Abstract
We have recently shown that a human CD4+ T cell line (CEM-SS) acquires the permissiveness to M-tropic strains and primary isolates of HIV-1 after transplantation into SCID mice. This permissiveness was associated with the acquisition of a memory (CD45RO+) phenotype as well as of a functional CCR5 coreceptor. In this study, we have used this model for invest-igating in vivo the relationships between HIV-1 infection, apoptosis and T cell differentiation. When an in vivo HIV-1 infection was performed, the CEM cell tumors grew to a lower extent than the uninfected controls. CEM cells explanted from uninfected SCID mice (ex vivo CEM) underwent a significant level of spontaneous apoptosis and proved to be CD45RO+, Fas+ and Fas-L+, while Bcl-2 expression was significantly reduced as compared to the parental cells. Acute HIV-1 infection markedly increased apoptosis of uninfected ex vivo CEM cells, through a Fas/Fas-L-mediated autocrine suicide/fratricide, while parental cells did not undergo apoptosis following viral infection. The susceptibility to apoptosis of ex vivo CEM cells infected with the NSI strain of HIV-1, was progressively lost during culture, in parallel with the loss of Fas-L and marked changes in the Bcl-2 cellular distribution. On the whole, these results are strongly reminiscent of a series of events possibly occurring during HIV-1 infection. After an initial depletion of bystander CD4+ memory T cells during acute infection, latently or chronically infected CD4+ T lymphocytes are progressively selected and are protected against spontaneous apoptosis through the development of an efficient survival program. Studies with human cells passaged into SCID mice may offer new opportunities for an in vivo investigation of the mechanisms involved in HIV-1 infection and CD4+ T cell depletion.
Similar content being viewed by others
Introduction
The central problem of HIV-1 pathogenesis is the decline of CD4+ T lymphocytes, which precedes the progression from asymptomatic infection to the acquired immunodeficiency syndrome (AIDS). Mechanisms underlying CD4+ T cell depletion in AIDS patients still remain poorly understood.1,2 Progress in this area has been hampered by the problems in reconciling the results obtained in studies using in vitro cell systems with the events occurring under in vivo conditions and, possibly, with those observed in HIV-1 infected patients. For instance, some isolates of HIV-1 recovered from patients with CD4+ T cell depletion show no cytopathic effect on cultured human T cells, suggesting that HIV-1 infection may lead to dysfunction and eventual loss of CD4+ T cells by indirect mechanisms that do not require virus infection of the target cells.3 Recent data highly support the hypothesis that one of the major causes of CD4+ T cell depletion, both in the peripheral blood and in the lymph nodes of AIDS patients, is the virus-mediated induction of apoptosis of bystander CD4+ T cells.4,5,6,7 Of interest, various reports have shown that CD4+ memory T cells (CD45RO+) may represent the major target for both HIV-1 infection and HIV-1-induced apoptosis.8,9,10,11 However, mechanisms responsible for these phenomena are still unknown.
Human-severe combined immunodeficient (SCID) mouse xenografts represent unique and practical in vivo models to study the early events triggered by the interaction of HIV-1 with the human immune system.12,13,14,15,16,17,18 In particular, the interactions between human lymphoid cells and the SCID mouse environment occurring in these models can lead to a marked activation/differentiation of the immune cells.19,20,21 Recently, we have observed that human lymphoblastoid CD4+ T cells (CEM cells), which are exclusively permissive in vitro to syncytium-inducing (SI) T-tropic HIV-1 strains, became permissive to M-tropic strain of HIV-1 after passage into SCID mice. This in vivo acquired permissiveness was due to an increase in the expression of a functional CCR5 β-chemokine receptor and was strongly associated with the appearance of a memory phenotype (CD45RO) on CEM cells.22 In the present study, we first investigated in vivo the effects of various HIV-1 strains on the growth of CEM cells in SCID mice. Moreover, we characterized the apoptotic phenotype of CEM cells obtained from SCID mice tumors (ex vivo CEM cells) and the effects of HIV-1 infection. We found that transplantation of CEM cells in SCID mice induced apoptotic behavior in these cells and that this newly acquired property was strongly associated with the expression of the CD45RO+ phenotype. HIV-1 infection markedly increased the apoptosis of bystander CEM cells through a massive Fas-mediated autocrine suicide/fratricide. After this early phase, T-tropic strains of HIV-1 induced cytopathic effect, while M-tropic strains led to a low level of chronic infection in CEM cells, which gained resistance to spontaneous apoptosis through the development of an efficient survival program. On the whole, these data, obtained in a human-SCID mouse model, recapitulate a sequence of events that may occur in the natural history of AIDS, such as CD4+ T cell depletion and the development of latently infected cells.23,24 Thus, studies with human cells passaged in SCID mice may offer new opportunities for in vivo investigating the mechanisms underlying HIV-1 infection and CD4+ T cell depletion.
Results
Impairment of CEM cells tumor growth and enhanced apoptosis of CEM cells by in vivo acute HIV-1 infection in SCID mice
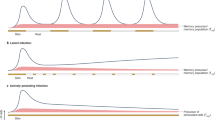
We performed an acute infection with the SF162 or the IIIB HIV-1 strains contemporaneously to the CEM cells subcutaneous (s.c.) injection in SCID mice. Consistently with a recent finding,22 CEM-SCID mouse xenografts were highly infected with both the HIV-1 strains used, while the parental CEM cells were in vitro infectable exclusively with the T-tropic strain of HIV (data not shown). This was due to a significant upregulation of a functional CCR5 on CEM cells that was crucial in rendering these cells permissive to the M-tropic strain of HIV-1, SF162.22 As shown in Figure 1A, infection with both HIV-1 strains resulted in a marked delay in the growth of CEM cell s.c. tumors in SCID mice, as compared to the uninfected tumors. To assess the nature of this virus-induced in vivo delay of CEM cell tumor growth, we compared the levels of spontaneous apoptosis, by flow cytometric analysis of TUNEL reaction, in single cell preparations of CEM cells collected from HIV-1 infected and uninfected s.c. tumors (ex vivo CEM cells), when the tumors reached 1 cm in diameter. The results showed that uninfected ex vivo CEM cells exhibited remarkable levels of spontaneous apoptosis (30–40%). However, higher levels of apoptosis (60–75%) were observed in ex vivo CEM cells from HIV-1-infected tumors (Figure 1B). Notably, histological analysis showed that both infected and uninfected CEM tumors were highly vascolarized and poorly necrotic (data not shown).
