Abstract
Objective To assess the prevalence, nature and outcome of medical emergencies experienced by general dental practitioners (GDPs) over a 10-year period.
Design Postal questionnaire survey of a random sample of GDPs in Great Britain.
Subjects 1500 GDPs, 1000 in England & Wales and 500 in Scotland.
Results There was a 74% response. Emergency events were reported by 70.2%: the number reported by a single individual ranged from none to 33. The most commonly experienced events, including those associated with general anaesthesia, were (as a percentage of the total) for England & Wales and Scotland, respectively: fits and seizures (31.0%, 36.3%); swallowed foreign bodies (15.7%, 18.1%); attacks of asthma (13.8%, 11.1%); chest pain associated with angina pectoris (10.1%, 11.0%) and diabetic events (10.6%, 9.0%): none of these resulted in any serious sequelae. More events were reported in Scotland. Overall, there were 20 deaths resulting from medical emergencies reported in the survey, 4 affecting passers-by and none associated with general anaesthesia. 8849 years of practice experience were represented (by 94% of respondents), from which an estimate of the frequency of events was made.
Conclusions An emergency event was reported, on average, for every 4.5 practice years in England & Wales and 3.6 years in Scotland and death associated with general dental practice, on average, once in 758 and 464 years, respectively.
Similar content being viewed by others
Main
Medical emergencies will occur in general dental practice. The prevalence of such events has not been quantified in any study in the UK for more than 20 years. Changing demographics in the population, leading to increased longevity have resulted in more people having medical conditions which predispose to a medical emergency or are taking medication which may influence their dental management. In a study in the US, 77% of a sample of 3217 non-institutionalised persons aged 65 years or over were considered to be taking medication with a potential effect on dental care.1
Chapter 5 of the 'Poswillo report' stated that 'collapse can occur in a dental practice at any time',2 a sentiment echoed by General Dental Council guidelines.3 As James pointed out,4 the report does not expand on this point and offers no information on the incidence of collapse and death in the surgery not associated with general anaesthesia or sedation. The implication is clear that a visit to the dentist is potentially hazardous and that collapse is sufficiently common to justify much expense on training, drugs and equipment. The need for these recommendations, in the absence of facts showing the actual risks associated with routine dental treatment, has been called into question.4,5
Aims of the study
The study was carried out to ascertain:
-
A measure of the frequency of medical emergencies experienced by GDPs and how these events were managed
-
The emergency drugs and equipment GDPs possessed
-
How well prepared they felt to manage such events.
Method
One thousand questionnaires with a covering letter and reply-paid envelope were sent by post, via the Dental Practice Board (DPB) to a random sample of GDPs in contract with the National Health Service (NHS) in England & Wales in May 1996. Likewise, 500 questionnaires were sent to a random sample of GDPs in Scotland, also through the DPB, in August 1996. A second questionnaire, with a reminder letter and reply-paid envelope, was sent to those who did not reply to the initial questionnaire some 3 weeks later and, in England & Wales, a third questionnaire, again with a reply-paid envelope, was sent to those who did not respond to the first reminder. The anonymity of recipients was a precondition of participation of the DPBs. A pilot survey had been carried out of the 92 GDPs in contract with the NHS in the Doncaster Family Health Service Authority in 1995.
The questionnaire, shown as an appendix at the end of this paper, sought information on:
-
How long GDPs had been practising in the General Dental Service (GDS)
-
Whether they provided treatment under general anaesthesia (GA), intravenous sedation (IVS) or inhalation sedation (IS)
-
The nature of medical emergencies experienced over a 10-year period, or for as long as they had been practising if less than this
-
For each event: the location, stage of treatment, procedure being carried out, outcome
-
The emergency drugs and equipment possessed
-
How they ensured that the emergency drugs were maintained within their 'use by' date
-
Treatment provided and drugs used in management of emergency events reported
-
Whether they had received training as undergraduates to manage medical emergencies, what this involved and how well prepared they felt to manage an emergency upon graduation
-
Whether they had received such training since graduation and what this involved
-
How competent they considered themselves currently to manage a medical emergency
-
How they felt their readiness could be improved.

