Key Points
-
PROHIs provide a means of recording the patients view of their own dental health
-
PROHIs are capable of describing and valuing dental health care
-
PROHIs are capable of identifying population subgroups in which there is a shortfall in dental health.
Abstract
An understanding of a broader concept of health is increasingly important for all health professionals, including dentists, and has recently been incorporated as a key principle in the Government White Paper, The New NHS1. This aims to deliver a dependable, high quality, egalitarian health service. In the past, performance measurements in the UK have often relied simply on those areas which are most easily quantified. For example, within the hospital service, performance was measured in terms of the cost and the number of finished consultant episodes, from which the 'purchaser efficiency index' was calculated. This tended to produce a driving force rewarding those doing more rather than those doing more better. It is analogous to the system which has been the backbone of NHS dental practice for many years, 'fee per item of service', where throughput is rewarded rather than outcome. However, the White Paper has signalled a move away from simply counting activity. From April 1999 within the hospital service the purchaser efficiency index has been replaced with more rounded measures, reflecting the changing concepts of health, in a new broader performance framework to determine what really counts for patients. It will focus on measuring health improvement, fairer access, better quality and outcome, including the views of patients.
Similar content being viewed by others
Main
Dentistry has been somewhat slower than medicine in responding to this changing concept of health, and in using indicators based on patients own assessment of their health. The dental profession have for many years used clinical indices to measure oral health and determine outcome, familiar examples are the number of decayed, missing and filled teeth, periodontal pocket depth on probing and the presence of plaque or calculus (e.g. the CPITN or the BPI). Whilst these indicate the patho-physiology of dental disease they fail to take account of the patient's perspective and impact of oral problems on their day to day life. They are clearly measures of disease rather than health. Clinical indicators remain an essential component of oral assessment, particularly in children and young adults for whom elimination of disease is often both possible and beneficial. However, alone they cannot capture the overall impact of oral disease as they essentially only reflect the end-point of the disease process, leaving the patient's perspective of their oral health largely unknown. A more complete assessment can only be determined by incorporating the patient's self reported perception of their oral health. This aspect is especially relevant amongst an older population who are increasingly dentate, but for whom a clinically perfect mouth is often neither possible nor desirable. It would be particularly helpful in this new environment to acknowledge that a broader concept of oral health is necessary, one which includes the patient's own ratings and perceptions of their health. This involves recording the impact of dental disease and the interventions used to treat dental disease on people's daily lives, in other words their health related quality of life (HR-QoL).
In the 1970s, it became clear that there was a need for these QoL measures, to define the social and psychological consequences of oral disorders.2 Research in this area revealed that patients appeared to base their oral health perceptions on functional concerns,3 which demonstrated only a weak relationship with clinical assessment. In other words patients and dentists have often used different criteria to assess oral health. Rosenberg and Kaplan found that whilst the periodontal status and the number of dental symptoms explained some of the self reported dental health status, the DMFT values did not.4 Cushing et al. also reported inconsistent associations between clinical indices and the social impact of dental disease.5
These alternative HR-QoL measures, based on patient's perceptions have come some way since this early work and are of increasing relevance to dentists:
-
The measures could be useful to dentists for monitoring and auditing their own work
-
They may be used by administrators who run health services (or insurance companies) as ways of measuring effectiveness of dentists and dental services and as a way of prioritising different dental needs when allocating resources
-
They may be useful as outcome measures in clinical trials of new techniques and materials.
How do you measure health related quality of life?
QoL can be thought of in its broadest sense as the sum of all the factors in a patient's life, including for example, health, environment, personality, age, housing, employment, and family situation. Health related QoL (HR-QoL) is a narrower concept and generally considered to encompass the effect of symptoms caused by the disease and its treatment, physical status, psychological functioning and social functioning.
