Abstract
The transcription factor nuclear factor kappa B (NF-κB) can intervene in oncogenesis by virtue of its capacity to regulate the expression of a plethora of genes that modulate apoptosis, and cell survival as well as proliferation, inflammation, tumor metastasis and angiogenesis. Different reports demonstrate the intrinsic activation of NF-κB in lymphoid and myeloid malignancies, including preneoplastic conditions such as myelodysplastic syndromes, underscoring its implication in malignant transformation. Targeting intrinsic NF-κB activation, as well as its upstream and downstream regulators, may hence constitute an additional approach to the oncologist's armamentarium. Several small inhibitors of the NF-κB-activatory kinase IκB kinase, of the proteaseome, or of the DNA binding of NF-κB subunits are under intensive investigation. Currently used cytotoxic agents can induce NF-κB activation as an unwarranted side effect, which confers apoptosis suppression and hence resistance to these drugs. Thus, NF-κB inhibitory molecules may be clinically useful, either as single therapeutic agents or in combination with classical chemotherapeutic agents, for the treatment of hematological malignancies.
Similar content being viewed by others
Introduction
Nuclear factor kappa B (NF-κB) was initially identified as a transcription factor present in the nucleus of B cells that bound to the enhancer of the κ light chain of immunoglobulins.1 NF-κB stimulates the expression of a panel of antiapoptotic gene products including FLICE inhibitory protein (FLIP), cIAP, survivin, B-cell leukemia/lymphoma 2 (Bcl-2), and Bcl-XL, underscoring its importance on cell death in hematologic malignancies (Table 1). In addition, NF-κB modifies the expression of numerous other target genes that are unrelated to cell death and affect inflammation, proliferation, or differentiation. NF-κB also enhances the expression of mdr1, whose product, P-glycoprotein (P-gp), a plasma membrane transporter, mediates chemoresistance by inducing the efflux of chemotherapeutic molecules, explaining its broad impact, not only in oncogenic transformation but also in chemoresistance.2
NF-κB consists of a family of Rel-domain-containing proteins including Rel A (p65), Rel B, c-Rel, p50 (NF-κB1), and p52 (NF-κB2).3, 4 Phosphorylation-dependent cleavage of inactive p100 yields active p52, while cleavage of p105 yields p50.5 Ankyrin-domain containing proteins, like IκBα, IκBβ, IκBγ, Bcl-3, p105, and p100, are responsible for withholding NF-κB subunits in the cytoplasm.3 The inactive, latent form of NF-κB is localized in the cytoplasm and is constituted by a heterotrimeric complex of p50, p65, and IκB.4, 5 Degradation of IκBα by sequential phosphorylation, ubiquitination, and proteasome-mediated proteolysis releases the p50–p65 heterodimer, which translocates to the nucleus and binds to specific consensus sequences within the promoter of NF-κB target genes.3, 5 NF-κB transactivates more than 200 genes implicated in cell survival/apoptosis, cell growth, immune response, and inflammation.3 The principal NF-κB activation pathway involves IκB phosphorylation at serine residues 32 and 36 by IκB kinase (IKK), which is formed by the IKKα, IKKβ, and IKKγ (NF-κB essential modulator (NEMO)) subunits.1 IKK can be activated by multiple intra- and extracellular stimuli6 (Figure 1).
Pathways of NF-κB activation and their subversion in hematological malignancies. The principal (canonical and alternative) NF-κB activation pathways are depicted. Blue rectangles indicate frequent mechanisms accounting for constitutive NF-κB activation. For details consult main text. BAFF, B-cell activating factor; CD40L, CD40 ligand, IκB, inhibitor of NF-κB; IKK, IκB kinase; IL, interleukin; IRAK, IL-1R-associated kinase; FADD, Fas-associated death domain protein; LPS, lipopolysaccharides; LTβ, lymphotoxinβ; NEMO, NF-κB essential modulator; NF-κB, nuclear factor kappa B; NIK, NF-κB-inducing kinase; RIP, receptor interacting protein; TLR, toll-like receptor; TNF, tumor necrosis factor; TRADD, TNF receptor-associated protein with a death domain; TRAF, TNF receptor-associated factor; Ub, ubiquitin
The NF-κB family members c-Rel and v-Rel have been identified as bona fide oncogenes.7 c-Rel is known for its potential to transform cells in culture, and it is frequently amplified in Hodgkin's lymphomas (HLs), diffuse large B-cell lymphomas (DBCLs), and some follicular and mediastinal B-cell lymphomas.8 A viral ortholog of c-Rel, v-Rel, induces lymphomas and leukemias in animal models.9 Constitutively active NF-κB has been detected in malignant cells derived from patients with multiple myeloma (MM), acute myelogenous leukemia (AML), acute lymphocyte leukemia (ALL), chronic myelogenous leukemia (CML), and most recently in myelodysplastic syndromes (MDS).10 Targeting NF-κB in these hematopoietic malignancies leads to apoptosis, corroborating the role of NF-κB in the survival and clonal expansion of malignant cells.
In this review, we will summarize novel insights into the pathophysiology of NF-κB in hematologic malignancies and evaluate the prospects for developing new NF-κB-targeted treatments.
Constitutive Activity of NF-κB in Hematologic Malignancies
Lymphoid malignancies
Hodgkin's lymphoma
HL is defined by the presence of Hodgkin and Reed–Sternberg (HRS) cells derived from clonal expansion of germinal-center B cells. The involvement of Epstein–Barr virus (EBV) in the pathophysiology of HL has been shown in about 50% of cases in industrialized countries.11 The constitutive activity of NF-κB has first been shown for HRS cell lines12 and then in primary HRS cells.13 Specifically, the transcriptionally active homodimer p50 accounts for constitutive NF-κB activation in HRS cells.14 A large number of studies addressed the mechanisms underlying constitutive NF-κB activity in HL. Autonomously active surface receptors, including CD30, CD40, receptor activator of NF-κB (RANK), and Notch 1, have been implicated in NF-κB activation in HRS.11 Alternatively, or in addition, EBV might mediate NF-κB activation through virally encoded genes such as latent membrane protein (LMP)1, LMP2a, and EBV nuclear antigen (EBNA), whose transcription has been detected in HRS cells.15 In particular, LMP1 can mimic CD40 signaling, and this could explain how latent EBV infection causes the upregulation of antiapoptotic target genes via NF-κB.16 In EBV-negative HL, other mechanisms have been suggested to explain constitutive NF-κB activity in HRS cells. Thus, inactivating mutations in the IκB gene were found in several studies of EBV-negative HLs.17, 18 In one report, mutations in the IκB gene were found in all 11 EBV-negative HLs as well as in 4 of 15 EBV-positive HLs. As an alternative or additional mechanism of NF-κB activation, amplifications of the NF-κB/REL gene have been detected by fluorescence in situ hybridization (FISH) of the 2p13–16 locus in HL.19
In line with the probable relevance of NF-κB for HL pathogenesis, the antiapoptotic NF-κB target gene c-FLIP is constitutively expressed by HRS cells. The presence of c-FLIP may indeed inhibit transmission of proapoptotic signals via death receptors including CD95/Fas/Apo1, as suggested in a study of 59 HL patients.20 This study proposed that c-FLIP would be recruited into the CD95L-triggered death-inducing signaling complex (DISC), thus blocking proapoptotic signaling by the DISC.
Non-Hodgkin's lymphoma
Genetic alterations that affect the activity and expression of cellular NF-κB/REL proteins have been linked to non-Hodgkin's lymphomas, which can arise from malignant transformation of either B- or T-lymphocytes. The amplification of the human c-REL locus, which is localized in the 2p14–15 chromosomal region, was found in a series of non-Hodgkin's B-cell lymphomas, resulting in increased c-REL expression.21 However, no direct correlation between c-REL expression and the expression of antiapoptotic NF-κB target genes could be observed.5 Overexpressed c-REL is likely to be implicated in malignant transformation because it can transform primary chicken lymphoid cells in vitro.9 In contrast to c-REL, amplifications and/or chromosomal rearrangements affecting the REL A locus, which encodes the NF-κB p65 subunit, are rare in lymphomas.22 No genetic alterations of the REL B locus have been described.5 However, chromosomal rearrangements that affect the p52 (NF-κB2) locus at the 10q24 chromosomal region have been detected in T-cell non-Hodgkin's lymphomas, and also in chronic B-lymphocytic leukemia (B-CLL), and MM.23 All these rearrangements result in the deletion of C-terminal IκB-like sequences within the p100 and hence stimulate the constitutive transcriptional activity of p100-derived p52.