It was, as far as possible, of the 'tick box' format but respondents were asked to state the outcome of any emergency events they reported and invited to make any pertinent additional comments. The emergency drugs and equipment asked about in the questionnaire were based on recommendations of the Dental Practitioners' Formulary6 and Scully and Cawson.7 Sampling in England & Wales represented some 6% of GDPs in contract with the NHS compared with 28% in Scotland.
One person (GJA) entered the coded data onto a Microsoft Excel spreadsheet with 10% of the data re-entered to ensure accuracy. It was adapted and transferred onto the Statistical Package for Social Sciences (for Windows) (SPSS Inc.) for further analysis. The data were analysed using non-parametric statistics as appropriate to test for differences between categories.
This is the first of three reports on the findings of the survey, the other parts will be presented in forthcoming papers. This part discusses the prevalence, nature and outcome of medical emergencies reported by GDPs in an attempt to assess more accurately the risks of routine dental treatment.
Results
Details of the samples are listed in Table 1: 1110 replies were received with a response of 74%. Seventeen questionnaires were not included in the analysis as they had not been completed, including a number returned as the recipient was no longer at the address, as well as three from orthodontic practitioners who stated that it was 'not relevant' to them. Analysis is based on assessment of 1093 completed forms. Four of the questionnaires had been torn up and stuck back together.
The questionnaire asked for details of emergency events experienced over the previous 10 years. An estimate of the total duration of dental practice experience represented in the survey was made by assuming 10 years' experience for each respondent in practice for longer than 10 years and as long as they had been practising if less than 10 years. In England & Wales, 701 stated when they commenced in practice and the total duration represented by them was 6062 years. Likewise in Scotland there were 2786 years of practice experience represented by 328 respondents. Thus a total of 8849 years of general dental practice experience was represented by 1029 (94.1%) respondents who stated when they commenced work in the GDS.
From the experience of the pilot study it was clear that vasovagal syncope with immediate recovery and presumed responses to intravascular administration of adrenaline-containing local anaesthetic were frequent events in general dental practice and took place with such frequency that respondents did not accurately enumerate their occurrence. Given the imprecise nature of data relating especially to faints, it was decided, after much deliberation, to exclude them from the analysis. No specific enquiry was made of either of these events, although they were reported by a number of respondents but were not quantified with any accuracy. One faint was reported which resulted in a fall, the patient sustaining facial lacerations and one followed IVS. These are recorded among 'other' events.
There were 1469 emergency events recorded by 748 respondents in England & Wales, a mean of 1.96 events per respondent (with a standard deviation of 2.76, a median of 1, a mode of 0 and a range of 0-33). In Scotland, 818 events were reported by 345 respondents, a mean of 2.37 events per respondent (standard deviation 3.67, median 1, mode 0, range: 0-32). There were statistically significantly more events reported in Scotland than in England & Wales (P = 0.009). A total of 325 respondents, in similar proportions in England & Wales, and Scotland (29.9% and 29.2%, respectively), reported no events and a further 54 (4.8% and 5.2%, respectively) reported only faints or reactions to adrenaline in local anaesthetic. The proportions of respondents carrying out treatment under IS, IVS and GA and those who stated that they had previously carried out treatment or reported events under GA is shown in Table 2.
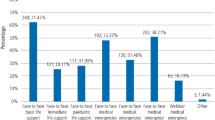
Figure 1 shows the proportion of each type of emergency as a percentage of the total of 1383 events reported in England & Wales, and 793 events in Scotland, for the events not associated with GA. Drug reactions accounted for 7.5% of events in England & Wales comprising anaphylaxis 2.9%, acute steroid insufficiency 0.6% and other drug reactions 4.0%. In Scotland they accounted for 5.8% — anaphylaxis 2.5%, acute steroid insufficiency 0.1% and other drug reactions 3.2%. These other drug reactions included unspecified reactions to local anaesthetic agents (25% in England & Wales and 8.7% in Scotland), allergy to penicillin (16.1%, 8.7%) and other allergic reactions (3.6%, 43.5%), however, the cause was not stated in a number of cases (25%, 21.7%). Other events reported included a number of cases of hyperventilation, two reports of transient ischaemic attacks, four respiratory arrests (0.3% of events in England & Wales), one road traffic accident and an instance of a woman going into labour. Events associated with GA are displayed in figure 2, again as a proportion of the total. These accounted for 5.9% of the events reported in England & Wales and 3.1% in Scotland. Even though a number of serious events occurred, including a number of cardiac arrests, no deaths were reported.
