in July 1999.
Reviewing the medical history, the patient reported having NF1. The diagnosis of NF1 was made at the age of 19. The patient was not aware of any other member of the family who had NF1.
The general clinical examination revealed hundreds of soft tissue cutaneous nodules on the body, including the face and neck (Fig. 1,Fig. 2). Five café-au-lait spots were noted on the trunk and upper arms (Fig. 3) Freckles could be seen diffusely over the back and axillary region. The patient reported that some pigmented lesions were present at birth and the other ones appeared when she was a child.
The cutaneous nodules began to develop in puberty and several of them had been presented when she was 18-years-old. She reported that the number of cutaneous nodules increased during the pregnancy. Short stature (1.5 m) was also observed.
Six months before our first clinical examination, the patient was diagnosed with a breast carcinoma (invasive ductal carcinoma) and was under chemotherapy and radiotherapy when she had been in our clinic.
Extra-oral examination revealed mandibular prognathism (Fig. 1). Intra-oral examination revealed an anterior cross-bite occlusion (Fig. 4). In addition, an isolated nodule was found at the lingual aspect of the attached gingiva of the lower central incisors (Fig. 5). This lesion was submucosal, non-ulcerated, non-painful and presented with an ovoid shape and normal color. It measured 1 cm in diameter and it was firm on palpation. The patient had no probing depth more than 2 mm on the lower incisors. All the teeth showed normal vitality, no decay and no history of accidental traumatism. The patient reported that the lesion had been there for more than 2 years with a slow growth. The lesion was clinically diagnosed as localized neurofibroma. No other lesions or intra-oral abnormalities were noted. The radiographs did not reveal any alteration. An excisional biopsy of the oral lesion was performed.
Results
Histopathologic findings confirmed the clinical diagnosis. The neoplasm was circumscribed but it was not encapsulated. It was composed of bundles of spindle cells having elongated, wavy and normochromatic nuclei. These cells were immersed in a stroma of delicate collagen bundles and moderate amounts of mixoid matrix. Giemsa stain confirmed the presence of numerous mast cells throughout the lesion. Immunohistochemical analysis for S-100 protein was positive for some spindle cells.
Discussion
Despite the advances of molecular biology, the diagnoses of NF1 and NF2 are still based on clinical criteria. The National Institute of Health Consensus Development Conference originally established the diagnostic criteria for NF1 and NF2 in 1987.6 (Table 1,2)
Pigmented lesions, one of the most common manifestations of NF1, are often present at birth or may appear during the first years of life.2,6,7 These pigmented lesions appear as café-au-lait spots and freckles.7 Café-au-lait spots are smooth-edged pigmented macules and their colour varies from yellowish to chocolate-brown. Their distribution is random over the body except for a disproportionately small number on the face.1 Freckles in the axillary or inguinal areas are very common and are referred to as Crowe's sign.7 In some patients with NF1, freckling may occur diffusely over the trunk, extremities, upper eyelids and base of the neck.2 Our patient exhibited five café-au-lait spots and freckles over her back and in the axillary region (Crowe's sign). Just as related in the literature, the patient reported that many pigmented lesions were present at birth and other ones appeared during childhood.
The NF1 gene is considered to be a tumour-suppressor gene because both benign and malignant tumours develop at an increased frequency in individuals with NF1.2,8 Loss-of-function mutations of the NF1 gene led to increased cell proliferation and the development of tumours.2
Neurofibromata are benign complex tumours that arise from peripheral nerve sheaths and constitute one of the main manifestations of NF1. Solitary neurofibroma may occur in an individual who does not have NF1, but multiple neurofibromata tend to develop in a person with such a disease. Clinical observation suggests that there are at least two major types of neurofibromata that may differ widely in their natural history: 'discrete' or 'localized' and 'plexiform' neurofibromata.2
A localized neurofibroma arises from a single site along a peripheral nerve and presents as a focal mass with well-defined margins. It can occur superficially or may involve deeper peripheral nerves. Localized neurofibromata are the most common type of neurofibromata that occur in NF1 patients. They are rarely, if ever, present at birth and usually appear in late childhood or early adolescence.2 The number of localized neurofibromata tends to increase with age, and varies widely from person to person. NF1 patients may have few, hundreds or even thousands of localized neurofibromata. Neurofibromata are found mostly on the skin. Nevertheless, many organs may be involved, including stomach, intestines, kidney, bladder, larynx and heart. In the head and neck region, the most commonly affected sites are the scalp, cheek, neck, and oral cavity.1
Several soft tissue lesions compatible with localized neurofibromata could be seen all over our patient's body. The literature reports an increase in size and number of localized neurofibromata during puberty and pregnancy.2 Our patient also reported an increase of her lesions during puberty and pregnancy.