Effects of in vivo HIV-1 infection on CEM cells growth and apoptosis in SCID mice. (A) CEM cell tumor growth in uninfected xenografts (□) and xenografts infected with the SF162 (▪) or IIIB (▴) HIV-1 strains; (B) Percentages of apoptotic cells in CEM cells isolated from the s.c. CEM tumors (ex vivo) uninfected ([open box]) and infected with SF162 ([filled box]) or IIIB ([hatched box]) HIV-1 strains. Points of the curves and histograms are means±S.E.M. of 15 animals in five separate experiments
CEM cells obtained from SCID mice exhibit an apoptotic phenotype
This data prompted us to characterize the phenotype of uninfected and HIV-1-infected ex vivo CEM cells, as compared to the parental cell line. We firstly analyzed the expression of CD45RO, CD45RA, Fas, Fas-L, Bcl-2, Bcl-xL and Bax, in uninfected ex vivo and parental CEM cells. Ex vivo and parental CEM cells did not show major differences in terms of T phenotypic markers, in that both cell types were CD4+, weakly CD3+, CD8− and CD14− (data not shown). Consistently with a previous report,22 FACS analysis showed that ex vivo CEM had become CD45RO+, while parental CEM cells were CD45RO− (data not shown). FACS analysis showed a significant induction of Fas-L expression and marked decrease of Bcl-2 in ex vivo CEM cells, as compared to the parental cells (Figure 2A). The bcl2 protein level was also investigated by Western blot analysis. Consistently with the results of the flow cytometric analysis, the experiments showed significant reduction of bcl2 protein in ex vivo CEM cells as compared to the parental cells (Figure 2B). Densitometric analysis showed that there was a twofold increase of the bcl2 content in parental CEM cells with respect to ex vivo CEM cells. Consistently with the protein expression, RT–PCR analysis showed lower level of bcl2 and higher level of FasL transcripts in ex vivo CEM cells, while no differences in the expression of Bax and Bcl-xL were observed (Figure 2C). Taken together, these data indicated that the phenotype of ex vivo CEM cells markedly differed from that of parental cells. This could be the result of either a progressive differentiation of CEM cells due to the stimuli present in the mouse environment or an expansion of a very small fraction of CEM cells (expressing the CD45RO phenotype, high level of Fas-L and low level of Bcl-2) in SCID mice. This hypothesis appears unlikely in the view of the fact that CD45RO and Fas-L are not expressed in parental CEM cells.
Phenotype analysis of CEM cells isolated from s.c. tumors grown in SCID mice (ex vivo) as compared to the parental CEM cells. (A) Fas-L and Bcl-2 expression in parental (dotted lines) and ex vivo (solid lines) CEM cells analyzed by flow cytometry; (B) Western blot analysis of bcl-2 protein level in parental and ex vivo CEM cells; (C) RT–PCR of parental and ex vivo CEM cells; (D) Flow cytometric analysis of Fas-L expression in uninfected (left panel) and HIV-infected (right panel) ex vivo CEM cells. All the results are representative of 15 animals in five separate experiments
In examining the phenotype of HIV-1 infected ex vivo CEM cells, we found that the percentage of Fas-L+ cells was markedly increased as compared to the uninfected cells (Figure 2D), while Fas, Bcl-2, Bcl-xL and Bax mRNA expression did not differ between infected and uninfected ex vivo CEM cells (data not shown).
Mechanisms underlying HIV-1-induced apoptosis of ex vivo CEM cells
Then we investigated whether a Fas-mediated mechanism was involved in the in vivo HIV-1-induced apoptosis of CEM cells. We first explored the ability of both IIIB and SF162 HIV-1 strains to induce apoptosis of ex vivo CEM cells as compared to the parental cells. We observed that, at 48 h after virus challenge, both IIIB and SF162 induced a marked increase in the percentage of apoptotic cells as compared to the uninfected ex vivo CEM cells, while the parental CEM cells did not undergo apoptosis either spontaneously or after HIV-1 challenge (Figure 3A). Of interest, the values obtained with the acute infection of ex vivo CEM cells in culture condition were comparable to those observed in CEM cells collected from the s.c. tumors infected in vivo (shown in Figure 1B).
Role of Fas/Fas-L interaction in the HIV-induced apoptosis of ex vivo CEM cells. (A) Induction of apoptosis by HIV-1 in vitro infection of parental (upper panel) or ex vivo (lower panel) CEM cells, analyzed by flow cytometry at 48 h postinfection. (B) Flow cytometric analysis of Fas-L expression in parental CEM cells as compared to uninfected or infected ex vivo CEM cells, at 48 h postinfection. (C) Effect of an anti-Fas blocking mAb (+αFas) on apoptosis in uninfected (CTR) (upper panel) or HIV-1 infected (HIV) (lower panel) ex vivo CEM cells, analyzed by flow cytometry at 48 h postinfection. All the results are representative of five separate experiments
The marked upregulation of Fas-L induced by HIV-1 infection (see Figure 2D) strongly suggested that a Fas-mediated mechanism was involved in the viral-induced apoptosis of ex vivo CEM cells. Thus, we firstly assessed the FasL expression on ex vivo CEM cells at 48 h after virus challenge, as compared to uninfected ex vivo and parental CEM cells. The results clearly showed that HIV-1 infection induced a significant increase of FasL expression in ex vivo CEM cells using either SF162 (Figure 3B) or IIIB (data not shown) viral strains. To further explore the role of the Fas-pathway in the HIV-induced apoptosis in these cells, we treated ex vivo CEM cells with a blocking anti-Fas mAb contemporaneously to the HIV-1 infection and analyzed the percentage of apoptotic cells at 48 h. This set of experiments was performed exclusively with the SF162 M-tropic strain of HIV-1, in that the IIIB T-tropic strain progressively induced the well known cytopathic effect25 in both parental and ex vivo CEM cells. Thus, in order to avoid that virus-induced cytopathic effect may overlap the Fas-mediated apoptosis, we used SF162 as a virus prototype of Fas-induced apoptosis. The results showed that treatment with the blocking anti-Fas mAb did not significantly affect the background level of apoptosis in uninfected ex vivo CEM cells (Figure 3C, upper panel), while virtually abolished the increase of apoptosis induced by HIV-1 infection in ex vivo CEM cells (Figure 3C, lower panel). To further define the role of Fas/Fas-L in the HIV-induced apoptosis of ex vivo CEM cells, we performed in situ immunocytochemical studies. Firstly, the results confirmed that, at 48 h post-infection, the vast majority of ex vivo CEM cells were apoptotic (70–80%) (Figure 4A). Moreover, approximately 50–60% of apoptotic cells were Fas-L+ (Figure 4B) and the HIV-1-infected cells did not show apoptotic staining of the nuclei (Figure 4C). Furthermore, the apoptotic cells highly outnumbered the HIV-infected cells (70–80% versus 5–10%) (Table 1). Double staining experiments using flow cytometry or immunocytochemistry showed that the vast majority of Fas-L+ CEM cells were also Fas+ (data not shown).