NF-κB activation has been extensively investigated for mucosa-associated lymphoid tissue (MALT) lymphomas. MALT lymphomas are the most common subtype of extranodal non-Hodgkin's lymphomas.24 These lymphomas are commonly observed in the context of chronic inflammation or autoimmune disease, in particular in the stomach, lung, and thyroid gland.25 Gastric MALT lymphoma often correlates with infection by Helicobacter pylori, and thyroid MALT lymphoma is observed in association with Hashimoto's thyroiditis.26 The most frequent chromosomal aberration associated with MALT is t(11;18)(q21;q21) translocation,27 which juxtaposes fragments of the gene encoding the inhibitor of apoptosis-2 (c-IAP2) gene on chromosome 11 and that encoding MALT lymphoma translocation gene 1 (MALT1) gene on chromosome 18.26 The resulting c-IAP2/MALT1 fusion protein can activate NF-κB.26 MALT1 contains a region with homology to caspases identifying MALT1 as a human paracaspase.28 The MALT1/paracaspase promotes the ubiquitination of NEMO, resulting in its activation and hence in that of NF-κB.29 A recent study performed on patient samples could demonstrate that the ubiquitin ligase activity of the MALT1/paracaspase targeting NEMO is deregulated by fusion with c-IAP2/MALT1.26
Burkitt's lymphoma (BL) is an aggressive B-cell malignancy that can be endemic in East Africa, always associated with Epstein–Barr virus (EBV) infection, or sporadic, in which case its association with EBV infection is less frequent.30 Classically, BL is associated with t(8;14)(q24;q32), in which the immunoglobulin promoter causes constitutive transcription of the c-myc oncogene.31 A recent study reported that, in EBV-positive BL, reactive oxygen species (ROS) and p38 MAPK mediated NF-κB activation. In contrast, EBV-negative BL cells failed to produce ROS and to activate MAPK or NF-κB, suggesting that BL can be classified into two distinct pathologies involving different signaling pathways.30
A plethora of reports implicate NF-κB signaling in the pathogenesis of DBCLs, which are thought to arise from normal antigen-exposed B cells in germinal centers (GCs) of secondary lymphoid organs,32 as inferred from gene profiling.33 Microarray data suggested a classification of DBCLs into germinal center-like and activated-B-cell (ABC)-like subtypes.34 DBCL cell lines with ABC-type signatures exhibit the constitutive activation of NF-κB target genes, as well as an increased sensitivity to cell death induction by NF-κB inhibition.35 Most recently, two large series of whole genome arrays led to the identification of three distinct DBCL subtypes: the oxidative phosphorylation, B-cell receptor/proliferation and host response (HR) subtypes.36, 37 The HR subtype exhibited a robust NF-κB target gene signature, while the activated B-cell (ABC)-like DBCLs had a more restricted NF-κB target gene signature that resembles that found during developmental maturation of normal B cells.36 Functional evidence establishing the precise role of NF-κB in DBCL subtypes is yet elusive. Amplification of the c-REL locus has been demonstrated in 23% of extranodal DBCLs.5 However, NF-κB activation in DBCLs can also been found in the absence of c-REL amplification, suggesting alternative mechanisms for constitutive NF-κB activation.5
The precise mechanisms, incidence, penetrance, and relevance of NF-κB activation remain to be characterized in most non-Hodgkin's lymphomas. An extensive gene profiling study revealed that NF-κB activation is common in non-Hodgkin lymphomas.38 In this report, the putative NF-κB target genes Bcl-2 and BIRC5/survivin were identified. BIRC5/survivin correlated with an aggressive phenotype, while Bcl-2 correlated with less aggressive lymphomas.
Multiple myeloma
MM is a clonal B-cell malignancy characterized by slowly proliferating secretory plasma cells in the bone marrow.39 Thus far, MM remains an incurable disease. Recently, two studies revealed the expression of constitutively active NF-κB in freshly drawn bone marrow aspirates from 37 of 37 MM patients.40, 41 Both studies demonstrated the retention of the NF-κB consensus sequence in nuclear extracts as well as translocation of the p65 subunit to the nucleus in highly purified CD138+ MM plasma cells. The underlying mechanisms for expression of constitutively activated NF-κB in MM cells are poorly understood. Two alternative, nonexclusive mechanisms could explain NF-κB activation in MM. First, NF-κB could be activated in an autocrine manner, because several NF-κB-inducing cytokines including tumor necrosis factor (TNF)-α, lymphotoxin (LT), IL-1, and RANKL are produced by MM cells and by the bone marrow microenvironment. Second, the IκBα gene can be mutated in MM patients.42
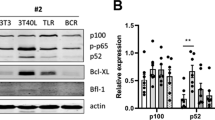
Interestingly, the interplay between intrinsically activated NF-κB and another antiapoptotic transcription factor, signal transducer and activator of transcription (STAT)3, may contribute to MM pathogenesis.42 As a possibility, NF-κB might upregulate the expression of interleukin-6 (IL-6), which in turn activates STAT3.40, 41 The expression of Bcl-XL, a prominent antiapoptotic Bcl-2 homolog, is induced by both STAT3 and NF-κB, and Bcl-XL overexpression has been demonstrated in MM cells at the protein level.42 The expression of Bcl-XL is negatively correlated with chemotherapy responses in MM. Indeed, objective responses to standard treatment regimens were observed in 83–87% of patients bearing Bcl-XL-negative MM. In contrast, only 20–31% of Bcl-XL-expressing MM did respond to chemotherapy.43
B-CLL
B-cell-derived chronic lymphocytic leukemia (B-CLL) is characterized by the accumulation of monoclonal CD19+/CD5+/CD23+ B lymphocytes arrested in the G0/G1 phase of the cell cycle.44 This accumulation is probably caused by reduced apoptosis rather than increased proliferation.44 One study demonstrated that unstimulated B-CLL cells obtained from patient samples exhibited higher levels of NF-κB activity than human B cells from healthy donors.45 As dominant NF-κB component's the transcriptionally active subunits p50, p65, and c-Rel were identified in this report. These results were confirmed by another study, which demonstrated constitutive NF-κB activity in malignant B-lymphocytes of 71 B-CLL patients.46 Additional studies revealed the importance of supportive interactions with a specific microenvironment for the survival of malignant B-CLL cells. One fundamental NF-κB-activatory stimulus in the bone marrow and in neoplastic follicles is mediated by a paracrine interaction between CD40L (on stroma cells) and CD40 (on tumor cells).45 It has also been shown that the functional interaction between CD40 and CD154 is essential for the transcriptional regulation and malignant B-cell survival in B-CLL. In those cases of B-CLL that are CD154+, addition of a neutralizing anti-CD154 mAb resulted in inhibition of NF-κB activity associated with subsequent cell death.47 Furthermore, survival kinases such as phosphatidylinositol-3 kinase (PI3-K) and Akt/protein kinase B may contribute to NF-κB activation. These pathways are constitutively activated in B-CLL upon CD40 crosslinking, leading to PI3-K-dependent Akt and NF-κB signaling.46 Vascular endothelial growth factor (VEGF), another factor of the microenvironment, implicated in increased neo-vascularization in B-CLL bone marrow, has been demonstrated recently to be potentially important for the pathogenesis and prognosis of B-CLL.47 B-CLL cells produce VEGF in vitro. High VEGF levels are found in the serum of patients. Moreover, an elevated expression of VEGF receptor (VEGFR)-2 on tumor cells correlated with shortened patient survival.48 It has been demonstrated that CD40 engagement by CD154 upregulates production of VEGF in B-CLL cells in an NF-κB-dependent fashion.47 In turn, VEGF favors the nuclear translocation of NF-κB in malignant B-CLL cells, suggesting the initiation of a positive feedforward loop in which NF-κB activation is amplified by VEGF in an autocrine manner.
In B-CLL cells, CD40 ligation induces the production of antiapoptotic proteins including inhibitors of apoptosis proteins (IAPs), while CD154 ligation induces survivin in a NF-κB-dependent manner.49 Furthermore, Bcl-XL expression in B-CLL cells is maintained through NF-κB and the expression of X-chromosome-linked inhibitor of apoptosis protein (XIAP) and FLIP in B-CLL has been linked to the constitutive PI3K-dependent NF-κB activation.46
ALL
B-precursor ALL is associated in 25–30% of adult cases, and 5% of childhood cases with the t(9;22) chromosomal translocation also found in 95% of chronic myeloid leukemia (CML, see below).50 This leads to the transcription of the Bcr/Abl fusion oncoprotein, a serine threonine kinase that activates NF-κB.51 NF-κB has been found to be activated in eight of eight Bcr/Abl+, but in none of three Bcr/Abl− B-precursor ALL blasts.52 IKK activity and IKKα expression levels were rather low in Bcr/Abl+ patient samples, pointing to an IKK-independent NF-κB activation. Ras mutations have been reported in B-precursor ALL patients,53 and Ras can mediate IKK independent p65 translocation to the nucleus.51
Human T-cell leukemia virus type I (HTLV-I)-induced adult T-cell leukemia (ATL) is an aggressive malignancy with poor prognosis. It arises from CD4+ T lymphocytes infected by HTLV-I.54 In all, 3–5% of HTLV-1-infected individuals develop ATL after a prolonged incubation period of 40–60 years,55 presumably due to secondary mutations that accumulate to transform HTLV-1-infected cells. It is thought that the HTLV-encoded 40 kDa transactivator protein Tax mediates leukemic transformation in concert with Ras oncogene.56 Tax induces NF-κB,57 which can cause upregulation of the protein subunit of telomerase, human telomerase reverse transcriptase (hTERT), thus promoting long-term proliferation of genomically instable cells.58 Tax expression can promote phosphorylation and activation of IKKα and IKKβ by the kinase NF-κB-inducing kinase (NIK), and/or can directly bind to IKKγ.59, 60 Constitutive NF-κB has also been detected in HTLV-1-negative ATL, indicating the existence of Tax-independent mechanisms of NF-κB activation.61 The expression of the NF-κB target genes XIAP, survivin, Bcl-2, and Bcl-XL has been measured in primary ATL cells.54, 62 XIAP expression can be induced in a Tax-dependent manner, and survivin predicts poor outcome since it is highly expressed in the most aggressive type of ATL.62
Myeloid malignancies
Myelodysplastic syndromes
MDS are clonal stem cell disorders with different characteristics at the early and the late stages of the disease. Early MDS is associated with peripheral cytopenias, which can be explained by an increased apoptotic turnover of hematopoietic stem cells and differentiating myeloid cells in a hypercellular bone marrow. Late-stage MDS is marked by a progressive increase of immature cells and frequent transformation to AML, presumably due to a progressive suppression of programmed cell death and increased clonal proliferation. Two studies performed on a limited number of patients did not reach a consensus on the status of intrinsic NF-B activity in MDS.63, 64 Two recent studies performed on 2465 and 55 MDS10 patients clearly revealed that the degree of NF-κB activation correlated with the risk of progression to AML, both in transversal and in longitudinal studies.