A plexiform neurofibroma is a peripheral nerve sheath tumour that extends along the length of a nerve. This lesion may also occur superficially or deeper inside the body. Plexiform neurofibromata are a major source of morbidity associated with NF1 due mainly to their tendency to grow to large sizes and cause disfigurement. They may extend for some distance along a nerve and can involve multiple nerve branches. The cranial nerves most involved in plexiform neurofibromata are the fifth, ninth and tenth nerves.2
Although benign neoplasias are the majority of the neoplasias presented in NF1 patients, there is a low percentage of malignant neoplasias that occur in these individuals. These neoplasias represent the more serious complication of NF1. The most common malignancy seen in individuals affected with NF1 is the malignant peripheral nerve sheath tumour (MPNST). MPNST is a histologically malignant tumour that arises from the peripheral nerve sheath. Like neurofibromata, MPNSTs can also occur in the general population but they are more common in individuals with NF1. Pre-existing plexiform neurofibromata appear to be the most common precursor to MPNSTs in people with NF1.2
The case presented here showed the development of an invasive ductal carcinoma in a NF1 patient. However we cannot conclude that the breast carcinoma is related to NF1. It is known that malignant epithelial tumours associated with NF1 are very rare and it is appropriate to emphasize that breast carcinoma is one of the most common neoplasms in women and the peak incidence is near menopause.3,9 Invasive ductal carcinoma is the most common breast carcinoma.3
Short stature has long been known to be a feature of NF1 and it was also observed in our patient. The average height of individuals with NF1 is less than expected for age, but reduction in height is usually mild.2
NF1 patients may present facial alterations caused by hypoplasia or hyperplasia of the jaws, the zygomatic bone and the temporomandibular joint. Osseous alterations can be a product of soft tissue growing against or within the bone. It has also been reported that bone growth may be stimulated by adjacent neural tumour, leading to hyperplasia. However, bony defects may arise from mesodermal dysplasia unrelated to the proximity of the neural lesion.7 Plexiform neurofibroma on the face can also cause facial asymmetry. Exophthalmia caused by sphenoid wing dysplasia can also be present.10
In the past, the frequency of oral manifestations of NF1 was estimated to occur in 4 to 7% of all cases.7,11 However, two studies suggested that oral manifestations are much higher.4,10 The low frequency of oral manifestations in certain studies can be explained by the lack of radiographic examinations, ignoring the intraosseous manifestations. Oral manifestations were found in 72% of patients with NF1 in a study performed by Shapiro et al.10 According to a survey performed by D'Ambrosio et al.4 66% of his NF1 patients had at least one intra-oral manifestation of the disease and 58% of the patients presented manifestations in the maxilla and the mandible, detected by panoramic radiographs.
The most common oral finding of NF1 reported in the literature is enlargement of the fungiform papillae of the tongue that occurs in about 50% of cases.10,11 Another common oral tissue change is the presence of single or multiple neurofibromata.12 All hard and soft oral tissues have been reported to be affected with these tumours. However, the majority of oral neurofibromata occur in the tongue.10 The tongue may be involved by a localized neurofibroma, but macroglossia caused by plexiform neurofibroma may also occur. In our case, a localized neurofibroma was found in the gingiva, which is an uncommon localization. Shapiro et al.10 observed gingival neurofibromata in only 5% of all patients with NF1.
Oral localized neurofibromata present as discrete nodules of normal colour and they are usually asymptomatic. Nevertheless, neurofibromata on or adjacent to the cranial nerves also affect motor function of the facial and hypoglossal nerves and sensory function of the trigeminal nerve.10
Plexiform neurofibromata of the second division of the trigeminal nerve may include the pterygopalatine ganglion, the maxillary region and the upper gums. Tumours of the third division led to enlargement of the lower jaw, gums and anterior two thirds of the tongue.2 Plexiform neurofibromata involving the salivary glands had already been described, but these locations are very rare.13 Cases of oral MPNST are also uncommon, but they have been reported in the palate and the floor of the mouth.10
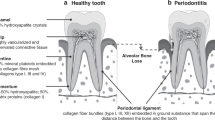
Oral radiographic findings include an enlarged mandibular canal, mandibular foramen and mental foramen. Neurofibromata can also develop intraosseously, resulting in well demarcated unilocular, but occasionally multilocular, radiolucent lesions. In our case, however, radiographic changes were not observed. Neurofibromata of the oral soft tissues or bone can cause malposition of the teeth with total or partial retention.1
The multiorgan occurrence of NF1 requires a multidisciplinary approach. Since there is no cure for NF1, the management must be toward prevention and control of the complications. Although the rate of malignant transformation of neurofibromata of NF1 is low (3–5%), these neoplasias can cause other clinical problems, including aesthetic and functional compromising, since they can assume great proportions and can be present in large numbers. Surgical treatment, therefore, is not always satisfactory, since the total removal of large and also multiple lesions is very difficult. The surgical intervention is indicated when the patient's function is compromised. There are esthetic problems or suspicion of malignant transformation. Risk, possible complication and expected benefit gained by such procedures should be considered.14 Despite previous beliefs to the contrary, many authors reported no increased malignant transformation in neurofibromata after surgical treatment.7
The NF1 patients must receive genetic counselling.15 These patients should be advised that the disorder is an autosomal dominant condition and that the probability of transmitting the disease to each offspring is 50% in both sexes.12 Because NF1 is one of the most common genetic disease and oral manifestations can be found in almost 72% of NF1 patients, dentists should be aware of the characteristics of this disease. It is important that dentists conduct long-term follow-up because of the potential for local complications and the known risk of malignant transformation.16 The rapid increase in size of the neurofibroma and presence of pain must raise the suspicion of malignant transformation.12 Biopsy of these lesions should be conducted for histopathological evaluation.