Immunocytochemical analysis of apoptosis, Fas-L expression and HIV-1 infection. (A) Apoptotic cells in cultures of HIV-1-infected ex vivo CEM cells (Cytospin preparation; Tunel Reaction+APAAP method, using NBT as chromogen) (×450 original magnification); (B) Double staining for Fas-L (orange) and Tunel Reaction (dark blue) in HIV-1-infected ex vivo CEM cells (Cytospin preparation; PAP versus APAAP methods respectively) (×850 original magnification), (C) Double staining for p24 (red) and Tunel reaction (dark blue). Tunel positive apoptotic bodies within and out the cells are shown (Cytospin preparation; APAAP method using fast red and NBT respectively as chromogen) (×850 original magnification)
Low level chronic infection leads to resistance to spontaneous apoptosis
We then observed the behavior of uninfected and HIV-infected ex vivo CEM cells maintained in culture conditions. Of interest, the effects of the IIIB (T-tropic) strain of HIV-1 on ex vivo CEM cells highly differed from that of the SF162 (M-tropic) strain. In fact, the IIIB strain induced a massive cytopathic effect in ex vivo CEM cell cultures 8–10 days after in vitro infection, while the infection with SF162 HIV-1 strain did not induce in ex vivo CEM cell cultures cytopathic effect up to 30 days after infection (data not shown). Thus, we studied the apoptotic behavior of ex vivo CEM cells infected with the SF162 strain of HIV and maintained in culture conditions for 30 days, as compared to the ex vivo uninfected cells. The results firstly showed that ex vivo CEM cells infected with the SF162 strain of HIV-1 progressively lost their susceptibility to spontaneous apoptosis at 20–30 days post infection, while uninfected CEM cells maintained marked levels of spontaneous apoptosis (Figure 5). To further confirm these data we cloned SF162-infected ex vivo CEM cells, obtaining infected and uninfected clones. The results showed that all the SF162-infected clones exhibited levels of spontaneous apoptosis significantly lower than the uninfected clones (8–12% versus 19–25% respectively), suggesting that chronic infection with a M-tropic strain of HIV-1 induced an anti-apoptotic state in infected ex vivo CEM cells. To further explore this issue, we evaluated the expression of the anti-apoptotic complex Bcl-2/Bcl-xL/Bax in uninfected and SF162-infected ex vivo CEM cells. The RT–PCR analysis showed that there were no differences in the expression of Bcl-2, Bcl-xL and Bax mRNA between infected and uninfected ex vivo CEM cells and between infected and uninfected ex vivo CEM cells clones (data not shown). Flow cytometric analysis showed only a slight but significant increase in the percentage of Bcl-2+ cells in the SF162-infected ex vivo CEM cells, as compared to the uninfected cells (Figure 6A). However, the most impressive differences were detected by the in situ immunocytochemical analysis. In fact, the distribution of Bcl-2 highly differed between infected and uninfected cells. Ninety to 95% of SF162-infected cells showed an intense and diffuse cytoplasmic staining while virtually all the uninfected ex vivo CEM cells showed a highly localized pre-Golgi/perinuclear staining for Bcl-2 (Figure 6B, upper panel). Notably, the mitochondrial distribution did not differ between infected and uninfected cells (Figure 6B, lower panel). Both flow cytometry and immunocytochemistry showed that infected cells expressed Fas-L at lower level than uninfected cells at this time, while Fas expression did not differ between infected and uninfected cells (data not shown). Notably, either HIV-1-infected ex vivo CEM cells or clones were reinoculated s.c. in SCID mice resulting in the development of highly productive (500±150 pg/ml p24 serum levels) tumors within 20–30 days (data not shown), suggesting that in vivo or ex vivo selection of mutants with defective viruses did not occur in our experiments.