The most exhaustive study, which was performed in our laboratory, clearly demonstrates that intrinsic NF-κB activation is a hallmark of high-risk MDS. NF-κB activity was evaluated in mononuclear cells and purified CD34+ hematopoietic stem cells from the bone marrow of low- and high-risk MDS patients, either by EMSA or by immunofluorescent detection of the subcellular localization of NF-κB subunit p65. Significant NF-κB activation was only detected in high-risk MDS as opposed to low-risk MDS. NF-κB activation and translocation of p65 were detected in mononuclear cells as well as in CD34+ hematopoietic stem cells and CD33+ myeloid cells and strongly correlated with bone marrow blast counts.10 Combined immunohistochemical detection of p65 and FISH detection of common MDS-associated cytogenetic alterations revealed that NF-κB activation was strictly restricted to mutated cells and hence was an intrinsic characteristic of malignant stem cells (as opposed to nonmutated stroma cells)10 (Figure 2).
Correlation between cytogenetic abnormalities associated with MDS and NF-κB activation at the single-cell level. Bone marrow aspirates from MDS patients were subjected to cytohistochemical detection of p65 (grey), followed by FISH for the detection of chromosomes 7 (red) and 8 (green) in (a) and (b). Representative images of euploid cells (two chromosomes) with cytoplasmic p65 and aneuploid cells (one chromosome 7 in A or three chromosomes 8 in b) with nuclear p65 are shown
Our results contrast with another recent study suggesting that TNF-α functions as a potent NF-κB inducer in late-stage MDS.65 This assumption was based on the correlation between the relative expression level of two TNF-α R subunits (R1 or p55 versus R2 or p75) and the degree of NF-κB activation in MDS. In patients where R1 predominated over R2, NF-κB activation was maximal.65 This can be correlated with fundamental studies suggesting that TNF-α R1 (p55) preferentially induces caspase-dependent apoptosis via the extrinsic TNF receptor-associated protein with a death domain (TRADD)/Fas-associated death domain protein (FADD)/caspase-8/caspase-3 pathway (which would be incompatible with NF-κB activation),66 while TNF-α R2 (p75) would activate NF-κB.65 Thus, this study insinuates that NF-κB activation involve a paracrine (and hence non-cell autonomous) contribution and also suggests that changes in TNF-α R1/R2 expression might be involved in disease progression.
To reconcile these two distinct theories explaining NF-κB activation in MDS (cell autonomous10 and TNF-α-driven65), one might invoke two distinct possibilities. Either, cytogenetic alterations (and secondary mutations?) could drive both NF-κB activation and differential TNF-α-R subunit expression as independent consequences, or the mutational profile of MDS blast would condition TNF-α-R subunit expression, which in turn would determine the intrinsic capacity of MDS blasts to respond to their microenvironment (which contains TNF-α) to activate NF-κB.
The more extensive studies on MDS and NF-κB differ from two previous reports in which no correlation with the French American British group (FAB) classification for MDS64 or no evidence for NF-κB activation could be found in bone marrow cells derived from MDS patients.63 In those earlier reports NF-κB activity had not been investigated at the stem cell level and the study was not made on purified blast populations from the bone marrow of MDS patients. These technical aspects coupled to lower patient numbers may have accounted for the failure to detect a correlation between disease progression and NF-κB activation.
A number of apoptosis-regulator NF-κB target genes, including Bcl-2, Bcl-XL, c-IAPs and FLIP have been correlated with clinical progression of MDS.67, 68, 69 Indeed, the expression of proapoptotic proteins of the Bcl-2 family like Bak, Bad, and Bcl-XS has a favorable prognostic value in MDS, while the expression of antiapoptotic proteins like Bcl-2 and Bcl-XL is associated with unfavorable prognostic value, suggesting that apoptosis suppression could be implicated in the transformation of MDS to AML.68 XIAP overexpression has also been implicated in apoptosis suppression and transformation of MDS to AML.69 A deregulation of FLIP and its splice variants in MDS bone marrow has also been shown recently.65, 70 FLIPLong levels correlated negatively with apoptosis, and expression of FLIPLong increased while levels of FLIPShort decreased with progression of MDS, leading to an increase in the FLIPLong/FLIPShort ratio. Determination of mRNA levels for FLIPLong and FLIPShort in patient bone marrow cells in a further study revealed that the FLIPLong/FLIPShort ratio positively correlated with the levels of NF-κB activity, suggesting its implication in apoptosis suppression during progression of MDS to AML.65, 67
Acute myeloid leukemia
AML represents a heterogenous group of clonal stem cell malignancies arising from so-called leukemic stem cells (LSC).70, 71, 72 LSC give rise to leukemic myeloid blasts arrested at different72 maturation steps. High proliferation rates of LSC are responsible for invasion of the bone marrow and are associated with fatal outcome. Several studies have characterized the activation level of NF-κB in bone marrow of AML patients and more precisely in LSC. Two reports demonstrated intrinsic activity of NF-κB in CD34+/CD38−/CD123+ in 11 and 13 AML patients, respectively.72 The first study revealed the nuclear translocation of the transcriptionally active NF-κB subunits p65 and p50. Of 30 AML cases, 14 showed constitutive activation of the NF-κB transcription factor complex composed by p65 and p50, but no correlation between blast counts and NF-κB activity could be established.63 This contrasts with a recent report in which NF-κB activation levels were observed to increase in proportion to peripheral blood blast counts.73 The molecular mechanism of NF-κB activation in LSCs or AML blasts remains elusive. Constitutive activation of the NF-κB complex via dysregulation of IKK signalling has been described recently in LSC and AML blasts from the bone marrow and peripheral blood in two studies enrolling 3574 and 18 patients, respectively.73 One report provided evidence for high IKK kinase activity leading to NF-κB activation independently from IκBα expression.74 The second report revealed that specific targeting of IKKβ with a pharmacologic inhibitor could block constitutive NF-κB activity leading to apoptosis via hypophosphorylation of IKKβ, underlying the role of IKK as pacemaker for constitutive NF-κB activity in LSC and AML blasts.73 Meanwhile, the reasons for IKK activation in AML are still to be elucidated. The cytokine interleukin 1β (IL-1β) has also been implicated in the activation of NF-κB in AML cells, possibly in an auto-amplification loop in which NF-κB stimulates IL-1β expression, which in turn activates NF-κB, that would be responsible for the proliferation of AML cells.70, 75
Not surprisingly, there is evidence that antiapoptotic NF-κB-regulated gene products play a major role in apoptosis regulation in LSC and AML blasts. As shown recently, Bcl-2 is expressed in AML with a particularly aggressive, apoptosis-resistant phenotype.63 Furthermore, indirect NF-κB inhibition by means of the proteasome inhibitor MG-132 decreased the expression of the antiapoptotic genes c-IAP2 et Bcl-XL.72
Myeloproliferative disorders
Myeloproliferative disorders (MPD) represent a group of clonal haematopoietic stem cell diseases caused by progenitors that are hypersensitive to or independent from cytokines that are normally required for their proliferation and differentiation.50 These progenitors derive mostly from the myeloid lineage and proliferate continuously, while reaching some degree of maturation (which is not the case in AML). Typical MPDs include CML as well as polycythemia vera, essential thrombocythemia, and idiopathic myelofibrosis (IMF).50 While the pathophysiology of most MPDs is still elusive, the molecular basis of CML is now well established.
CML
CML is a typical MPD characterized by the chromosomal translocation 9;22 leading to expression of the Bcr/Abl fusion oncoprotein that exhibits constitutive kinase activity.50 Bcr/Abl kinase signaling leads to activation of different survival pathways, including that of NF-κB.51, 76 Activation of NF-κB by the Bcr/Abl fusion oncoprotein results in increased translocation of the transcriptionally active subunit p65 to the nucleus, probably due to p65 hypophosphorylation that occurs in an IKK independent manner.51, 76 These pathways lead to expression of antiapoptotic proteins like Bcl-XL, providing a growth advantage for clonal Bcr/Abl+ cells. Constitutive activation of NF-κB has been shown for late-stage CML in different studies.63, 76 One study demonstrated intrinsic activity of NF-κB in leukemic blasts of eight CML patients with relapsed disease before and during treatment with the tyrosine kinase inhibitor STI 571 (Gleevec®). Another report revealed the absence of significant nuclear activity of NF-κB in 15 CML patients monitored in the chronic/early disease stage, while two CML patients in advanced CML with blast crisis exhibited high intrinsic NF-κB activity in nuclear extracts.63 As activating Ras mutations are typical for late-stage CML77 and as Ras can induce IKK-independent translocation of p65 to the nucleus,78 activated Ras represents a possible candidate for activating NF-κB in progressive CML, marking the initiation of the blast crisis.