The frequency of the occurrence of medical emergencies in general dental practice can be approximated from the information given by those respondents who stated when they commenced in practice. In England & Wales, there were 1341 events reported over 6062 years, on average one event every 4.5 years and in Scotland there were 782 events reported during 2786 years, one event every 3.6 years. The frequency of events per 40 years, an estimate of a dentist's working lifetime, are listed in Table 3 for events not associated with GA and in Table 4 for those associated with GA. There were 518 years of practice experience represented by those in England & Wales who stated that they carried out treatment under GA (or reported events associated with GA) and 431 years by those in Scotland. In England & Wales there were 86 emergency events reported, an average of one for every 6.0 years, and in Scotland 25 events were reported, one for every 17.2 years. However, one respondent in England & Wales reported 20 GA events.
Where details were provided, nearly four out of five events occurred in the dental surgery (79.6%), 15.6% occurring elsewhere in the dental practice with a minority (4.8%) in other locations, such as outside the surgery building or the patient's home. In Scotland four instances of cardiac arrest and one of a stroke were reported to have affected passers-by outside the dental surgery premises. Thirty-five events (3.3%) in England & Wales, including a number of reported instances of anaphylaxis and other less severe drug reactions, and seven events (1.3%) in Scotland were reported to have occurred at the patient's home. Virtually all GA events reported occurred in the surgery or recovery area.
Most commonly, events occurred during treatment (36.7%), nearly a quarter (23.1%) occurred before treatment, 20.1% after administration of the local anaesthetic and 16.4% after the clinical procedure. A number of events were reported some time after the procedure (see above), when the patient had got home. Thirty-eight events in England & Wales (2.6%) and eighteen in Scotland (2.2%) affected persons who were not actually undergoing treatment, including those accompanying patients, passers-by and five members of dental staff, including a dentist and a technician. All the GA events took place at the time of the procedure or soon thereafter.
The majority of events took place during conservative procedures (52.2%) and dentoalveolar surgery (23.5%). Virtually all other types of treatment were implicated in a minority of events: including fourteen (1.1%) during the course of orthodontic treatment. There were ten events in England & Wales associated with IVS: a seizure, two diabetic events, three asthma attacks, two cases of respiratory arrest, a case of 'heart block' and a case of laryngospasm. In Scotland there were three: a seizure; an asthma attack and a faint after the procedure. No events were associated with IS.
Comparison was made between those who carried out treatment under GA, IVS and IS and those who did not in terms of the number of emergency events reported. In England & Wales, those carrying out treatment under all three modalities recorded statistically significantly more events than those who did not (GA: P < 0.001, IVS: P = 0.028, IS: P = 0.023). In Scotland, there was only a statistically significant difference in number of events reported by those carrying out IVS (GA: P = 0.437, IVS: P = 0.026, IS: P = 0.722).
Figure 3 shows the outcome of events not associated with GA and figure 4 the outcome of GA events. While no details were given in about a quarter of the events reported, 23.0% of patients were referred to hospital, in more than a third (36.3%) of these for radiography for assessment of a swallowed foreign body, or rarely, an inhaled foreign body (0.5%). In 38.5% of cases some sort of action was taken in management of the event (discussed in detail in Part 2 of this series) and in 3.8% of situations patients were referred to their general medical practitioner for further management.
