Abstract
Treatment planning may be facilitated by determining the desired end result which meets the needs of the patient, and then planning in reverse order to achieve this goal.
Similar content being viewed by others
Main
Treatment planning for the provision of an implant retained restoration is essentially the same as that for the conventional restoration, except it also has to consider the provision of an adequate number, type, position and distribution of implants. It therefore involves a surgical phase of treatment (Part 6) and a time delay for the process of osseointegration to take place. The treatment plan should begin with a clear idea of the end result which should fulfil the functional and aesthetic needs of the patient. It is important that these goals are realistic, predictable and readily maintainable.
Types of implant restoration
Before considering the more detailed aspects of planning the following types of implant retained restoration are described:
-
Fixed bridges
-
Overdentures
-
Single tooth restorations.
Fixed bridges
Implant retained fixed bridges range from limited span bridges to complete arch restorations for the edentulous jaw. There are two basic bridge designs, the original type as described by Branemark which was a cast metal bar with acrylic teeth and 'gumwork' attached to a number of implants and resembled a denture on stilts (fig. 1), and the more modern aesthetic approach where it resembles conventional bridgework with implants placed so that the prosthetic teeth appear to emerge from the natural soft tissues (fig. 2). These two designs will be considered in more detail.
The bridge is similar in design and concept to that described by Branemark. Titanium abutments protrude a few millimetres through the mucosa and a space separates the bridge superstructure from the underlying mucosa. The prosthetic teeth are acrylic and have 'gumwork' in much the same fashion as a complete denture. This bridge is very rigid and is not removable by the patient
Maxillary bridges usually require a more aesthetic approach and the design of bridge gives the impression that the teeth are emerging from the gum. The bridge design in figure 1 would not be suitable in this case
The original Branemark 'bone anchored bridge' is the design on which many of the long-term success reports are based. It was largely used in the mandible and required the placement of five to six implants between the mental foramina. A cast metal framework is cantilevered distally, generally to a distance of about 12 mm but determined by the size of the bar and the maximum antero-posterior distance between implant centres.
In this part, we will discuss:
-
Types of implant restoration
-
Planning considerations
-
Provisional restorations
-
Treatment order
In the mandibular arch, prosthetic stability has been reported for 99% of fixed prostheses over a 15-year period. However, lack of facial support and cheek biting can present appearance and functional limitations, especially in patients with more advanced bone resorption. Fixed prostheses in the mandible opposing a complete denture may also cause more bone loss in the opposing jaw than a mandibular overdenture. More frequent maxillary denture relines and potential for retention problems have been noted.
Although maxillary prosthetic survival rates of 92% have been reported over a 15-year period, more complications are encountered. Phonetic problems are the most frequent complaint. Spaces between the bridge and the underlying soft tissues result in breaks in the palatal contour and speech disruption. Oral hygiene may be compromised if acrylic flanges are extended over abutments and soft tissue hyperplasia may occur. Although the situation can be improved by placing a removable gingival veneer, they are complex and technically demanding restorations. The appearance can be very good but in patients with less ridge resorption or a high smile line, there is a greater likelihood of aesthetic problems.
Type of implant restoration
-
Fixed bridges
-
Overdentures
-
Single tooth restorations.
Modern bridges usually have a cast metal framework extending beneath the soft tissue to connect to the implant abutments. The prosthesis is similar in design to a conventional fixed bridge prosthesis constructed on natural teeth and can be cemented or screw retained. In favourable circumstances, with minimal bone resorption, it is possible to achieve optimal aesthetics. Conversely when there has been substantial loss of bone, or when soft tissue replacement is required, it may be impossible to achieve the desired aesthetic result with this type of restoration. Where there is considerable labial resorption, the prosthetic teeth become progressively long, with large spaces apparent interproximally. In patients with a high lip line, the result is aesthetically unacceptable and the large spaces also compromise speech.
The intermaxillary relationship affects the design and use of these bridges. In restoring the maxillary arch in patients with an orthognathic jaw relationship (Angles Class 1), a ridge lap of the crown is not usually necessary. In situations where there is a severe space limitation, and ridge lap pontics are required for aesthetics, it is best to avoid implants in the incisor region. Patients with a Class III malocclusion and more than minimal bone resorption may not be suitable for this type of maxillary fixed restoration. Cantilevering a fixed prosthesis more than one abutment diameter posteriorly and two abutments anteriorly is ill advised if the high bending moments during occlusal load are to be prevented. Patients with advanced bone loss are not usually suitable for these restorations because of the unfavourable biomechanics and inadequate facial and lip support.