Idiopathic myelofibrosis
IMF is a rare clonal stem cell disorder marked by fibrotic destruction of the bone marrow, probably secondary to proliferation of the malignant clone of megakaryocytes that produces fibrotic cytokines such as transforming growth factor-β1 (TGF-β1).79 Recently, it has been reported that monocytes from IMF patients presented constitutive activation of NF-κB associated with TGF-β1 secretion.80 Another study demonstrated the spontaneous activity of the NF-κB pathway in IMF CD34+ cells and megakaryocytes and the implication of the immunophilin FK506-binding protein 51 (FKBP51), probably leading to activation of NF-κB composed by p65/p50 subunits.79 Inhibition of NF-κB activity by the NF-κB super-repressor did not alter resistance to apoptosis, but inhibited secretion of TGF-β1. As TGF-β1 is responsible for the development of marrow fibrosis, NF-κB is likely to play a cardinal role in the pathophysiology of IMF.
The implication of NF-κB in the pathogenesis of other MPDs is not well established. In one report, no evidence for NF-κB activation was obtained in two cases of essential thrombocythemia, whereas, ex vivo, two samples from patients with chronic myeloid leukemia presented NF-κB activation,79 as described by others.63 The exact molecular and cellular mechanisms activating NF-κB in MPDs remain obscure. Apoptosis resistance in IMF and polycythaemia vera is mediated via the janus kinase (JAK)2/STAT5 pathway.79, 81 A unique valine-to-phenylalanine substitution at amino acid position 617 in the JH2 pseudo-kinase domain of the JNK JAK2 gene leading to constitutive signaling has been found in more than 80% of polycythaemia vera patients and patients with other MPDs like IMF and essential thrombocythaemia.81 In view of the fact that sustained activation of JAK2 can activate the NF-κB pathway, at least in neurons,82 it can be speculated that constitute activation of mutated JAK2 favors NF-κB activation in MPDs as well.
Therapeutic Strategies Targeting NF-κB
As loss of IKKα or IKKβ function leads to defective activation of either the alternative or the classical NF-κB signaling pathway6 (Figure 1), IKKs constitute a promising drug target for cancer treatment. To date, no potent IKKα-selective inhibitors have been reported, perhaps related to the fact that the role of IKKα in NF-κB activation is still enigmatic. Several compounds, initially designed to inhibit IKK-β kinase activity, also inhibit IKKα in the low micromolar range.6 The dual involvement of IKKα in the classical p65/p50-dependent pathway (where it plays an auxiliary role) and in the alternative p52 (NF-κB2)-dependent pathway (where it plays an essential role) makes it a conceptually attractive drug target for the treatment of lymphoid and myeloid malignancies.6
Much effort has been undertaken to develop specific IKKβ inhibitors, and a limited number of reports have documented their efficacy in killing cancer cell lines and primary cells via apoptosis.73, 83, 84 The inhibition of IKKβ activity by the carboline derivative PS-1145 inhibits NF-κB activation, suppressing cytokine production and cell proliferation in MM.84 Another specific IKKβ inhibitor AS602868, an anilinpyrimidine derivate, was successfully tested on LSCs and peripheral blasts of 18 AML patients.73 Autophosphorylation of IKKβ was efficiently blocked, leading to NF-κB inhibition and consequent apoptosis.
Beyond specific small-molecule IKK inhibitors, antisense oligonucleotides and small interfering RNAs targeting IKKs or NF-κB subunits are being developed6, 10 (Figure 3). Moreover, cell-permeable peptides preventing the oligomerization and auto-activation of two subdomains of IKK-γ (NEMO) abrogate NF-κB activation and induce apoptosis in retinoblastoma cell lines.60, 85, 86, 87 It remains to be seen whether these technologies will open new perspectives for the treatment of hematologic malignancies.
An indirect strategy to target constitutive NF-κB activation has entered clinical trials for the treatment of MM. Bortezomib (Velcade®; Millenium, formerly known as PS341), a dipeptidyl boronic acid derivate, is a reversible inhibitor of the 26S proteasome, a multiprotein complex, that degrades ubiquitinated proteins.88 It has been shown that, in vitro, myeloma cells are up to 1000-fold more sensitive to apoptosis induced by bortezomib than normal plasma cells.84 Bortezomib exerts its apoptotic effects via inhibition of IκB degradation and subsequent inhibition of constitutive nuclear translocation of NF-κB subunits in MM cells. This abrogates the expression of antiapoptotic target genes.89 Bortezomib was evaluated in several clinical trials in relapsed and refractory MM, yielding response rates from 30 to 40%.90, 91 Bortezomib is approved by the FDA and by the European Regulatory Agency (EMEA) for the treatment of MM. Clinical trials are currently undertaken to evaluate its therapeutic potential in other hematologic malignancies. Objective responses have been observed for non-Hodgkin's lymphomas (including mantle cell lymphoma) and AML92, 93, 94 The recent observation that bortezomib induces apoptosis ex vivo in purified MDS hematopoietic stem cells suggests that bortezomib may be indicated in this disease as well as for AML patients10 (Figure 4). Of note, however, is that it is not clear whether the therapeutic effects of bortezomib are entirely due to inhibition of NF-κB or whether bortezomib may act on other relevant targets. Proteasomes selectively destroy a number of abnormal or unfolded proteins, which may be generated in increased amounts in cancer cells, especially in MM.95 Moreover, proteasomes degrade several proteins involved in cell-cycle control,96 again suggesting that the benefical effects of bortezomib could involve the accumulation of proteins that are not related to NF-κB. According to one study, bortezomib responses could be linked to the upregulation of the proapoptotic Bcl-2 protein family member NOXA93 (Figure 4).
Proapoptotic mode of action of bortezomib. The molecule inhibits NF-κB activation indirectly through an effect on the proteasome. In addition, it causes the accumulation of the proapoptotic Bcl-2 family member Noxa, which can stimulate mitochondrial membrane permeabilization with the consequent release of caspase-dependent or -independent proapoptotic factors. Note that the relative contribution of NF-κB, Noxa and yet-to-be-discovered proapoptotic mechanisms to Noxa-induced cell death is yet to be determined. Cyt c, cytochrome c; EndoG, endonuclease G; AIF, apoptosis-inducing factor
A different approach to inhibit constitutive NF-κB activation may be to interfere with NF-κB binding to DNA by means of phosphorothioate oligonucleotides that mimic the NF-κB consensus binding site. Such NF-κB-targeted decoy phosphorothioate oligonucleotides did not significantly affect cell survival in B-CLL and AML, yet enhanced the apoptotic response to classical cytotoxic compounds.60, 85, 86, 97 However, NF-κB decoy oligonucleotides are relatively large and polar compounds, a fact that negatively affects their cellular uptake and bioavailability.6 Thus, further drug design will be required to improve their clinical applicability.
Thalidomide and its analogs, including CC-5013 (Lenalidomide), are highly active against MM in clinical trials.98 Among several possible modes of action accounting for their therapeutic efficacy is inhibition of NF-κB activation.99 Indeed, thalidomide prevents IκBα degradation by inhibiting IKKβ6 (Figure 3). Thalidomide-induced apoptosis in MM cells is associated with downregulation of NF-κB DNA-binding activity and down-modulation of NF-κB targets such as c-IAP2 and c-FLIP.100
Malignant cells exhibiting constitutive NF-κB activation are relatively resistant to chemo- or radiotherapy, and NF-κB inhibitors increase their sensitivity to such anticancer treatments,3, 101 presumably by downmodulating antiapoptotic NF-κB target genes such as c-IAPs, c-FLIP, Bcl-2, and Bcl-XL.5 In B-precursor acute lymphoblastic leukemia (ALL), the most common pediatric malignancy, NF-κB is activated by treatment with anthracyclines, known to favor the nuclear translocation of NF-κB subunits,102 or by irradiation.103 Pharmacologic inhibition of NF-κB restored or enhanced apoptosis in doxorubicin-treated primary ALL cells.104 Moreover, the activation of physiological signal transduction pathways that inhibit constitutive activation of NF-κB may represent a strategy to overcome anthracycline resistance.101 Human growth hormone (GH) can sensitize the AML cell line U937 to TNF or anthracyclin-induced apoptosis via inhibition of NF-κB.105 Similarly, erythropoietin106 can sensitize U937 cells to daunorubicin-induced apoptosis. This effect involves an EPO-induced activation of JAK2 and stabilization of IκB.101 Thus, in this particular setting, JAK2 may exert a paradoxical, proapoptotic function. These results suggest that growth factors like EPO could be used to overcome NF-κB-mediated chemoresistance.