Ten deaths resulted from the 1469 events reported in England & Wales (0.7%) and ten in Scotland from 818 events reported (1.2%). Table 5 shows that these were associated with cardiac arrest (14), myocardial infarction (4) and cerebrovascular accident (2). However, in four of the fatalities reported in Scotland, the victims were not patients but passers-by. Taking this into account, fatalities resulted from about 0.7% of emergencies in both England & Wales and Scotland. Considering the deaths reported by those who stated when they commenced in practice, there were eight deaths reported by respondents in England & Wales and six (as well as the three which befell passers-by) by respondents in Scotland. Thus the frequency with which a death was experienced in association with dental practice in England & Wales was one for every 758 practice years, a 1:19 risk of encountering a death during a 40-year career and one in 464 practice years in Scotland, about a 1:12 risk.
Discussion
The occurrence of medical emergencies in dental practice is a subject which has received scant attention in the dental literature during the past 20 years. This may be due, at least in part, to the difficulty in procuring meaningful and reliable data on this issue. Any study in this area, either prospective or retrospective, must be both large enough and cover sufficiently long a period of time to produce worthwhile information. A prospective study would require a monumental feat of organisation, keeping track of participants' whereabouts for the duration of the study, a need for persistent reminders to them to record events and anonymity would necessarily be lost, which might lead some to be economical with the truth on this potentially sensitive issue. Retrospective studies, comparatively easier to organise, suffer from a total reliance on participants for the interpretation and accurate recollection of the circumstances surrounding the onset, management and outcome of any incident over a period of a number of years. Vagaries of memory, especially in recollection of less major events, will almost certainly lead to inaccuracies of the information presented. A retrospective postal questionnaire study appeared to be the only means by which enough information could be gathered in a reasonable time.
The importance of achieving adequate response rates in postal questionnaire studies to avoid bias has been recently highlighted.8 In England & Wales a response rate of 75% was achieved after two reminders were sent, and in Scotland, where a single reminder was sent, the response rate was 70% giving an overall response rate of 74% which is considered 'acceptable'.9 It was intended, with the use of reply-paid envelopes, to make responding to the survey as easy as possible. This is the first national survey on this subject, comparing favourably with other surveys on this and related subjects, where response rates of 20%,10 25%,11 and 65%,12 have been reported. A high response rate may also reflect respondents' interest in this subject, given the potentially sensitive nature of the enquiry. Sackett defined bias as 'any process at any stage of inference which tends to produce results or conclusions that differ systematically from the truth'.13 Another potential source of bias in this study was in determining what respondents had written as, in some instances, this was open to interpretation. At least if one person entered the data, it would all be interpreted similarly.
The use of 'practice years' in the analysis takes no account of how many days of the year were worked or how many patients were seen per day or week, and no enquiry was made on these points. However, it is likely that with the large samples used, the average number of patients seen by dentists in the sample would approximate to mean number of patients seen by the 'average dentist', so beloved of the NHS. Listing the 'number of events per year' (or years per event) does provide an indication of the frequency of events and has allowed comparisons to be made with other studies.
No specific enquiry was made of GDPs' experience of faints. It appears that these events were frequent, as they were unreliably quantified, with responses such as '2-3 per year', '100-150' or 'lots'. They appear to have been managed well, as no untoward sequelae were reported. As fainting is a relatively common event, it was considered unreasonable to ask GDPs to guess their numbers over a 10-year period.
Other than faints, the most commonly experienced emergency event was a seizure, accounting for about a third of all events recorded. It is possible that some of the recorded seizures were actually related to the hypoxia which may accompany a faint. The next most common events were swallowed foreign bodies, hypoglycaemia, chest pain associated with angina pectoris and events associated with diabetes. Thus safe and effective management of such events in dental practice should form an important component of education in management of medical emergencies.
