Abstract
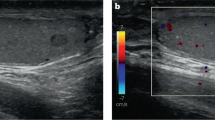
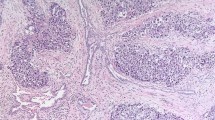
Despite the high incidence of prostatic adenocarcinoma and its ability for wide dissemination, metastatic involvement of testis is rather uncommon. We report two cases (aged 76 and 55 years, respectively), where unilateral testicular metastasis was incidentally discovered after bilateral orchiectomy following detection of adenocarcinoma prostate in six-quadrant trucut specimen. Both patients had obstructive voiding symptoms, hard nodular prostate on direct rectal examination and raised serum prostate-specific antigen levels, without associated systemic or testicular symptoms. Extensive evaluation excluded any other possible primary, although axial skeletal metastasis was detected on radionucleotide bone scans, in the first case. These cases highlight the need for proper evaluation of testes and para-testicular structures, for accurate staging of these tumors and to exclude any possible metastasis.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Dutt N, Bates AW, Baithun SI . Secondary neoplasms of the male genital tract with different patterns of involvement in adults and children. Histopathology 2000; 37: 323–331.
Schneider A, Kollias A, Woziwodzki J, Stauch G . Testicular metastasis of a metachronous small cell neuroendocrinic prostate cancer after anti-hormonal therapy of a prostatic adenocarcinoma. Case report and literature review. Urologe A 2006; 45: 75–80.
Anastasiadis AG, Ebert T, Gerharz CD, Ackermann R . Epididymal metastasis of a prostatic carcinoma. Urol Int 1998; 60: 124–125.
Thon W, Mohr W, Altwein JE . Testicular and epididymal metastasis of prostate cancer. Urologe A 1985; 24: 287–290.
Zrara I, Touiti D, Rimani M, Jira H, Beddouch A, Oukheira H et al. Testicular metastasis of prostatic adenocarcinoma: report of 2 cases. Ann Urol (Paris) 2000; 34: 200–202.
Gaskin DA, Shah D . Bilateral epididymal metastases from primary adenocarcinoma of the prostate. West Indian Med J 2003; 52: 253–254.
Inaba Y, Okamoto M, Harada M, Sakaue M, Maeda S . Prostatic carcinoma with bilateral testicular metastasis: a case report. Hinyokika Kiyo 1994; 40: 249–252.
Heidrich A, Bollmann R, Knipper A . Testicular metastasis of prostatic carcinoma 3 years after subcapsular orchiectomy. A case report. Urologe A 1999; 38: 279–281.
Gunlusoy B, Arslan M, Selek E, Cetinel M, Ayder AR, Cicek S . A case report: prostatic carcinoma with metastasis to the testicle. Int Urol Nephrol 2004; 36: 63–64.
Tu SM, Reyes A, Maa A, Bhowmick D, Pisters LL, Pettaway CA et al. Prostate carcinoma with testicular or penile metastases. Clinical, pathologic, and immunohistochemical features. Cancer 2002; 94: 2610–2617.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Deb, P., Chander, Y. & Rai, R. Testicular metastasis from carcinoma of prostate: report of two cases. Prostate Cancer Prostatic Dis 10, 202–204 (2007). https://doi.org/10.1038/sj.pcan.4500942
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.pcan.4500942