The flourishing literature on NF-κB in hematological malignancies suggests that this area of translational research may be particularly fertile in thus far that therapeutic strategies for subverting NF-κB function are being developed and enter clinical trials. Without doubt, indirect or direct NF-κB inhibitors will constitute a welcome addition to the hematological oncologist's repertoire.
Abbreviations
- ALL:
-
acute lymphocyte leukemia
- AML:
-
acute myeloid leukemia
- ATL:
-
adult T-cell leukemia
- Bcl-2:
-
B-cell leukemia/lymphoma 2
- BL:
-
Burkitt's lymphoma
- BMMNC:
-
bone marrow mononuclear cells
- CLL:
-
chronic lymphocytic leukemia
- CML:
-
chronic myelogenous leukemia
- DBCLs:
-
diffuse large B-cell lymphomas
- DISC:
-
death-inducing signaling complex
- EBNA:
-
EBV nuclear antigen
- EBV:
-
Epstein–Barr virus
- FADD:
-
Fas-associated death domain protein
- FISH:
-
fluorescence in situ hybridization
- FKBP51:
-
FK506-binding protein 51
- FLIP:
-
FLICE inhibitory protein
- HL:
-
Hodgkin's lymphoma
- HRS:
-
Hodgkin and Reed–Sternberg
- hTERT:
-
human telomerase reverse transcriptase
- HTLV-1:
-
human T-cell leukemia virus type I
- IAP:
-
inhibitor of apoptosis protein
- IκB:
-
inhibitor of NF-κB
- IKK:
-
IκB kinase
- IMF:
-
idiopathic myelofibrosis
- JAK:
-
janus kinase
- LMP:
-
latent membrane protein
- LSC:
-
leukemic stem cells
- LT:
-
lymphotoxin
- MALT:
-
mucosa-associated lymphoid tissue
- MDR:
-
multi-drug resistance
- MDS:
-
myelodysplastic syndrome
- MM:
-
multiple myeloma
- MPD:
-
myeloproliferative disorders
- NEMO:
-
NF-κB essential modulator
- NF-κB:
-
nuclear factor kappa B
- NIK:
-
NF-κB-inducing kinase
- PI3K:
-
phosphatidylinositol-3 kinase
- RANK:
-
receptor activator of NF-κB
- STAT:
-
signal transducer and activator of transcription
- TGF-β1:
-
transforming growth factor-β1
- TNF:
-
tumor necrosis factor
- TRADD:
-
TNF receptor-associated protein with a death domain
- VEGF:
-
vascular endothelial growth factor
- XIAP:
-
X-chromosome-linked inhibitor of apoptosis protein
References
Ghosh S and Karin M (2002) Missing pieces in the NF-kappaB puzzle. Cell 109 (Suppl): S81–S96.
Bentires-Alj M, Barbu V, Fillet M, Chariot A, Relic B, Jacobs N, Gielen J, Merville MP and Bours V (2003) NF-kappaB transcription factor induces drug resistance through MDR1 expression in cancer cells. Oncogene 22: 90–97.
Aggarwal BB (2004) Nuclear factor-kappaB: the enemy within. Cancer Cell 6: 203–208.
Hayden MS and Ghosh S (2004) Signaling to NF-kappaB. Genes Dev. 18: 2195–2224.
Karin M, Cao Y, Greten FR and Li ZW (2002) NF-kappaB in cancer: from innocent bystander to major culprit. Nat. Rev. Cancer 2: 301–310.
Karin M, Yamamoto Y and Wang QM (2004) The IKK NF-kappa B system: a treasure trove for drug development. Nat. Rev. Drug. Discov. 3: 17–26.
Gilmore TD (1999) Multiple mutations contribute to the oncogenicity of the retroviral oncoprotein v-Rel. Oncogene 18: 6925–6937.
Gilmore TD, Kalaitzidis D, Liang MC and Starczynowski DT (2004) The c-Rel transcription factor and B-cell proliferation: a deal with the devil. Oncogene 23: 2275–2286.
Gilmore TD, Cormier C, Jean-Jacques J and Gapuzan ME (2001) Malignant transformation of primary chicken spleen cells by human transcription factor c-Rel. Oncogene 20: 7098–7103.
Braun T, Carvalho G, Coquelle A, Vozenin MC, Lepelley P, Hirsch F, Kiladjian JJ, Ribrag V, Fenaux P and Kroemer G (2006) NF-{kappa}B constitutes a potential therapeutic target in high-risk myelodysplastic syndrom. Blood 107: 1156–1165.
Thomas RK, Re D, Wolf J and Diehl V (2004) Part I: Hodgkin's lymphoma – molecular biology of Hodgkin and Reed–Sternberg cells. Lancet. Oncol. 5: 11–18.
Bargou RC, Leng C, Krappmann D, Emmerich F, Mapara MY, Bommert K, Royer HD, Scheidereit C and Dorken B (1996) High-level nuclear NF-kappa B and Oct-2 is a common feature of cultured Hodgkin/Reed–Sternberg cells. Blood 87: 4340–4347.
Bargou RC, Emmerich F, Krappmann D, Bommert K, Mapara MY, Arnold W, Royer HD, Grinstein E, Greiner A, Scheidereit C and Dorken B (1997) Constitutive nuclear factor-kappaB-RelA activation is required for proliferation and survival of Hodgkin's disease tumor cells. J. Clin. Invest. 100: 2961–2969.
Mathas S, Johrens K, Joos S, Lietz A, Hummel F, Janz M, Jundt F, Anagnostopoulos I, Bommert K, Lichter P, Stein H, Scheidereit C and Dorken B (2005) Elevated NF-{kappa}B p50 complex formation and Bcl-3 expression in classical Hodgkin, anaplastic large cell, and other peripheral T. Blood 106: 4287–4293.
Niedobitek G, Deacon EM, Young LS, Herbst H, Hamilton-Dutoit SJ and Pallesen G (1991) Epstein–Barr virus gene expression in Hodgkin's disease. Blood 78: 1628–1630.
Gires O, Zimber-Strobl U, Gonnella R, Ueffing M, Marschall G, Zeidler R, Pich D and Hammerschmidt W (1997) Latent membrane protein 1 of Epstein–Barr virus mimics a constitutively active receptor molecule. EMBO J. 16: 6131–6140.
Emmerich F, Meiser M, Hummel M, Demel G, Foss HD, Jundt F, Mathas S, Krappmann D, Scheidereit C, Stein H and Dorken B (1999) Overexpression of I kappa B alpha without inhibition of NF-kappaB activity and mutations in the I kappa B alpha gene in Reed–Sternberg cells. Blood 94: 3129–3134.
Jungnickel B, Staratschek-Jox A, Brauninger A, Spieker T, Wolf J, Diehl V, Hansmann ML, Rajewsky K and Kuppers R (2000) Clonal deleterious mutations in the IkappaBalpha gene in the malignant cells in Hodgkin's lymphoma. J. Exp. Med. 191: 395–402.
Joos S, Menz CK, Wrobel G, Siebert R, Gesk S, Ohl S, Mechtersheimer G, Trumper L, Moller P, Lichter P and Barth TF (2002) Classical Hodgkin lymphoma is characterized by recurrent copy number gains of the short arm of chromosome 2. Blood 99: 1381–1387.
Mathas S, Lietz A, Anagnostopoulos I, Hummel F, Wiesner B, Janz M, Jundt F, Hirsch B, Johrens-Leder K, Vornlocher HP, Bommert K, Stein H and Dorken B (2004) c-FLIP mediates resistance of Hodgkin/Reed–Sternberg cells to death receptor-induced apoptosis. J. Exp. Med. 199: 1041–1052.
Houldsworth J, Mathew S, Rao PH, Dyomina K, Louie DC, Parsa N, Offit K and Chaganti RS (1996) REL proto-oncogene is frequently amplified in extranodal diffuse large cell lymphoma. Blood 87: 25–29.
Trecca D, Guerrini L, Fracchiolla NS, Pomati M, Baldini L, Maiolo AT and Neri A (1997) Identification of a tumor-associated mutant form of the NF-kappaB RelA gene with reduced DNA-binding and transactivating activities. Oncogene 14: 791–799.
Neri A, Fracchiolla NS, Roscetti E, Garatti S, Trecca D, Boletini A, Perletti L, Baldini L, Maiolo AT and Berti E (1995) Molecular analysis of cutaneous B- and T-cell lymphomas. Blood 86: 3160–3172.
Zucca E, Roggero E and Pileri S (1998) B-cell lymphoma of MALT type: a review with special emphasis on diagnostic and management problems of low-grade gastric tumours. Br. J. Haematol. 100: 3–14.
Isaacson PG and Du MQ (2004) MALT lymphoma: from morphology to molecules. Nat. Rev. Cancer 4: 644–653.
Zhou H, Du MQ and Dixit VM (2005) Constitutive NF-kappaB activation by the t(11;18)(q21;q21) product in MALT lymphoma is linked to deregulated ubiquitin ligase activity. Cancer Cell. 7: 425–431.