A medical emergency occurred in general dental practice according to this survey, on average between once in 3.6 and 4.5 years of practice and a death between once in 464 and 757 years of practice. This suggests that a GDP will see, on average between 9 and 11 medical emergencies in a practice lifetime of 40 years. In England & Wales there were, on average 2.8 episodes of seizure, 0.9 of angina pectoris, 0.1 of myocardial infarction and 0.09 of a stroke reported in the 40 years of a working career. Correspondingly, in Scotland there were 4.0 episodes of seizure, 1.3 of angina pectoris, 0.1 of myocardial infarction and 0.06 of a stroke in a 40-year working career. In a recent national survey of 1250 Australian GDPs, there was reported the equivalent of respectively 1.52, 1.01, 0.08 and 0.05 for these events,12 figures of a similar order of magnitude.
This survey collated information from the 5 years before and after publication of the 'Poswillo report' and shows that some practitioners had ceased to provide general anaesthesia during this period. The trend of fewer GDPs equipping their surgeries to Poswillo standards to provide GA treatment, has been identified previously14 and may reflect the continued move away from GA in general dental practice. GA was provided by 8.4% of the sample in Scotland, less than the 13% reported in 1993-4,5 nonetheless a higher proportion in Scotland than in England & Wales, perhaps a reflection of a higher demand in a population with relatively poorer oral health.
While nearly four out of five emergency events were reported to have occurred in the dental surgery itself, it is notable that about one in six took place elsewhere in the practice premises, such as the waiting room or reception area. Another feature was the late occurrence of some events: 42 incidents actually occurred after the patient had reached home. The majority of these were drug reactions (including what was reported as anaphylaxis) but fortunately none of these resulted in a fatality. It is advisable therefore to counsel patients to contact the surgery immediately should any adverse reaction occur following treatment, particularly following the administration of any drug and that arrangements exist and are explained to patients for out-of-hours cover.15
Many emergency events occurred during the treatment procedure — 36.7% of those reported. Certain incidents (eg ingestion or inhalation of a foreign body) are most likely to happen at this point. It is also likely that patients spend the majority of their time in the practice undergoing the treatment procedure, but emergency events are reported at all stages of a visit to the dental practice. A total of 56 emergency events affected persons other than the patient, including at least 14 who were passers-by. These included a number of cardiac arrests for which assistance was offered. The General Medical Council now lays down guidelines to medical practitioners stating that 'In an emergency, you must offer anyone at risk the treatment you could reasonably be expected to provide'.16 While such a recommendation does not currently exist for the dental profession, it is apparent from the results of this study that GDPs are using skills in basic life support for patients wherever the need is encountered.
More than half the emergency events occurred during restorative procedures (52.2%), most likely because of the large amount of surgery time devoted to such procedures. Dentoalveolar surgery was associated with nearly a quarter of events, perhaps as a result of greater psychological and physiological stress. Other areas of general dental treatment are much less commonly implicated. There were few events associated with IVS but these included two instances of respiratory arrest, indicating the importance of adequate preparation to manage such events by those using this technique.
It is remarkable that those providing treatment under GA, IVS and IS, in England & Wales at least, recorded more events — and fewer reported no events — than those who did not. However, one person reported 20 episodes of respiratory obstruction associated with GA but gave no details of any of them. In both England & Wales and Scotland, those providing IVS reported more events than those who did not, even though events associated with IVS comprised only 0.7% (of non-GA events) in England & Wales and 0.3% in Scotland, and there were no events associated with IS.
That two-thirds of respondents reported one or more medical emergencies emphasises the need for the whole dental team — reception staff, nurses, hygienists, as well as dentists — to be trained in management of these events. Peskin and Siegelman made the point that there is a general assumption that patients seeking dental treatment do so on the implied understanding that the dentist is capable of managing any event which may result from treatment or occur at or around the time of treatment.17 Even though emergency events are uncommon, the evidence presented here suggests that there is a need for GDPs to be prepared to manage a medical emergency. Serious events are rare but they do occur, therefore a well rehearsed routine for assessment, calling for help and initiating cardiopulmonary resuscitation (CPR), where appropriate, are all essential. This is reinforced by the fact that all the deaths reported in this survey involved cardiovascular events and all but two were of cardiac origin, thus basic life support for cardiac emergencies is confirmed as a training necessity for the entire team in dental practice.