The term 'QoL measurement' conveys the impression of precision, as in the physical sciences where results are expressed in standard units of measure. However this is not how it actually works. QoL can be defined, measured and quantified in a multitude of ways and approaches to this problem of measuring HR-QoL fall into two basic categories. Firstly, you can use a proxy indicator, of which some examples are listed in Table 1. Within dentistry, Reisine used a proxy indicator and investigated the effects of dental conditions on QoL by using the number of days work loss associated with dental problems.6,7 In fact, whilst the work loss days as a result of dental disease may be small for the individual, the accumulated work loss within a population is significant and has economic ramifications. This type of indicator has the advantage of being relatively simple to observe and collect data on, but the way these variables are linked with health related QoL is often a matter of some conjecture.
The second approach to the measurement of health related QoL uses one of a number of alternative questionnaires, designed for self-completion by patients. The questionnaire can be termed generic, when it is designed to measure health related QoL across the widest possible range of health settings, for example the Sickness Impact Profile8 and Euro QoL EQ-5D.9 These give an indication of overall health. Alternatively they can be specific, intended for use in a particular disease or treatment setting. Examples include the Arthritis Impact Measuring Scale and Functional Living Index-cancer. Within these two extremes, indicators can be developed for use in a context-specific setting, that is within a particular discipline of medicine, for example dentistry. These patient rated oral health indicators (PROHI), sometimes referred to as 'subjectively reported instruments' allow patients to rate their own oral health state.
The content of the questions are not simply thrown together off the top of a social scientist's head, but are developed over a period of time using sound scientific and statistical methodology. They may be based on a preconceived and accepted model, as in the work of Locker10 or derived from a number of different reference groups, for example patients with first hand experience of illness, dentists, doctors, or other professionals with objective insights.
Almost all formal questionnaires are composed of two complementary elements. Firstly, a system of describing health states, which consists of questions or statements to which the patient indicates their response. Secondly, a means of weighting those states in order to account for any imbalance in the impact of the dimensions under investigation. The weights need careful consideration as they may be important. To illustrate this, consider two different oral dimensions, pain, and chewing ability. Their impact on QoL is unlikely to be identical. In a representative population pain may have a much greater impact than chewing ability on QoL and may require a higher weight. On the other hand it may have lesser impact and be given a lower weight. The rationale for weights is to enable the relative importance of each dimension to be identified, and to allow for the aggregation of information across dimensions -- thus generating a single summary score. The weighting of health status measures is both a crucial and topical issue, although within dentistry there is currently little evidence to suggest that weighting of items substantially improve the performance of health status measures.11,12 The weights are usually derived from a reference population, which might be patients, health-care professionals or the general public. In some indicators they are derived separately for each individual as they complete the questionnaire. Clearly the choice of method can play a significant part in determining the range and dispersion of scores. By ascribing weights to the dimensions it is then possible to combine scores for an individual to yield a single score, referred to as an 'index' which gives a very easy to handle statistic and could be particularly useful in establishing cost-effectiveness of treatment options.
Alternatively data can be represented as a profile; a series of scores representing different areas of QoL which may be affected by oral health. This often provides a more meaningful picture, although it may be more difficult to make direct comparison between patients, and also a comparison in the calculation of the magnitude and direction of the change in health status.
Over the last decade a number of such PROHIs have been developed and the reliability and validity of these scales are being analysed in on-going research. Examples of these context-specific, oral health related QoL measures can be seen in Table 2. Research in this field has not been restricted to the UK, and differences exist in the development and applications of these instruments. Some instruments are specific and are designed for use in certain patient groups, (for example, the GOHAI was originally designed for use in the elderly). A number are generic to dentistry, capable of being used in the widest possible range of dental health settings. Only time will tell if one of these will emerge as the most accepted and commonly used. It is already becoming clear that to be of use, these instruments have to be practical. In other words, easily completed by patients, so lengthy instruments have been more difficult to employ and to date, OHIP has been the most widely applied instrument in the UK.
How could patient-rated oral health indicators be used in dental practice?