Ye H, Liu H, Attygalle A, Wotherspoon AC, Nicholson AG, Charlotte F, Leblond V, Speight P, Goodlad J, Lavergne-Slove A, Martin-Subero JI, Siebert R, Dogan A, Isaacson PG and Du MQ (2003) Variable frequencies of t(11;18)(q21;q21) in MALT lymphomas of different sites: significant association with CagA strains of H pylori in gastric MALT lymphoma. Blood 102: 1012–1018.
Akagi T, Motegi M, Tamura A, Suzuki R, Hosokawa Y, Suzuki H, Ota H, Nakamura S, Morishima Y, Taniwaki M and Seto M (1999) A novel gene, MALT1 at 18q21, is involved in t(11;18) (q21;q21) found in low-grade B-cell lymphoma of mucosa-associated lymphoid tissue. Oncogene 18: 5785–5794.
Zhou H, Wertz I, O'Rourke K, Ultsch M, Seshagiri S, Eby M, Xiao W and Dixit VM (2004) Bcl10 activates the NF-kappaB pathway through ubiquitination of NEMO. Nature 427: 167–171.
Cerimele F, Battle T, Lynch R, Frank DA, Murad E, Cohen C, Macaron N, Sixbey J, Smith K, Watnick RS, Eliopoulos A, Shehata B and Arbiser JL (2005) Reactive oxygen signaling and MAPK activation distinguish Epstein–Barr Virus (EBV)-positive versus EBV-negative Burkitt's lymphoma. Proc. Natl. Acad. Sci. USA 102: 175–179.
Haralambieva E, Banham AH, Bastard C, Delsol G, Gaulard P, Ott G, Pileri S, Fletcher JA and Mason DY (2003) Detection by the fluorescence in situ hybridization technique of MYC translocations in paraffin-embedded lymphoma biopsy samples. Br. J. Haematol. 121: 49–56.
Kuppers R, Klein U, Hansmann ML and Rajewsky K (1999) Cellular origin of human B-cell lymphomas. N. Engl. J. Med. 341: 1520–1529.
Savage KJ, Monti S, Kutok JL, Cattoretti G, Neuberg D, De Leval L, Kurtin P, Dal Cin P, Ladd C, Feuerhake F, Aguiar RC, Li S, Salles G, Berger F, Jing W, Pinkus GS, Habermann T, Dalla-Favera R, Harris NL, Aster JC, Golub TR and Shipp MA (2003) The molecular signature of mediastinal large B-cell lymphoma differs from that of other diffuse large B-cell lymphomas and shares features with classical Hodgkin lymphoma. Blood. 102: 3871–3879.
Rosenwald A, Wright G, Chan WC, Connors JM, Campo E, Fisher RI, Gascoyne RD, Muller-Hermelink HK, Smeland EB, Giltnane JM, Hurt EM, Zhao H, Averett L, Yang L, Wilson WH, Jaffe ES, Simon R, Klausner RD, Powell J, Duffey PL, Longo DL, Greiner TC, Weisenburger DD, Sanger WG, Dave BJ, Lynch JC, Vose J, Armitage JO, Montserrat E, Lopez-Guillermo A, Grogan TM, Miller TP, LeBlanc M, Ott G, Kvaloy S, Delabie J, Holte H, Krajci P, Stokke T and Staudt LM (2002) The use of molecular profiling to predict survival after chemotherapy for diffuse large-B-cell lymphoma. N. Engl. J. Med. 346: 1937–1947.
Davis RE, Brown KD, Siebenlist U and Staudt LM (2001) Constitutive nuclear factor kappaB activity is required for survival of activated B cell-like diffuse large B cell lymphoma cells. J. Exp. Med. 194: 1861–1874.
Feuerhake F, Kutok JL, Monti S, Chen W, LaCasce AS, Cattoretti G, Kurtin P, Pinkus GS, de Leval L, Harris NL, Savage KJ, Neuberg D, Habermann TM, Dalla-Favera R, Golub TR, Aster JC and Shipp MA (2005) NFkappaB activity, function, and target-gene signatures in primary mediastinal large B-cell lymphoma and diffuse large B-cell lymphoma subtypes. Blood 106: 1392–1399.
Monti S, Savage KJ, Kutok JL, Feuerhake F, Kurtin P, Mihm M, Wu B, Pasqualucci L, Neuberg D, Aguiar RC, Dal Cin P, Ladd C, Pinkus GS, Salles G, Harris NL, Dalla-Favera R, Habermann TM, Aster JC, Golub TR and Shipp MA (2005) Molecular profiling of diffuse large B-cell lymphoma identifies robust subtypes including one characterized by host inflammatory response. Blood 105: 1851–1861.
Tracey L, Perez-Rosado A, Artiga MJ, Camacho FI, Rodriguez A, Martinez N, Ruiz-Ballesteros E, Mollejo M, Martinez B, Cuadros M, Garcia JF, Lawler M and Piris MA (2005) Expression of the NF-kappaB targets BCL2 and BIRC5/Survivin characterizes small B-cell and aggressive B-cell lymphomas, respectively. J. Pathol. 206: 123–134.
Hallek M, Bergsagel PL and Anderson KC (1998) Multiple myeloma: increasing evidence for a multistep transformation process. Blood 91: 3–21.
Ni H, Ergin M, Huang Q, Qin JZ, Amin HM, Martinez RL, Saeed S, Barton K and Alkan S (2001) Analysis of expression of nuclear factor kappa B (NF-kappa B) in multiple myeloma: downregulation of NF-kappa B induces apoptosis. Br. J. Haematol. 115: 279–286.
Bharti AC, Donato N and Aggarwal BB (2003) Curcumin (diferuloylmethane) inhibits constitutive and IL-6-inducible STAT3 phosphorylation in human multiple myeloma cells. J. Immunol. 171: 3863–3871.
Bharti AC, Shishodia S, Reuben JM, Weber D, Alexanian R, Raj-Vadhan S, Estrov Z, Talpaz M and Aggarwal BB (2004) Nuclear factor-kappaB and STAT3 are constitutively active in CD138+ cells derived from multiple myeloma patients, and suppression of these transcription factors leads to apoptosis. Blood 103: 3175–3184.
Tu Y, Renner S, Xu F, Fleishman A, Taylor J, Weisz J, Vescio R, Rettig M, Berenson J, Krajewski S, Reed JC and Lichtenstein A (1998) BCL-X expression in multiple myeloma: possible indicator of chemoresistance. Cancer. Res. 58: 256–262.
Escobar-Diaz E, Lopez-Martin EM, Hernandez del Cerro M, Puig-Kroger A, Soto-Cerrato V, Montaner B, Giralt E, Garcia-Marco JA, Perez-Tomas R and Garcia-Pardo A (2005) AT514, a cyclic depsipeptide from Serratia marcescens, induces apoptosis of B-chronic lymphocytic leukemia cells: interference with the Akt/NF-kappaB survival pathway. Leukemia 19: 572–579.
Furman RR, Asgary Z, Mascarenhas JO, Liou HC and Schattner EJ (2000) Modulation of NF-kappa B activity and apoptosis in chronic lymphocytic leukemia B cells. J. Immunol. 164: 2200–2206.
Cuni S, Perez-Aciego P, Perez-Chacon G, Vargas JA, Sanchez A, Martin-Saavedra FM, Ballester S, Garcia-Marco J, Jorda J and Durantez A (2004) A sustained activation of PI3K/NF-kappaB pathway is critical for the survival of chronic lymphocytic leukemia B cells. Leukemia 18: 1391–1400.
Farahani M, Treweeke AT, Toh CH, Till KJ, Harris RJ, Cawley JC, Zuzel M and Chen H (2005) Autocrine VEGF mediates the antiapoptotic effect of CD154 on CLL cells. Leukemia 19: 524–530.
Chen H, Treweeke AT, West DC, Till KJ, Cawley JC, Zuzel M and Toh CH (2000) In vitro and in vivo production of vascular endothelial growth factor by chronic lymphocytic leukemia cells. Blood 96: 3181–3187.
Granziero L, Ghia P, Circosta P, Gottardi D, Strola G, Geuna M, Montagna L, Piccoli P, Chilosi M and Caligaris-Cappio F (2001) Survivin is expressed on CD40 stimulation and interfaces proliferation and apoptosis in B-cell chronic lymphocytic leukemia. Blood 97: 2777–2783.
Delaval B, Lelievre H and Birnbaum D (2005) Myeloproliferative disorders: the centrosome connection. Leukemia 19: 1739–1744.
Reuther JY, Reuther GW, Cortez D, Pendergast AM and Baldwin Jr AS (1998) A requirement for NF-kappaB activation in Bcr-Abl-mediated transformation. Genes Dev. 12: 968–981.
Munzert G, Kirchner D, Ottmann O, Bergmann L and Schmid RM (2004) Constitutive NF-kappab/Rel activation in Philadelphia chromosome positive (Ph+) acute lymphoblastic leukemia (ALL). Leuk. Lymphoma 45: 1181–1184.
Yokota S, Nakao M, Horiike S, Seriu T, Iwai T, Kaneko H, Azuma H, Oka T, Takeda T, Watanabe A, Kikuta A, Asami K, Sekine I, Matsushita T, Tsuhciya T, Mimaya J, Koizumi S, Miyake M, Nishikawa K, Takaue Y, Kawano Y, Iwai A, Ishida Y, Matsumoto K and Fujimoto T (1998) Mutational analysis of the N-ras gene in acute lymphoblastic leukemia: a study of 125 Japanese pediatric cases. Int. J. Hematol. 67: 379–387.