Bone grafting may be necessary to avoid this problem (Part 8) or an alternative restoration chosen, such as an overdenture or patient detachable bridgework. In the latter design a cast metal bar is attached to an equivalent number of implants used for fixed bridgework. A superstructure bearing the prosthetic teeth and a labial flange can be removed by the patient for daily oral hygiene. The restoration is implant supported and although the teeth and labial flange are detachable there is a high level of 'security'. The restoration is difficult to manufacture, requiring a high level of precision with retention of the removable section of the prosthesis dependent on the accuracy of fit onto the milled bar.
Overdentures
These are patient removable complete dentures retained usually by implants joined with a straight round bar or with 'ball' attachments (fig. 3). In the mandible the classic overdenture design is based on two implants placed in the mandibular canine regions and connected together by a bar which should be parallel to a line drawn between the mandibular condyles. The implants greatly improve retention and stability of the denture. Support for the denture is improved anteriorly but the posterior saddles are mucosal supported. In severely resorbed mandibles continued loss of bone has been reported in the molar areas. These overdentures may be also be retained by individual stud attachments with a high degree of success. In the maxilla, the failure rate is much higher, probably due to the poorer bone quality in the maxilla and high mechanical forces. It is usually recommended to provide at least four implants joined rigidly together with a bar (fig. 3d). Maxillary overdentures are more often opposed by a fixed dentition than mandibular overdentures and higher occlusal forces on the implants could be generated.
Single tooth restorations
Single tooth restorations are individual free-standing units not connected to other teeth or implants (fig. 4). They are similar to conventional single crowns and are normally cemented to prefabricated or customised abutments. Cantilever units are not normally recommended, and if two adjacent teeth are missing the requirement is for placement of two implants. If more than two adjacent teeth are missing, for example four incisor teeth, the decision has to be made whether to restore the space with four single units or a fixed bridge using fewer implants. The latter option is the one most often used because space is not normally available to provide an implant per tooth (see later section on implant spacing).
High success rates have been reported for single tooth restorations, particularly those replacing anterior teeth. Replacement of single molars is more problematic because of the size discrepancy between implant and tooth and the high occlusal loads. Therefore, wider diameter (5–6 mm) or two standard diameter implants may be used if space and finances allow.
Planning considerations
For simplicity, it will be assumed that treatment options other than implant retained restorations have been considered (Part 3) and there are no contra-indications. Planning begins with an assessment of the aesthetic and functional requirements, and proceeds to more detailed planning with intra-oral examination, diagnostic set-ups, appropriate radiographic examination (Part 5), and construction of provisional restorations and surgical guides.
Planning considerations
-
Functional and aesthetic considerations
-
Evaluation of the endentulous ridge
-
Study casts and diagnostic set-ups
-
Implant numbers and spacing
Functional and aesthetic considerations
Reduced or insufficient function is a common complaint for patients who have removable dentures or who have lost many molar teeth. Function of an otherwise adequate denture may be improved by providing implants to aid stability and retention. The alternative treatment is to replace the denture with a fixed bridge. The overdenture may be the treatment of choice where:
-
The patient does not have a psychological problem with dentures and is quite happy to wear a removable restoration
-
There is considerable resorption of the jaws allowing few implants to be placed
-
The opposing jaw is restored with a satisfactory denture or the opposing teeth may be compromised by the occlusal forces generated by a fixed implant supported restoration.
The fixed bridge may be the treatment of choice where:
-
There is a good dentition in the opposing jaw which may de-stabilise the denture. This is a particular problem where a natural dentition in the maxilla opposes an edentulous mandible (fig. 1).
-
Patients have such a strong gag reflex that they cannot tolerate a removable prosthesis
-
Resorption of the jaws is not too advanced thereby allowing placement of an adequate number of implants, and the prosthetic replacement of large amounts of soft and hard tissue is not required.
A shortened dental arch extending to the first molar or second premolar should always be considered. Providing there are sufficient well distributed implants in the anterior part of the jaw, a distal cantilever extension can be used, thereby avoiding placement of implants in more difficult anatomical locations. Patients who request replacement of missing molar teeth need sufficient bone above the inferior dental canal or below the maxillary sinus floor to allow implants of sufficient length to withstand high occlusal forces. For example, replacement of the first and second molars would require a minimum of three standard implants joined together with a fixed bridge. The occlusion should be carefully assessed, particularly in all excursive movements. It may be helpful to examine the occlusion with the existing prosthesis or the provisional prosthesis to assess the type of loading to which the implant restoration will be subjected.