Dentists are well aware that the impact of oral conditions varies between individuals, for instance there are some patients with relatively minor dental problems as classified by clinical indices, but for whom the impact on their day to day life is significant. Sometimes the reverse is true, where clinical indices demonstrate what appears to be a significant dental problem but the impact on their life is minor. Implementing PROHIs provides a means of recording this information in a valid and reliable way and may be of value to a number of groups. These include dentists, administrators and researchers, all of which could have an impact on dental practice. Within medicine, these types of subjective health status measures have been used to assess outcome following treatment. In particular they have been used to investigate patients with rheumatoid arthritis, mental health problems and cancer, already indirectly affecting resource allocation. The potential applications of PROHIs are summarised in Table 3. Within the general dental service, dental practitioners may use PROHIs as a screening tool in simply measuring self-rated oral health at a particular moment in time, allowing the dentist to make more informed decisions about treatment options. Alternatively they could be used over time; for example, in interventional or observational studies or even in clinical audit to measure change. This information may be used when advocating public funding of treatment methods for individual patients.
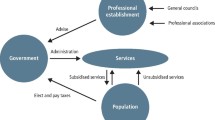
In the future, PROHIs may be useful in providing information for Health Service Administrators when planning the service and setting priorities as the 'New NHS' must be accountable to patients, and shaped by their views. The information they yield would be useful to purchasers, providers and consumers in order to make informed choices about healthcare, particularly where financial resources are limited but technological advances are continually expanding the range of treatment options available. They provide a means of assessing cost-benefit analysis and assessment of performance and outcome. For example, in the NHS alone, £50 million per annum are spent on the provision of partial dentures.21 We need to ask which patients really benefit from these and what can we do to stop a large proportion ending up in the top drawer? Administrators assigned to drive efficiency are seeking value for money. They are adopting a more vigorous approach to performance measurement, incorporating patient views, to ensure that every pound is spent to maximise care. PROHIs provide the mechanism to collect this information and may soon help to determine the way treatments are allocated.
Researchers have already found uses for PROHIs, not just as an alternative for measuring the population's health, as in the 1998 Adult Health Survey, but also as a way of evaluating the outcome of new treatments in clinical trials. For instance, the field of dental implantology is rapidly expanding, and this relatively new and expensive dental intervention could be prescribed for many existing conventional denture cases. However, provision in the public sector is limited by cost. PROHIs provide a way of determining whether and to what extent the patient perceives that they have benefited from treatment so one form of treatment can then be assessed against another. It may be possible to identify those patient subgroups likely to feel the greatest benefit from a particular form of treatment.
These oral HR-QoL instruments are continuing to be developed and evaluated. Researchers have tended to either adapt existing measures of general health status or alternatively have developed measures specific to oral health (see Table 2 for details). The more specific an instrument, the more likely it is to detect subtle changes but it will say little about the relative worth or outcome of health status across treatment groups. The generic measure places oral health within the domain of general health, but there is a trade off in that it may lack the sensitivity to the impact of more subtle oral conditions. However it does have the advantage that it can be used across differing specialities in medicine and dentistry allowing comparison of the impact of differing diseases and treatments on a patient's QoL. Oral health can then be compared alongside respiratory disease or gastrointestinal disorders (for example).
To the uninitiated, the application of QoL measures can appear to entail much uncertainty. Today, the view of the consumer is central, so it is likely that QoL research will continue to develop, as it provides a means of collecting this data. Presently we have a number of conceptually accepted and validated instruments but if PROHIs are to be of any use they have to perform in the field. Original PROHIs were designed for use in face to face interviews, although many are now developed for use in postal surveys. For researchers and administrators this type of tool is straight-forward to use, but does have some inherent potential problems, for example non-response bias. The ideal instrument for practitioners to administer would be short, have good validity, precision and reliability properties and various measures are currently available which can be completed in approximately five minutes.9,15
It may be useful to use one selectively targeted instrument in tandem with a generic measure when investigating a specific population or intervention. The next step is to determine population 'norms' and to perform controlled interventional studies. This work depends on collaboration of clinicians and health-care researchers, thus evaluating the effects of dental care.