Tomita M, Kawakami H, Uchihara JN, Okudaira T, Masuda M, Takasu N, Matsuda T, Ohta T, Tanaka Y and Mori N (2006) Curcumin suppresses constitutive activation of AP-1 by downregulation of JunD protein in HTLV-1-infected T-cell lines. Leuk. Res. 30: 313–321.
Tajima K (1990) The 4th nation-wide study of adult T-cell leukemia/lymphoma (ATL) in Japan: estimates of risk of ATL and its geographical and clinical features. The T- and B-cell Malignancy Study Group. Int. J. Cancer 45: 237–243.
Pozzatti R, Vogel J and Jay G (1990) The human T-lymphotropic virus type I tax gene can cooperate with the ras oncogene to induce neoplastic transformation of cells. Mol. Cell. Biol. 10: 413–417.
Sun SC and Ballard DW (1999) Persistent activation of NF-kappaB by the tax transforming protein of HTLV-1: hijacking cellular IkappaB kinases. Oncogene 18: 6948–6958.
Sinha-Datta U, Horikawa I, Michishita E, Datta A, Sigler-Nicot JC, Brown M, Kazanji M, Barrett JC and Nicot C (2004) Transcriptional activation of hTERT through the NF-kappaB pathway in HTLV-I-transformed cells. Blood 104: 2523–2531.
Geleziunas R, Ferrell S, Lin X, Mu Y, Cunningham Jr ET, Grant M, Connelly MA, Hambor JE, Marcu KB and Greene WC (1998) Human T-cell leukemia virus type 1 Tax induction of NF-kappaB involves activation of the IkappaB kinase alpha (IKKalpha) and IKKbeta cellular kinases. Mol. Cell. Biol. 18: 5157–5165.
Turco MC, Romano MF, Petrella A, Bisogni R, Tassone P and Venuta S (2004) NF-kappaB/Rel-mediated regulation of apoptosis in hematologic malignancies and normal hematopoietic progenitors. Leukemia 18: 11–17.
Mori N, Nunokawa Y, Yamada Y, Ikeda S, Tomonaga M and Yamamoto N (1999) Expression of human inducible nitric oxide synthase gene in T-cell lines infected with human T-cell leukemia virus type-I and primary adult T-cell leukemia cells. Blood 94: 2862–2870.
Kawakami H, Tomita M, Matsuda T, Ohta T, Tanaka Y, Fujii M, Hatano M, Tokuhisa T and Mori N (2005) Transcriptional activation of survivin through the NF-kappaB pathway by human T-cell leukemia virus type I tax. Int. J. Cancer 115: 967–974.
Bueso-Ramos CE, Rocha FC, Shishodia S, Medeiros LJ, Kantarjian HM, Vadhan-Raj S, Estrov Z, Smith TL, Nguyen MH and Aggarwal BB (2004) Expression of constitutively active nuclear-kappa B RelA transcription factor in blasts of acute myeloid leukemia. Hum. Pathol. 35: 246–253.
Sanz C, Richard C, Prosper F and Fernandez-Luna JL (2002) Nuclear factor k B is activated in myelodysplastic bone marrow cells. Haematologica 87: 1005–1006.
Kerbauy DM, Lesnikov V, Abbasi N, Seal S, Scott B and Deeg HJ (2005) NF-{kappa}B and FLIP in arsenic trioxide (ATO)-induced apoptosis in. Blood 106: 3917–3925.
Sawanobori M, Yamaguchi S, Hasegawa M, Inoue M, Suzuki K, Kamiyama R, Hirokawa K and Kitagawa M (2003) Expression of TNF receptors and related signaling molecules in the bone marrow from patients with myelodysplastic syndromes. Leuk. Res. 27: 583–591.
Benesch M, Platzbecker U, Ward J, Deeg HJ and Leisenring W (2003) Expression of FLIP(Long) and FLIP(Short) in bone marrow mononuclear and CD34+ cells in patients with myelodysplastic syndrome: correlation with apoptosis. Leukemia 17: 2460–2466.
Boudard D, Vasselon C, Bertheas MF, Jaubert J, Mounier C, Reynaud J, Viallet A, Chautard S, Guyotat D and Campos L (2002) Expression and prognostic significance of Bcl-2 family proteins in myelodysplastic syndromes. Am. J. Hematol. 70: 115–125.
Yamamoto K, Abe S, Nakagawa Y, Suzuki K, Hasegawa M, Inoue M, Kurata M, Hirokawa K and Kitagawa M (2004) Expression of IAP family proteins in myelodysplastic syndromes transforming to overt leukemia. Leuk. Res. 28: 1203–1211.
Estrov Z, Shishodia S, Faderl S, Harris D, Van Q, Kantarjian HM, Talpaz M and Aggarwal BB (2003) Resveratrol blocks interleukin-1beta-induced activation of the nuclear transcription factor NF-kappaB, inhibits proliferation, causes S-phase arrest, and induces apoptosis of acute myeloid leukemia cells. Blood 102: 987–995.
Guzman ML, Swiderski CF, Howard DS, Grimes BA, Rossi RM, Szilvassy SJ and Jordan CT (2002) Preferential induction of apoptosis for primary human leukemic stem cells. Proc. Natl. Acad. Sci. USA 99: 16220–16225.
Guzman ML, Neering SJ, Upchurch D, Grimes B, Howard DS, Rizzieri DA, Luger SM and Jordan CT (2001) Nuclear factor-kappaB is constitutively activated in primitive human acute myelogenous leukemia cells. Blood 98: 2301–2307.
Frelin C, Imbert V, Griessinger E, Peyron AC, Rochet N, Philip P, Dageville C, Sirvent A, Hummelsberger M, Berard E, Dreano M, Sirvent N and Peyron JF (2005) Targeting NF-kappaB activation via pharmacologic inhibition of IKK2-induced apoptosis of human acute myeloid leukemia cells. Blood 105: 804–811.
Baumgartner B, Weber M, Quirling M, Fischer C, Page S, Adam M, Von Schilling C, Waterhouse C, Schmid C, Neumeier D and Brand K (2002) Increased IkappaB kinase activity is associated with activated NF-kappaB in acute myeloid blasts. Leukemia 16: 2062–2071.
Estrov Z, Manna SK, Harris D, Van Q, Estey EH, Kantarjian HM, Talpaz M and Aggarwal BB (1999) Phenylarsine oxide blocks interleukin-1beta-induced activation of the nuclear transcription factor NF-kappaB, inhibits proliferation, and induces apoptosis of acute myelogenous leukemia cells. Blood 94: 2844–2853.
Kirchner D, Duyster J, Ottmann O, Schmid RM, Bergmann L and Munzert G (2003) Mechanisms of Bcr-Abl-mediated NF-kappaB/Rel activation. Exp. Hematol. 31: 504–511.
LeMaistre A, Lee MS, Talpaz M, Kantarjian HM, Freireich EJ, Deisseroth AB, Trujillo JM and Stass SA (1989) Ras oncogene mutations are rare late stage events in chronic myelogenous leukemia. Blood 73: 889–891.
Finco TS, Westwick JK, Norris JL, Beg AA, Der CJ and Baldwin Jr AS (1997) Oncogenic Ha-Ras-induced signaling activates NF-kappaB transcriptional activity, which is required for cellular transformation. J. Biol. Chem. 272: 24113–24116.
Komura E, Tonetti C, Penard-Lacronique V, Chagraoui H, Lacout C, Lecouedic JP, Rameau P, Debili N, Vainchenker W and Giraudier S (2005) Role for the nuclear factor kappaB pathway in transforming growth factor-beta1 production in idiopathic myelofibrosis: possible relationship with FK506 binding protein 51 overexpression. Cancer Res. 65: 3281–3289.
Rameshwar P, Narayanan R, Qian J, Denny TN, Colon C and Gascon P (2000) NF-kappa B as a central mediator in the induction of TGF-beta in monocytes from patients with idiopathic myelofibrosis: an inflammatory response beyond the realm of homeostasis. J. Immunol. 165: 2271–2277.
James C, Ugo V, Le Couedic JP, Staerk J, Delhommeau F, Lacout C, Garcon L, Raslova H, Berger R, Bennaceur-Griscelli A, Villeval JL, Constantinescu SN, Casadevall N and Vainchenker W (2005) A unique clonal JAK2 mutation leading to constitutive signalling causes polycythaemia vera. Nature 434: 1144–1148.
Digicaylioglu M and Lipton SA (2001) Erythropoietin-mediated neuroprotection involves cross-talk between Jak2 and NF-kappaB signalling cascades. Nature 412: 641–647.
Hideshima T, Richardson P and Anderson KC (2003) Novel therapeutic approaches for multiple myeloma. Immunol. Rev. 194: 164–176.
Hideshima T, Richardson P, Chauhan D, Palombella VJ, Elliott PJ, Adams J and Anderson KC (2001) The proteasome inhibitor PS-341 inhibits growth, induces apoptosis, and overcomes drug resistance in human multiple myeloma cells. Cancer Res. 61: 3071–3076.