Aesthetic considerations may assume great importance in some patients. The coverage of the anterior teeth (and gingivae) by the lips during normal function and smiling should be carefully assessed (figs 5 and 6). An anterior restoration should also provide adequate lip support. The appearance of the planned restoration can be judged by providing a diagnostic set up or a provisional restoration (fig. 7). They may also serve extremely well as a model for the surgical stent or guide to assist in the optimal placement of the implants (fig. 8), and also as a transitional restoration during the treatment programme. Ideally, the patient should be examined with and without their current or provisional prosthesis to assess facial contours, lip support, tooth position and how much of the prosthesis is revealed during function.
Evaluation of the edentulous ridge
The height, width and contour of the ridge can be visually assessed and carefully palpated (fig. 9). The presence of concavities/depressions (particularly on the labial aspects) are usually readily detected. However, accurate assessment of the underlying bone width is difficult, especially where the overlying tissue is fibrous. This occurs on the palate where the tissue may be very thick and can result in a very false impression of the bone profile. Clinical techniques such as ridge mapping may help. The area under investigation is given local anaesthesia and the thickness of the soft tissue measured by puncturing it to the bone using either a graduated periodontal probe or specially designed callipers. The information is transferred to a cast of the jaw which is sectioned through the ridge (fig. 10). This method gives a better indication of bone profile than simple palpation but is still prone to error. Whenever evaluation of the bone width and contour is critical, radiographic assessment is advised (Part 5).
The angulation of the ridge and its relationship to the opposing dentition is also important. The distance between the edentulous ridge and the opposing dentition should be measured to ensure that there is adequate room for the restorative components. Proclined ridge forms will tend to lead to proclined placement of the implants which could affect aesthetics and loading. Large horizontal discrepancies between the jaws, for example the pseudo class III jaw relationship following extensive maxillary resorption are not suitable for treatment with fixed bridges.
The clinical examination of the ridge also allows assessment of the soft tissue thickness which is important for the attainment of good aesthetics. Keratinised tissue which is attached to the edentulous ridge will also generally provide a better peri-implant soft tissue than non-keratinised mobile mucosa (Part 2). The length of the edentulous ridge can be measured to give an indication of the possible number of implants that could be accommodated. However, this also requires reference to radiographs to allow a correlation with available bone volume and the diagnostic set-up for the proposed tooth location. In edentulous ridges bound by teeth, the available space will also be affected by angulation of adjacent tooth roots, which may be palpated or assessed radiographically (fig. 11).
Study casts and diagnostic set-ups
Study casts, preferably articulated, allow detailed measurements of many of the factors considered in the previous section. The proposed replacement teeth can be positioned on the casts by the technician using either denture teeth or teeth carved in wax. The former have the advantage that they can be converted into a temporary restoration which can be evaluated in the mouth by the clinician and patient (fig. 7). The diagnostic set-up therefore determines the number and position of the teeth to be replaced and their occlusal relationship with the opposing dentition.
Once the diagnostic set-up has been approved it can be used to construct a stent or guide for radiographic imaging (fig. 12 and see Part 5) and surgical placement of the implants (fig. 8 and see Part 6). The stent/guide can be positioned on the original cast and with reference to the radiographs, the clinician can decide upon the optimum location, number, and type of implants.
Implant numbers and spacing
There are a few general guidelines as to the number of implants that are required in different situations (Table 1).
The more teeth which require replacement the greater the variation, especially when molar teeth are also considered. For example, four missing lower incisors could be replaced quite readily with two implants supporting a four unit bridge. Four missing upper incisors could be replaced with a bridge supported by three implants, but four implants would be required in a spaced dentition.
Two missing molar teeth would require three standard implants, or alternatively two wider diameter implants. Implants with different diameters can be chosen according to the tooth they are replacing. For example, most systems have a standard implant of about 4 mm in diameter that can be used in most situations. However, replacement of single upper lateral incisors, or lower incisors, may require narrower diameter implants (eg 3.25 mm) whereas a molar tooth may be more satisfactory replaced with an implant of 5 to 6 mm diameter.