Apoptosis in HIV-infected and uninfected ex vivo CEM cells maintained in cultures for 30 days. Percentages of apoptotic cells in uninfected ([open box]) and SF162 HIV-1 strain-infected ([hatched box]) ex vivo CEM cells at 1 day and at 30 days postinfection, analyzed by flow cytometry. Histograms are means±S.E.M. of five separate experiments
Bcl-2 expression and cellular distribution in HIV-infected and uninfected ex vivo CEM cells maintained in cultures for 30 days. (A) Flow cytometric analysis of the percentage of Bcl-2 positive cells in uninfected (dotted lines) and HIV-infected (solid lines) ex vivo CEM cells maintained in culture for 30 days; (‘B) Immunocytochemistry for Bcl-2 (upper panel) and mitochondria (lower panel) in HIV-1-infected (left panel) and uninfected (right panel) ex vivo CEM cells maintained in culture for 30 days. Arrows point to pre-golgi/perinuclear distribution of Bcl-2 in uninfected ex vivo CEM cells. Ninety to 95% of HIV-1-infected ex vivo CEM cells showed a more intense staining, widely distributed to the cytoplasm (left panel). (Cytospin preparation; APAAP method with fast red as chromogen+H&H counterstaining) (×850 original magnification). Results are representative of four separate experiments
Discussion
The initial observation, which led to the ensemble of studies reported in this article, consisted in a marked delay in the growth of CEM s.c. tumors in SCID mice, after an acute HIV-1 infection. Further analysis showed that CEM cells obtained from uninfected s.c. tumors exhibited a certain level of spontaneous apoptosis and that HIV-1 infection markedly increased these baseline levels of apoptosis. We compared the phenotype of parental CEM cells (maintained in culture condition) to CEM cells obtained from SCID mice tumors (ex vivo CEM). The results showed that ex vivo CEM cells, differently to the parental cells, exhibited the memory phenotype (CD45RO+) and a sort of apoptotic phenotype characterized by: (i) spontaneous apoptosis; (ii) induced expression of Fas-L; (iii) reduced expression of Bcl-2. Both T-tropic and M-tropic strains of HIV-1 induced a marked increase of Fas-L expression and apoptosis in ex vivo CEM cells as early as 2 days post-infection. Moreover, the HIV-1-induced apoptosis was Fas-mediated and involved Fas/Fas-L+ uninfected cells. These findings strongly suggest that: (i) HIV-1 induces apoptosis of CD4+ T cells already prone to undergo apoptosis; (ii) HIV-1 induces a Fas-mediated autocrine fratricide/suicide of uninfected CD4+ T lymphocytes. Thus, some of our data appear to be consistent with recent reports showing that: (i) CD4+ T cells with low levels of Bcl-2 are highly susceptible to HIV-1-induced apoptosis; 26,27 (ii) HIV-1-induced apoptosis may be Fas-mediated28,29,30,31,32,33,34,35,36 and occurs predominantly in bystander cells.5,7,35 Notably, given the specific features of this model, the HIV-1-induced Fas-mediated apoptosis of uninfected cells occurs in a homotypic system of CD4+ T cells, suggesting that HIV-1 infection may trigger an autocrine suicide of CD4+ T lymphocytes without the participation of Fas-L expressing macrophages or CTL.37 The possibility that apoptosis can occur through a Fas/Fas-L-mediated autocrine suicide has been proposed in lymphocyte38,39,40 and in other cell systems.41,42 Here we show that the in vivo acquired pathway of spontaneous apoptosis is associated with the expression of the memory (CD45RO+) phenotype on CEM cells. This is consistent with some reports showing that CD4+ memory T cells are generally more susceptible to apoptosis than naive T cells.43,44 Even though the role of memory T cells in CD4+ T cell depletion is controversial,45 it is of interest to mention that some in vitro studies have shown that memory T cells are depleted by apoptosis more rapidly than naive T cells following HIV infection.11,46,47,48 Of interest, some body districts, such as intestinal mucosa, are particularly rich in CD4+ memory T cells and a consistent rate of Fas-mediated spontaneous apoptosis normally occurs in these districts.49 We have recently shown that human intestinal CD4+ T cells are naturally permissive to a long lasting HIV-1 infection, which is highly related to the memory phenotype, as well as to the expression of HIV-1 co-receptors and to a baseline state of activation.50 Notably, it has been reported that loss of CD4+ T cells in intestinal mucosa precedes the appearance of CD4+ T cell depletion in the peripheral blood of asymptomatic HIV infected patients.51 Taking into consideration all these findings, it is conceivable that activated memory CD4+ T cells are the preferential target for both HIV-1 infection and apoptosis-mediated CD4+ T lymphocyte depletion in AIDS patients.
In the present study, we have also explored the long-term effects of HIV-1 on ex vivo CEM cells by maintaining infected cells in culture for 20–30 days. The results have revealed a scenario of events dramatically different from that of the first 2 days post-infection. First, the T-tropic strain of HIV-1 induced a massive cytopathic effect in ex vivo CEM cells within the first 7–10 days of culture. The cytopathic effect induced by T-tropic strains of HIV-1 is a well known phenomenon due to the formation of enormous syncytia through a continuous virus-induced cell-to-cell-to-syncytia fusion.25 In contrast, the M-tropic strains of HIV did not induce any cytopathic effect, thus enabling us to investigate the effect of long lasting HIV-1 infection on apoptosis. Our results showed that: (i) the rate of spontaneous apoptosis progressively declined during time in culture, reaching values significantly lower than those of uninfected cells at 30 days of culture; (ii) the decrease of spontaneous apoptosis was associated with increased levels and diffuse cytoplasmic distribution of Bcl-2, as well as with lower levels of Fas-L, in infected ex vivo CEM cells as compared to the uninfected counterparts. It is well established that Bcl-2 protects cells from apoptosis.52 However, the precise subcellular localization of bcl2 and its importance in the modulation of programmed cell death are both unresolved problems. Particularly, bcl2 has been identified at the inner53 and the outer54,55 mitochondrial membrane, the endoplasmic reticulum,56,57 the nuclear membrane54,57 and close to the nuclei.58 Variation in the cellular distribution of bcl2 protein is associated with different susceptibility to apoptosis.58 Consistently with our data, resistance to apoptotic cell death is associated with a wide distribution of Bcl-2 within the cell, while the distribution of Bcl-2 to the perinuclear area is associated with an increased susceptibility to spontaneous apoptosis.58 The subcellular distribution of Bcl-2 is considered to be a crucial event in allowing interactions with the other apoptosis regulatory proteins (e.g. Bax). Thus, the wider distribution of Bcl-2 protein in HIV-1 infected ex vivo CEM cells could well explain their increasing resistance to spontaneous apoptosis.