Romano MF, Petrella A, Bisogni R, Turco MC and Venuta S (2003) Effect of NF-kappaB/Rel inhibition on spontaneous vs chemotherapy-induced apoptosis in AML and normal cord blood CD34+ cells. Leukemia 17: 1190–1192.
Romano MF, Lamberti A, Bisogni R, Tassone P, Pagnini D, Storti G, Del Vecchio L, Turco MC and Venuta S (2000) Enhancement of cytosine arabinoside-induced apoptosis in human myeloblastic leukemia cells by NF-kappa B/Rel- specific decoy oligodeoxynucleotides. Gene. Therapy 7: 1234–1237.
Zhou A, Scoggin S, Gaynor RB and Williams NS (2003) Identification of NF-kappa B-regulated genes induced by TNFalpha utilizing expression profiling and RNA interference. Oncogene 22: 2054–2064.
Coux O, Tanaka K and Goldberg AL (1996) Structure and functions of the 20S and 26S proteasomes. Annu. Rev. Biochem. 65: 801–847.
Dong QG, Sclabas GM, Fujioka S, Schmidt C, Peng B, Wu T, Tsao MS, Evans DB, Abbruzzese JL, McDonnell TJ and Chiao PJ (2002) The function of multiple IkappaB: NF-kappaB complexes in the resistance of cancer cells to Taxol-induced apoptosis. Oncogene 21: 6510–6519.
Richardson PG, Barlogie B, Berenson J, Singhal S, Jagannath S, Irwin D, Rajkumar SV, Srkalovic G, Alsina M, Alexanian R, Siegel D, Orlowski RZ, Kuter D, Limentani SA, Lee S, Hideshima T, Esseltine DL, Kauffman M, Adams J, Schenkein DP and Anderson KC (2003) A phase 2 study of bortezomib in relapsed, refractory myeloma. N. Engl. J. Med. 348: 2609–2617.
Richardson PG, Sonneveld P, Schuster MW, Irwin D, Stadtmauer EA, Facon T, Harousseau JL, Ben-Yehuda D, Lonial S, Goldschmidt H, Reece D, San-Miguel JF, Blade J, Boccadoro M, Cavenagh J, Dalton WS, Boral AL, Esseltine DL, Porter JB, Schenkein D and Anderson KC (2005) Bortezomib or high-dose dexamethasone for relapsed multiple myeloma. N. Engl. J. Med. 352: 2487–2498.
Goy A, Younes A, McLaughlin P, Pro B, Romaguera JE, Hagemeister F, Fayad L, Dang NH, Samaniego F, Wang M, Broglio K, Samuels B, Gilles F, Sarris AH, Hart S, Trehu E, Schenkein D, Cabanillas F and Rodriguez AM (2005) Phase II study of proteasome inhibitor bortezomib in relapsed or refractory B-cell non-Hodgkin's lymphoma. J. Clin. Oncol. 23: 667–675.
Perez-Galan P, Roue G, Villamor N, Montserrat E, Campo E and Colomer D (2006) The proteasome inhibitor bortezomib induces apoptosis in mantle cell lymphoma through generation of ROS species and Noxa activation independent of p53 status. Blood 107: 257–264.
Orlowski RZ, Voorhees PM, Garcia RA, Hall MD, Kudrik FJ, Allred T, Johri AR, Jones PE, Ivanova A, Van Deventer HW, Gabriel DA, Shea TC, Mitchell BS, Adams J, Esseltine DL, Trehu EG, Green M, Lehman MJ, Natoli S, Collins JM, Lindley CM and Dees EC (2005) Phase 1 trial of the proteasome inhibitor bortezomib and pegylated liposomal doxorubicin in patients with advanced hematologic malignancies. Blood 105: 3058–3065.
Paramore A and Frantz S (2003) Bortezomib. Nat. Rev. Drug Discov. 2: 611–612.
Rajkumar SV, Richardson PG, Hideshima T and Anderson KC (2005) Proteasome inhibition as a novel therapeutic target in human cancer. J. Clin. Oncol. 23: 630–639.
Romano MF, Lamberti A, Tassone P, Alfinito F, Costantini S, Chiurazzi F, Defrance T, Bonelli P, Tuccillo F, Turco MC and Venuta S (1998) Triggering of CD40 antigen inhibits fludarabine-induced apoptosis in B chronic lymphocytic leukemia cells. Blood 92: 990–995.
Teo SK (2005) Properties of thalidomide and its analogues: implications for anticancer therapy. AAPS J. 7: E14–E19.
Keifer JA, Guttridge DC, Ashburner BP and Baldwin Jr AS (2001) Inhibition of NF-kappa B activity by thalidomide through suppression of IkappaB kinase activity. J. Biol. Chem. 276: 22382–22387.
Mitsiades N, Mitsiades CS, Poulaki V, Chauhan D, Richardson PG, Hideshima T, Munshi NC, Treon SP and Anderson KC (2002) Apoptotic signaling induced by immunomodulatory thalidomide analogs in human multiple myeloma cells: therapeutic implications. Blood 99: 4525–4530.
Carvalho G, Lefaucheur C, Cherbonnier C, Metivier D, Chapel A, Pallardy M, Bourgeade MF, Charpentier B, Hirsch F and Kroemer G (2005) Chemosensitization by erythropoietin through inhibition of the NF-kappaB rescue pathway. Oncogene 24: 737–745.
Laurent G and Jaffrezou JP (2001) Signaling pathways activated by daunorubicin. Blood 98: 913–924.
Weston VJ, Austen B, Wei W, Marston E, Alvi A, Lawson S, Darbyshire PJ, Griffiths M, Hill F, Mann JR, Moss PA, Taylor AM and Stankovic T (2004) Apoptotic resistance to ionizing radiation in pediatric B-precursor acute lymphoblastic leukemia frequently involves increased NF-kappaB survival pathway signaling. Blood 104: 1465–1473.
Avellino R, Romano S, Parasole R, Bisogni R, Lamberti A, Poggi V, Venuta S and Romano MF (2005) Rapamycin stimulates apoptosis of childhood acute lymphoblastic leukemia cells. Blood 106: 1400–1406.
Cherbonnier C, Deas O, Carvalho G, Vassal G, Durrbach A, Haeffner A, Charpentier B, Benard J and Hirsch F (2003) Potentiation of tumour apoptosis by human growth hormone via glutathione production and decreased NF-kappaB activity. Br. J. Cancer 89: 1108–1115.
Wattel E, Solary E, Hecquet B, Caillot D, Ifrah N, Brion A, Milpied N, Janvier M, Guerci A, Rochant H, Cordonnier C, Dreyfus F, Veil A, Hoang-Ngoc L, Stoppa AM, Gratecos N, Sadoun A, Tilly H, Brice P, Lioure B, Desablens B, Pignon B, Abgrall JP, Leporrier M and Fenaux P (1999) Quinine improves results of intensive chemotherapy (IC) in myelodysplastic syndromes (MDS) expressing P-glycoprotein (PGP). Updated results of a randomized study. Groupe Francais des Myelodysplasies (GFM) and Groupe GOELAMS. Adv. Exp. Med. Biol. 457: 35–46.
Horita M, Andreu EJ, Benito A, Arbona C, Sanz C, Benet I, Prosper F and Fernandez-Luna JL (2000) Blockade of the Bcr-Abl kinase activity induces apoptosis of chronic myelogenous leukemia cells by suppressing signal transducer and activator of transcription 5-dependent expression of Bcl-xL. J. Exp. Med. 191: 977–984.
Acknowledgements
Guido Kroemer is supported by Cancéropôle Ile-de-France, Association pour le Recherche sur le cancer, Fondation de France, and European Community (Active p53, TransDeath, Right). Thorsten Braun is supported by a fellowship from the Etablissement Français du Sang. Gabrielle Carvalho is supported by the Association NRB Vaincre le Cancer. Claire Fabre is supported by the Fondation Recherche Médicale. Jennifer Grosjean is supported by Cancéropôle Ile-de-France.
Author information
Authors and Affiliations
Corresponding author
Additional information
Edited by G Melino
Rights and permissions
About this article
Cite this article
Braun, T., Carvalho, G., Fabre, C. et al. Targeting NF-κB in hematologic malignancies. Cell Death Differ 13, 748–758 (2006). https://doi.org/10.1038/sj.cdd.4401874
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.cdd.4401874
Keywords
This article is cited by
-
PHF6 maintains acute myeloid leukemia via regulating NF-κB signaling pathway
Leukemia (2023)
-
The molecular biology and therapeutic potential of Nrf2 in leukemia
Cancer Cell International (2022)
-
Hinokiflavone induces apoptosis, cell cycle arrest and autophagy in chronic myeloid leukemia cells through MAPK/NF-κB signaling pathway
BMC Complementary Medicine and Therapies (2022)
-
The Ube2m-Rbx1 neddylation-Cullin-RING-Ligase proteins are essential for the maintenance of Regulatory T cell fitness
Nature Communications (2022)
-
NT157 has antineoplastic effects and inhibits IRS1/2 and STAT3/5 in JAK2V617F-positive myeloproliferative neoplasm cells
Signal Transduction and Targeted Therapy (2020)