References
Gorlin RJ, Cohen MM, Levin LF . Syndromes of the head and neck. p. 353–416. Oxford: Oxford University Press, 1990.
Friedman JM, Gutmann DH, MacCollin M et al. Neurofibromatosis. Phenotype, natural history and pathogenesis. Baltimore: the Johns Hopkins University Press, 1999
Cotran RS, Kumar V, Robbins SL . Robbins Pathologic Basis of Disease. 5th ed. Philadelphia: W. B. Saunders Company, 1994.
D'Ambrosio JA, Langlais RP, Young RS . Jaw and skull changes in neurofibromatosis. Oral Surg Oral Med Oral Pathol 1988; 66: 391–396.
Dugoff L, Sujansky E . Neurofibromatosis type I and pregnancy. Am J Med Genet 1996; 66: 7–10.
Gutmann DH, Aylsworth A, Carey JC et al. The diagnostic evaluation and multidisciplinary management of neurofibromatosis 1 and neurofibromatosis 2. JAMA 1997; 278: 51–57.
Geist JR, Gander DL, Stefanac SJ . Oral manifestations of neurofibromatosis types I and II. Oral Surg Oral Med Oral Pathol 1992; 73: 376–382.
Fahsold R, Hoffmeyer S, Mischung C et al. Minor lesion mutational spectrum of the entire NF1 gene does not explain its high mutability but points to a functional domain upstream of the GAP-related domain. Am J Hum Genet 2000; 66: 790–818.
Polyak K . On the birth of breast cancer. Biochim Biophys Acta 2001; 1552: 1–13.
Shapiro SD, Abramovitch K, Van Dis ML et al. Neurofibromatosis: oral and radiographic manifestations. Oral Surg Oral Med Oral Pathol 1984; 58: 493–498.
Neville BW, Damm DD, Allen CM et al. Oral and Maxillofacial Pathology. pp. 381–383. Philadelphia: WB Saunders Company, 1995.
Vincent SD, Williams TP . Mandibular abnormalities in neurofibromatosis. Oral Surg Oral Med Oral Pathol 1983; 55: 253–258.
Derekoy S, Sefali M . Plexiform neurofibroma of the submandibular gland. J Laryngol Otol 2000; 114: 643–645.
Holtzman L . Radiographic manifestation and treatment consideration in a case of multiple neurofibromatosis. J Endod 1998; 24: 442–443.
Maceri DR, Saxon KG . Neurofibromatosis of the head and neck. Head Neck Surg 1984; 6: 842–850.
Epstein JB, Schubert MM, Hatcher DC . Multiple neurofibromatosis. Report of a case. Oral Surg 1983; 56: 560–562.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Cunha, K., Barboza, E., Dias, E. et al. Neurofibromatosis type I with periodontal manifestation. A case report and literature review. Br Dent J 196, 457–460 (2004). https://doi.org/10.1038/sj.bdj.4811175
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4811175
This article is cited by
-
The interaction between the nervous system and the stomatognathic system: from development to diseases
International Journal of Oral Science (2023)
-
Increased extracellular matrix deposition during chondrogenic differentiation of dental pulp stem cells from individuals with neurofibromatosis type 1: an in vitro 2D and 3D study
Orphanet Journal of Rare Diseases (2018)
-
Gingival overgrowth: Part 1: aetiology and clinical diagnosis
British Dental Journal (2017)
-
High prevalence of hyposalivation in individuals with neurofibromatosis 1: a case–control study
Orphanet Journal of Rare Diseases (2015)
-
Von Recklinghausens Disease: A Series of Four Cases with Variable Expression
Journal of Maxillofacial and Oral Surgery (2015)