Thus, these results appear to be consistent with the hypothesis that HIV-1 may in vivo prevent apoptosis through Bcl-2 mediated mechanisms until high levels of virus are produced. In this regard, it is worth mentioning that small amounts of some HIV-1-proteins have been shown to prevent or delay death of infected cells through various antiapoptotic mechanisms.2 As an example, low levels of endogenous expression of HIV-1 vpr can protect CD4+ T cells from apoptotic stimuli (including Fas pathway) through upregulation of Bcl-2.59 Moreover, our results suggest that a bcl2-mediated mechanism may render CD4+ T cells particularly susceptible to HIV-1-mediated CD4+ T cell death via a Fas pathway.60
In conclusion, our results, obtained in a model of SCID mice transplanted with CEM cells, are strongly reminiscent of a series of events possibly occurring in HIV-1 infected individuals. Particularly, our data indicate that an acute HIV-1 infection can induce a rapid CD4+ T lymphocyte depletion through a massive Fas-mediated autocrine suicide of differentiated memory CD4+ T cells, infecting a relative low number of lymphocytes. Following this dramatic scenario, CD4+ T lymphocytes infected with M-tropic strains of HIV-1, that do not induce cytopathic effect and predominate in the early phases of AIDS,61 undergo a chronic infection becoming resistant to apoptosis through the development of an efficient survival program. Notably, the dynamics of CD4+ T cell differentiation and cell phenotype, possibly shaped by the cytokine environment,62 may continuously change the CD4+ T cell permissiveness to HIV-1 strains which use CCR5 or CXCR4 as coreceptors. Thus, on one hand, HIV-1 may induce a massive Fas-mediated autocrine suicide/fratricide of uninfected CD4+ memory T cells during acute infection. On the other hand, HIV may inhibit or at least delay spontaneous apoptosis in chronically infected CD4+ T cells allowing a long lasting viral production. These cells may constitute a pool of latently infected CD4+ T cells that are rapidly established during primary infection23 and are resistant to highly active antiretroviral therapy.24
Lastly, these data emphasize the usefulness and versatility of human-SCID mouse models in investigating in vivo the relationships between T cell differentiation, HIV-1 infection and the mechanisms underlying CD4+ T cell depletion.
Materials and Methods
Growth of CEM cell-tumors in SCID mice and in vivo HIV-1 infection
CB.17 SCID/SCID female mice (Charles River, Milan, Italy) were used at 4–5 weeks of age and were kept under specific pathogen-free conditions. SCID mice were housed in microisolator cages and all food, water and bedding were autoclaved prior to use. The animal studies were performed in biosafety level three facility. Mice were injected subcutaneously (s.c.) in the shoulder with 20×106uninfected CEM cells63 resuspended in 0.2 ml RPMI 1640 medium. The two major diameters of each tumor nodule were measured by callipers and the mean tumor diameter was calculated for each tumor. To deplete animals of some residual reactivity, SCID mice were injected i.p. with 0.2 ml of a monoclonal anti-mouse granulocyte antibody (RB6-8C5 hybridoma), 1 day before, 3 and 7 days after cell injection, as previously described.63
The in vivo HIV infection of CEM-SCID mice was performed with a simultaneous s.c. injection of 20×106 uninfected CEM cells with 106 TCID50 cell-free virus. The viral strains used in these experiments were: HIV-1IIIB and HIV-1SF162. In all conditions, the HIV-infected chimeras were sacrificed when the tumors reached 20–25 mm mean diameter and analyzed for the virus replication at the tumor site and p24 antigenemia.
Detection of viral infection
At sacrifice, the CEM cell tumors were excised. To obtain single cell suspension tumors were carefully minced, mechanically disrupted with the blunt end of a 5-ml syringe plug and filtered. The single cell suspensions were washed twice in RPMI 1640 medium. Cell suspensions underwent: (i) HIV-1 DNA-PCR as previously described;19 (ii) HIV-1 RT–PCR, using specific primers which detect all viral RNAs, as reported elsewhere;64 (iii) FACS analysis for human cells markers and apoptosis. Sera of infected animals were tested for HIV p24 antigen by an antigen capture enzyme-linked immunosorbent assay (Dupont, B-1130 Bruxelles, Belgium).
Cell culture and in vitro HIV-1 infection
Parental CEM cells (ATCC, Rockville, MD, USA) as well as CEM cells collected from s.c. tumors of SCID mice (ex vivo CEM cells) were cultured in RPMI 1640 medium supplemented with 10% heat-inactivated fetal calf serum. Cells were seeded at 2×105/ml and passaged every 3 days. For in vitro HIV-1 infection cells were pelleted and incubated with the virus inoculum at 0.1 M.O.I. for 1 h at 37°C, washed three times and cultured in complete medium. The virus stocks were derived from clarified culture medium of PHA-stimulated HIV-1-infected PBMC, frozen at −140°C. Titers were determined by standard end-point dilution methods. The virus strains used in these experiments were: HIV-1IIIB, HIV-1SF162.
Cell cloning
CEM cells obtained from subcutaneous tumors were exposed to HIV-1SF162 virus strain at 1 M.O.I. for 1 h at 37°C, then washed extensively, and seeded in complete medium at a concentration of 0.5 cell/well in a 96-microwell cell culture plate. After 2 weeks pure clones were screened for virus infection by PCR. Infected as well as uninfected clones were propagated for further analyses as described.65
Western blot analysis
Cell extracts were resuspended in SDS sample buffer, denaturated by boiling and separate on 8% SDS–PAGE gels. Then, proteins were transferred to Hybond C Extra (Amersham Pharmacia Biotech, NY, USA) and blocked in 5% milk overnight. Bcl-2 was detected with an anti-Bcl-2 monoclonal antibody (Santa Cruz, CA, USA) and visualized with peroxidase anti-Ig followed by ECL (Pierce, SuperSignal Substrate, Rockford, IL, USA). Immunoblotting for actin protein (Chemicon, CA, USA) was performed to normalize the level of proteins in all the samples.