It is a great mistake to attempt to place too many implants in a given space (fig. 13) and, if necessary, orthodontic treatment should be used to optimise spacing (fig. 14). Spacing is required to provide:
-
An adequate width of bone and soft tissue between implants and adjacent teeth
-
For the prosthetic components not to impact on each other
-
For the patient to be able to clean the prosthesis effectively.
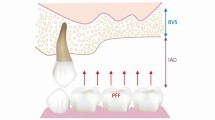
Implants placed next to natural teeth should allow an absolute minimum of 1 mm of intervening bone and preferably 2 mm. It is advisable to allow a little more spacing between implant heads, ideally 3 mm and no less than 2 mm. This is because in many systems the abutments are larger than the implant heads, and the restoration is often designed so that it increases in diameter to establish a good emergence profile. With all these factors competing for space it is easy to see how the soft tissue and oral hygiene may be compromised if implants are placed too close together.
Provisional restorations
-
Complete denture
-
Partial denture
-
Adhesive bridgework
-
Fixed bridgework
It should be noted that the above guidelines take no account of the differing implant diameters which are available. In many cases, manufacturer's recommend minimal centre-to-centre spacing of the implants, which is dependent upon their diameter and the minimum intervening tissue requirements described above.
The bone volume which can accommodate the proposed diameter and length of implant has to be determined radiographically. Implants should be selected to ensure optimum fixation, but seldom are implants longer than 15 mm required. In many instances the clinician is limited by the need to avoid damage to important anatomical structures, such as the inferior dental nerve. The assessment of length should allow an adequate safety margin, particularly as many drills are designed to prepare the implant site slightly longer than the chosen implant.
Provisional restorations
In the majority of treatment plans the provisional restoration is an essential component. It helps to establish the design of the final reconstruction and is used by the patient throughout the treatment stages. The following provisonal restorations are used:
-
Complete denture
-
Partial denture
-
Adhesive bridgework
-
Fixed bridgework.
Complete dentures are used as a provisional restoration for edentulous patients. There is a period (1–2 weeks) following surgical placement of implants when the dentures must not be worn. This avoids early transmucosal loading of the implants and allows adequate reduction of post surgical oedema to take place, facilitating proper adaptation of the denture. In general bone grafting and ridge augmentation procedures should not be carried out unless the denture can be left out for a considerable period after surgery.
Partial dentures can be used in anterior and posterior saddles and the same constraints apply as to full dentures (fig. 15). They are simple and inexpensive to construct. Acrylic dentures allow easy adjustment to accommodate any changes in tissue profile following implant placement and the transmucosal abutments when they are fitted.
Adhesive bridgework is most commonly used as a provisional restoration in the replacement of single teeth or small spans in anterior regions. A single tooth replacement is normally retained by a single adjacent retainer, whereas the replacement of multiple teeth requires more abutments. Provisional retainers should be easily removable and, therefore, the Rochette rather than Maryland design is recommended (fig. 16).
Fixed bridgework retained by full coverage restorations may be the treatment of choice, particularly for patients having extensive treatment who are not prepared to undergo a period of time without a fixed restoration. This assumes the presence of a sufficient number of teeth to support the provisional or transitional bridge. It also enables ridge augmentation procedures to be carried out without the risk of transmucosal loading and the associated micromovement affecting the healing. The bridgework may have to remain in place some considerable time with frequent removal and replacement. Abutment teeth must be adequately prepared to allow for the casting of a metal framework of sufficient strength and rigidity and for the acylic/ composite. Allowance should be made for the fact that the bridge will have to be modified following abutment connection.
Treatment order
Deciding on the treatment order may be very straightforward in some circumstances and in others extremely difficult, particularly for those cases involving transitional restorations.
A traditional plan may include the points listed in Table 2.
Conclusion
Treatment planning for implant restorations may at first appear complicated. It is imperative to consider all treatment options with the patient, and during detailed planning it may become apparent that an alternative solution is preferred. In all cases the implant treatment should be part of an overall plan to ensure health of any remaining teeth. Once the goal or end point has been established it should be possible to work back to formulate the treatment sequence. The cost of the proposed treatment plan is also of great relevance. The greater the number of implants placed, the higher will be the cost and this may therefore place limits on treatment options.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Floyd, P., Palmer, R. & Barrett, V. Treatment planning for implant restorations. Br Dent J 187, 297–305 (1999). https://doi.org/10.1038/sj.bdj.4800265
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4800265
This article is cited by
-
Implant retention systems for implant-retained overdentures
British Dental Journal (2017)