We then have the exciting prospect of being able to identify quickly and easily those oral conditions responsible for the greatest effect on HR-QoL and the change in HR-QoL that dentistry can produce. This information is central to a proper evaluation of the impact of dental care. QoL measurement is here to stay.
References
Secretary of State for Health. The New NHS. 1997; London: Stationery Office.
Cohen L K, Jago J D. Toward the formulation of sociodental indicators. Int J Health Serv 1976; 6: 681–98.
Aitchison K, Dolan T. Development of the geriatric oral health assessment index. J Dent Educ 1990; 54: 680–7.
Rosenberg D, Kaplan S, Senie R, Badner V. Relationships among dental functional status, clinical dental measures and generic health measures. J of Dent Educ 1988; 52: 653–657.
Cushing A M, Sheiham A, Maizels J. Developing sociodental indicators-the social impact of disease. Community Dent Health. 1986; 3: 3–17.
Reisine S. Dental disease and work loss. J Dent Res 1984: 63: 1158–61.
Reisine S T, Miller J A. A longitudinal study of work loss related to dental diseases. Soc Sci Med 1985; 21: 1309–14.
Gilson B S, Gilson J S, Bergner M, Bobbit R A, Kressell S, Pollard W E, Vesselago M. The sickness impact profile. Development of an outcome measure of health care. Am J of Public Health 1975; 65: 1304–1310.
The EuroQol group. EuroQol -- a new facility for the measurement of health related quality of life. Health Policy 1990; 16: 199–208.
Locker D. Measuring oral health: a conceptual framework. Community Dent Health 1988; 5: 3–18.
Leao A, Sheiham A. The development of a socio-dental measure of dental impacts on daily living. Community Dent Health. 1996; 13: 22–26.
Allen D F, Locker D. Do item weights matter? An assessment using the oral health impact profile. Community Dent Health 1997; 14: 133–138.
Locker D, Miller Y. Evaluation of subjective oral health status indicators. J of Public Health Dent 1994; 54: 167–176.
Slade S G, Spencer J A. Development and evaluation of the Oral Health Impact Profile. Community Dent Health 1994; 11: 3–22.
Slade G D. Derivation and validation of a short-form oral health impact profile. Community Dent Oral Epidemiol 1997; 25: 284–90.
Leao A. The development of measures of dental impact on daily living. PhD thesis, 1993; University College London.
Kind P, Boyd T, Corson M A. Measuring dental health status: calibrating a context-specific instrument. 1998; In proceedings of International Society for Technology in Health Care, Ottawa, Canada.
Kind P, Boyd T, Corson M A. Measuring dental health status: comparison of EQ-5D and DS-QoL. 1998; In proceedings of the 14th EuroQoL Scientific Plenary, Hanover, Germany.
Steele J G, Sheiham A, Marcenes W, Walls A. National Diet and Nutrition Survey: people aged 65 years and over. Volume 2. Report of the Oral Health Survey. 1998; London: Stationery Office.
Strauss R P, Hunt R J. Understanding the value of teeth to older adults: influences on the quality of life. J Am Dent Assoc 1993; 124: 105–10.
Dental Practice Board annual prescribing profile. April 1995–March 1996.
Author information
Authors and Affiliations
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Corson, M., Boyd, T., Kind, P. et al. Measuring oral health: does your treatment really make a difference. Br Dent J 187, 481–484 (1999). https://doi.org/10.1038/sj.bdj.4800310
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4800310
This article is cited by
-
Promoting menstrual health among persian adolescent girls from low socioeconomic backgrounds: a quasi-experimental study
BMC Public Health (2012)
-
The effectiveness of out-of-hours dental services: I. pain relief and oral health outcome
British Dental Journal (2005)
-
The impact of attendance patterns on oral health in a general dental practice
British Dental Journal (2002)