Conclusions
Medical emergencies in general dental practice in Great Britain are rare events, occurring with an average frequency of between one in 3.6 and 4.5 practice years, or, on average, between nine and eleven emergency events per practising lifetime of 40 years. Events were more frequently reported in Scotland than in England & Wales. The most commonly reported event was a seizure. In England & Wales, significantly more emergency events were reported by those carrying out treatment under GA, IVS and IS, and in Scotland those providing IVS. Death associated with general dental practice is very rare: in this study one death was reported per 464-758 practice years, translating into a risk of experiencing a death of 1 in 12-19 practising lifetimes of 40 years, with a greater frequency in Scotland. None of the deaths reported in this study occurred in association with general anaesthesia. An emergency most frequently occurs during treatment in the dental surgery and most often during conservative treatment and dentoalveolar surgery.
These findings show the importance of acquiring and maintaining skills for the management of medical emergencies, as outlined in the General Dental Council recommendations.3 This should involve the whole dental team, which must be capable of early recognition of an adverse occurrence, calling promptly for assistance and the rapid institution of appropriate management.
References
Levy S M, Baker K A, Semla T P, Kahout F J . Use of medications with dental significance by a non-institutionalised elderly population. Gerodontics 1988; 4: 119–125.
Poswillo D E (Chair) . Standing Dental Advisory Committee. General anaesthesia, sedation and resuscitation in dentistry: report of an expert working party. London: HMSO, 1990.
Maintaining standards — guidance to dentists on professional and personal conduct. London: General Dental Council, November 1997.
James D W . General anaesthesia, sedation and resuscitation in dentistry. Br Dent J 1991; 171: 345–347.
Macpherson L M D, Binnie V I . A survey of general anaesthesia, sedation and resuscitation in general dental practice. Br Dent J 1996; 181: 199–203.
British Dental Association, British Medical Association, Pharmaceutical Society. Dental practitioners' formulary 1996-1998, together with the British national formulary No 32 (September 1996). BMA & Pharmaceutical Press, 1996.
Scully C, Cawson R A . In Medical problems in dentistry. p550. 3rd ed. Bristol: Wright, 1993.
Rugg-Gunn A . Scientific validity? (editorial). Br Dent J 1997; 182: 41.
Guidelines for acceptable response rates in epidemiological surveys. Br Dent J 1997; 182: 68.
Young T M . Questionnaire on the need for resuscitation in the dental surgery. Anaesthesia 1975; 30: 391–401.
Fast T B, Martin M D, Ellis T M . Emergency preparedness: a survey of dental practitioners. J Am Dent Ass 1986; 112: 499–501.
Chapman P J . Medical emergencies in dental practice and choice of emergency drugs and equipment: a survey of Australian dentists. Aust Dent J 1997; 42: 103–108.
Sackett D L . Bias in analytic research. J Chron Dis 1979; 32: 51–63.
Hastings G B, Lawther S, Eadie D R, Haywood A, Lowry R, Evans D . General anaesthesia: who decides and why? Br Dent J 1994; 177: 332–336.
Developing emergency services in the community: the final report. London: Department of Health, 1997, publication no. EL(97)46.
Duties of a doctor: good medical practice. London: General Medical Council, 1997.
Peskin R M, Siegelman L I . Emergency cardiac care. Moral, legal and ethical considerations. Dental Clinics of N America 1995; 39: 677–688.
Author information
Authors and Affiliations
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Atherton, G., McCaul, J. & Williams, S. Medical emergencies in general dental practice in Great Britain Part 1: their prevalence over a 10-year period. Br Dent J 186, 72–79 (1999). https://doi.org/10.1038/sj.bdj.4800023
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4800023
This article is cited by
-
Prevalence of medical emergency events in primary dental care within the UK
British Dental Journal (2023)
-
Comparison of different feedback modalities for the training of procedural skills in Oral and maxillofacial surgery: a blinded, randomized and controlled study
BMC Medical Education (2020)