Flow cytometry and apoptosis detection
CEM cells were washed twice with phosphate-buffered saline and stained for 30 min with the appropriate monoclonal antibody at 4°C. The monoclonal antibodies used were anti-CD45RA FITC, anti-CD45RO PE (Becton Dickinson, Mountain View, San Diego, CA, USA), anti-FAS PE (Becton Dickinson, San Diego, CA, USA), anti-FAS-L (NOK-1, Pharmingen, CA, USA), anti-Bcl-2 (Neomarkers, Fremont, CA, USA). An anti-mouse IgG mAb PE (SIGMA) was used for indirect staining. Seventy per cent ethanol treatment was used to permeabilize cells before staining for Bcl-2. After staining cells were fixed with 2% paraformaldehyde and analyzed on a FACSORT cytometer (Becton Dickinson) equipped with a 488 nm argon laser. Data were recorded and analyzed by using LYSIS II software (Becton Dickinson). The analysis was performed by gating ex vivo CEM cells using forward and side scatter characteristics, to avoid SCID mouse cell contamination.
Apoptotic cells were detected by labeling DNA strand breaks with FITC-dUTP by terminal transferase (TUNEL reaction) (‘In situ cell death detection kit’, Boehringer Mannheim). Briefly 106 cells were fixed with 4% paraformaldehyde, permeabilized with 0.1% Triton X-100, 0.1% sodium cytrate and labeled at 37°C for 60 min with TUNEL reaction mixture as recommended by the manufacturer. Apoptosis was evaluated directly by flow cytometry.
Fas blocking
Ex vivo CEM cells were infected with HIV-1IIIB or HIV-1SF162 strains in the absence or in the presence of an anti-Fas ZB4 neutralizing mAb (10 μg/ml) (UBI, NY, USA). Apoptosis was evaluated by FACS analysis 48 h postinfection.
RT–PCR for apoptotic regulating genes
mRNA for human pro-apoptotic and anti-apoptotic genes (Fas, Fas-L, Bcl-2, Bax, Bcl-xL) were detected in CEM cells by RT–PCR as previously described19 with specific primer pairs: Fas-L 5′ CAGCTCTTCCACCTACAGAAGGAG, 3′ CAGAGAGAGCTCAGATACGTTGAC; primers specific for Fas, Bcl-2, Bax, Bcl-xL are reported elsewhere.66,67,68,69 The samples were amplified for 30–35 cycles at the following conditions: 94°C 40 s, 62°C 40 s, 72° 40 s. β2-microglobulin RT–PCR19 was run in parallel to normalize the levels of human RNA in all the samples.
Immunocytochemistry
Cell suspensions from the tumors were spun onto glass slides (Shandon, Cheshire, UK) or attached to L-polylysine-covered glass chamber slides (Labtek Naperville, IL, USA),70 and stained by immunocytochemistry for HIV-p55/p18 (anti-HIV-p55/p18 IgG1, clone 11H9, from Medical Research Council AIDS Reagent Project, London, UK), Fas (Pierce, Rockford, IL, USA), Fas-L (Pharmigen, San Diego, CA, USA), Bcl-2 (Biomeda, Foster City, CA, USA), mitochondria (Chemicon, CA, USA) and TUNEL reaction (‘In situ cell death detection kit′ Boehringer Mannheim),71 using the alkaline phosphatase anti-alkaline phosphatase (APAAP) (Dako, Denmark) method or the peroxidase-anti-peroxidase (PAP) (Dako, Denmark) method, in single and double staining, as appropriate.70
Abbreviations
- HIV:
-
Human Immunodeficiency Virus
- AIDS:
-
acquired immunodeficiency syndrome
- SCID:
-
Human-severe combined immunodeficient
- SI:
-
syncytium-inducing
- NSI:
-
non syncytium-inducing
- T-tropic:
-
T lymphocyte-tropic
- M-tropic:
-
monocyte-tropic
References
Fauci AS, Pantaleo G, Stanley S and Weissman D . 1996 Immunophatogenic mechanism of HIV infection. Ann. Intern. Med. 124: 654–663
Casella CR and Finkel TH . 1997 Mechanisms of lymphocyte killing by HIV. Curr. Opin. Hematol. 4: 24–31
Evans LA and Levy JA . 1989 Characteristics of HIV infection and pathogenesis. Biochim. Biophys. Acta. 989: 237–254
Nardelli B, Gonzales CJ, Schechter M and Valentine FT . 1995 CD4+ blood lymphocytes are rapidly killed in vitro by contact with autologous human immunodeficiency virus-infected cells. Proc. Natl. Acad. Sci. USA 92: 7312–7316
Finkel TH, Tudor-Williams G, Banda NK, Cotton MF, Curiel T, Monks C, Baba TW, Ruprecht RM and Kupfer A . 1995 Apoptosis occurs predominantly in bystander cells and not in productively infected cells of HIV- and SIV-infected lymph nodes. Nat. Med. 1: 129–134
Herbein G, Van Lint C, Lovett JL and Verdin E . 1998 Distinct mechanisms trigger apoptosis in human immunodeficiency virus type 1-infected and in uninfected bystander T lymphocytes. J. Virol. 72: 660–670
Carbonari M, Pesce AM, Cibati M, Modica A, Dell'Anna L, D'Offizi G, Angelici A, Uccini S, Modesti A and Fiorilli M . 1997 Death of bystander cells by a novel pathway involving early mitochondrial damage in human immunodeficiency virus-related lymphadenopathy. Blood 90: 209–216
Schnittman SM, Lane HC, Greenhouse J, Justement JS, Baseler M and Fauci S . 1990 Preferential infection of CD4+ memory T cells by human immunodeficiency virus type 1: evidence for a role in the selective T-cell functional defects observed in infected individuals. Proc. Natl. Acad. Sci. USA 87: 6058–6062
Woods TC, Roberts BD, Butera ST and Folks TM . 1997 Loss of inducible virus in CD45RA naive cells after human immunodeficiency virus-1 entry accounts for preferential viral replication in CD45RO memory cells. Blood 89: 1635–1641
Spina CA, Prince HE and Richman DD . 1997 Preferential replication of HIV-1 in the CD45RO memory cell subset of primary CD4 lymphocytes in vitro. J. Clin. Invest. 99: 1774–1785
Heinkelein M, Muller M, Kutsch O, Sopper S and Jassoy C . 1997 Rapid and selective depletion of CD4+ T lymphocytes and preferential loss of memory cells on interaction of mononuclear cells with HIV-1 glycoprotein-expressing cells. J. Acquir. Immune Defic. Syndr. Hum. Retrovirol. 16: 74–82
McCune JM . 1988 The SCID-hu mouse: murine model for the analysis of human hematolymphoid differentiation and function. Science 24: 1632–1639
Mosier DE, Gulizia RJ, Baird SM and Wilson DB . 1988 Transfer of functional human immune system to mice with severe combined immunodeficiency. Nature 335: 256–259
McCune JM, Namikawa R, Shih CC, Rabin L and Kaneshima H . 1990 Suppression of HIV infection in AZT-treated SCID-hu mice. Science 247: 564–566
Namikawa R, Kanemisha H, Lieberman M, Weissman IL and McCune JM . 1991 Infection of the SCID-hu mouse by HIV-1. Science 242: 1684–1686
Mosier DE, Gulizia RJ, Baird SM, Wilson DB, Spector DH and Spector SA . 1991 Human immunodeficiency virus infection of human PBL-SCID mice. Science 25: 791–794
Mosier DE, Gulizia RJ, MacIsaac PD, Torbett BE and Levy JA . 1993 Rapid loss of CD4+ T cells in Human-PBL-SCID mice by noncytopathic HIV isolates. Science 260: 689–692
McCune JM . 1997 Animal models of HIV-1 disease. Science 278: 2141–2142
Rizza P, Santini SM, Logozzi M, Lapenta C, Sestili P, Gherardi G, Lande R, Spada M, Parlato S, Belardelli F and Fais S . 1996 T-cell dysfunction in hu-PBL-SCID mice infected with human immunodeficiency virus (HIV) shortly after reconstitution: in vivo effects of HIV on highly activated human immune cells. J. Virol. 70: 7958–7964
Tary-Lehman M, Saxon A and Lehman PV . 1995 The human immune system in hu-PBL-SCID mice. Immunol Today 16: 529–533
Uittembogaart CH, Anisman DJ, Tary-Lehmann M, Vollger LW, Breit TM, Van Dongen JJM and Saxon A . 1994 The SCID mouse environment causes immunophenotypic changes in human immature T-cell lines. Int. J. Cancer 56: 546–551
Lapenta C, Parlato S, Spada M, Santini SM, Rizza P, Logozzi M, Proietti E, Belardelli F and Fais S . 1998 Human lymphoblastoid CD4+ T cells become permissive to macrophage-tropic strains of HIV-1 after passage into severe combined immunodeficient (SCID) mice through in vivo upregulation of CCR5: role of in vivo dynamics of CD4+ T cell differentiation in the pathogenesis of AIDS. J. Virol. 72: 10323–10327
Chun TW, Engel D, Berrey MM, Shea T, Corey L and Fauci AS . 1998 Early establishment of a pool of latently infected, resting CD4(+) T cells during primary HIV-1 infection. Proc. Natl. Acad. Sci. USA 95: 8869–8873
Finzi D, Hermankova M, Pierson T, Carruth LM, Buck C, Chaisson RE, Quinn TC, Chadwick K, Margolick J, Brookmeyer R, Gallant J, Markowitz M, Ho DD, Richman DD and Siliciano RF . 1997 Identification of a reservoir for HIV-1 in patients on highly active antiretroviral therapy. Science 278: 1295–1300
Fais S, Burgio VL, Capobianchi MR, Gessani S, Pallone F and Belardelli F . 1997 The biological relevance of polykaryons in the immune response. Immunol. Today 18: 522–527
Hashimoto F, Oyaizu N, Kalyanaraman VS and Pahwa S . 1997 Modulation of Bcl-2 protein by cross-linking: a possible mechanism for lymphocyte apoptosis in human immunodeficiency virus infection and for rescue of apoptosis by interleukin-2. Blood 90: 745–753
Ledru E, Lecoeur H, Garcia S, Debord T and Gougeon ML . 1998 Differential susceptibility to apoptosis among peripheral Th1 subset: correlation with bcl-2 expression and consequences for AIDS pathogenesis. J. Immunol. 160: 3194–3206
Katsikis PD, Wunderlich ES, Smith CA, Herzenberg LA and Herzenberg LA . 1995 Fas antigen stimulation induces marked apoptosis of T lymphocytes in human immunodeficiency virus-infected individuals. J. Exp. Med. 181: 2029–2036
Silvestris F, Cafforio P, Frassanito MA, Tucci M, Romito A, Nagata S and Dammacco F . 1996 Overexpression of Fas antigen on T cells in advanced HIV-1 infection: differential ligation constantly induces apoptosis. AIDS 10: 131–141
Baumler CB, Bohler T, Herr I, Benner A, Krammer PH and Debatin KM . 1996 Activation of the CD95 (APO-1/Fas) system in T cell from human immunodeficiency virus type-1-infected children. Blood 88: 1741–1746
Sloand EM, Young NS, Kumar P, Weichold FF, Sato T and Maciejewski JP . 1997 Role of Fas ligand and receptor in the mechanism of T-cell depletion in acquired immunodeficiency syndrome: effects on CD4+ lymphocyte depletion and human immunodeficiency virus replication. Blood 89: 1357–1363
Badley AD, Dockrell DH, Algeciras A, Ziesmer S, Landay A, Lederman MM, Connick E, Kessler H, Kuritzkes D, Lynch DH, Roche P, Yagita H and Paya CV . 1998 In vivo analysis of Fas/FasL interactions in HIV-infected patients. J. Clin. Invest. 102: 79–87
Mitra D, Steiner M, Lynch DH, Staiano-Coico L and Laurence J . 1996 HIV-1 upregulates Fas ligand expression in CD4+ T cells in vitro and in vivo: association with Fas-mediated apoptosis and modulation by aurintricarboxylic acid. Immunology 87: 581–585
Bahr GM, Capron A, Dewulf J, Nagata S, Tanaka M, Bourez JM and Mouton Y . 1997 Elevated serum level of Fas ligand correlates with the asymptomatic stage of human immunodeficiency virus infection. Blood 90: 896–898
Badley AD, McElhinny JA, Leibson PJ, Lynch DH, Alderson MR and Paya CV . 1996 Upregulation of Fas ligand expression by human immunodeficiency virus in human macrophages mediated apoptosis of uninfected T lymphocytes. J. Virol. 70: 199–206
Dockrell DH, Badley AD, Villacian JS, Heppelman CJ, Algeciras A, Ziesmer S, Yagita H, Lynch DH, Roche PC, Leibson PJ and Paya CV . 1998 The expression of Fas ligand by macrophages and its upregulation by human immunodeficiency virus infection. J. Clin. Invest. 101: 2398–2405
Garcia S, Fevrier M, Dadaglio G, Lecoeur H, Riviere Y and Gougeon ML . 1997 Potential deleterious effect of anti-viral cytotoxic lymphocyte through the CD95 (FAS/APO-1)-mediated pathway during chronic HIV infection. Immunol. Lett. 57: 53–58
Dhein J, Walczak H, Baumler C, Debatin KM and Krammer PH . 1995 Autocrine T-cell suicide mediated by APO-1(Fas/CD95). Nature 373: 438–441
Nagata S and Sada T . 1995 Fas and Fas ligand: lpr and gld mutations. Immunol. Today 16: 39–43
Su X, Cheng J, Liu W, Liu C, Wang Z, Yang P, Zhou T and Mountz JD . 1998 Autocrine and paracrine apoptosis are mediated by differential regulation of Fas ligand activity in two distinct Jurkat T cell populations. J. Immunol. 160: 5288–5293
Giordano C, Stassi G, De Maria R, Todaro M, Richiusa P, Papoff G, Ruberti G, Bagnasco M, Testi R and Galluzzo A . 1997 Potential involvement of Fas and its ligand in the pathogenesis of Hashimoto's thyroiditis. Science 275: 960–963
Buechner SA, Wernli M, Harr T, Hahn S, Itin P and Erb P . 1997 Regression of basal cell carcinoma by intralesional interferon-alpha treatment is mediated by CD95 (Apo-1/Fas)-CD95 ligand-induced suicide. J. Clin. Invest. 100: 2691–2696
Salmon M, Pilling D, Borthwick NJ, Viner N, Janossy G, Bacon PA and Akbar AN . 1994 The progressive differentiation of primed T cells is associated with an increasing susceptibility to apoptosis. Eur. J. Immunol. 24: 892–899
Akbar AN, Borthwick N, Salmon M, Gombert W, Bofill M, Shamsadeen N, Pilling D, Pett S, Grundy JE and Janossy G . 1993 The significance of low bcl-2 expression by CD45RO T cells in normal individuals and patients with acute viral infection. The role of apoptosis in T cell memory. J. Exp. Med. 178: 427–438
Wang L, Chen JJ, Gelman BB, Konig R and Cloyd MW . 1999 A novel mechanism of CD4 lymphocyte depletion involves effects of HIV on resting lymphocytes: induction of lymph node homing and apoptosis upon secondary signaling through homing receptors. J. Immunol. 162: 268–276
Bohler T, Nedel S and Debatin KM . 1997 CD95-induced apoptosis contributes to loss of primed/memory but not resting/naive T cells in children infected with human immunodeficiency virus type 1. Pediatr. Res. 41: 878–885
Chun TW, Chadwick K, Margolick J and Siliciano RF . 1997 Differential susceptibility of naive and memory CD4+ T cells to the cytopathic effects of infection with human immunodeficiency virus type 1 strain LAI. J. Virol. 71: 4436–4444
Gougeon ML, Lecoeur H, Dulioust A, Enouf MG, Crouvoiser M, Goujard C, Debord T and Montagnier L . 1996 Programmed cell death in peripheral lymphocytes from HIV-infected persons: increased susceptibility to apoptosis of CD4 and CD8 T cells correlates with lymphocyte activation and with disease progression. J. Immunol. 156: 3509–3520
De Maria R, Boirivant M, Cifone MG, Roncaioli P, Hahne M, Tschopp J, Pallone F, Santoni A and Testi R . 1996 Functional expression of Fas and Fas ligand on human gut lamina propria T lymphocytes. J. Clin. Invest. 97: 316–322
Lapenta C, Boirivant M, Marini M, Santini SM, Logozzi M, Viora M, Belardelli F and Fais S . 1999 Human intestinal lamina propria lymphocytes are naturally permissive to HIV-1 infection. Eur. J. Immunol. 29: 1202–1208
Schneider T, Jahn HU, Schmidt W, Riecken EO, Zeitz M and Ullrich R . 1995 Loss of CD4 T lymphocytes in patients infected with human immunodeficiency virus type 1 is more pronounced in the duodenal mucosa than in the peripheral blood. Berlin Diarrhea/Wasting Syndrome Study Group. Gut 37: 524–529
Nunez G, Merino R, Grillot D and Gonzales-Garcia M . 1994 Bcl-2 and Bcl-x: Regulatory switches for lymphoid death and survival. Immunol. Today 15: 582–588
Hockenbery DM, Nunez G, Minniman RD, Schreiber RD and Korsmeyer SJ . 1990 Bcl-2 is an inner mitochondrial membrane protein that blocks programmed cell death. Nature 348: 334–336
Monaghan P, Robertson D, Andrew T, Amos S, Dyer MJS, Mason DY and Greaves MF . 1992 Ultrastructural localization of Bcl-2 protein. J. Histochem. Cytochem. 40: 1819–1825
Riparbelli MG, Callaini G, Tripodi SA, Cintorino M, Tosi P and Dallai R . 1995 Localization of the Bcl-2 protein to the outer mitochondrial membrane by electron microscopy. Exp. Cell. Res. 221: 363–369
Chen-Levy Z, Nourse J and Cleary ML . 1989 The bcl-2 candidate proto-oncogene product is a 24 kilodalton integral-membrane protein highly expressed in lymphoid cell lines lymphomas carrying the t(14;18) translocation. Mol. Cell. Biol. 9: 701–710
Akao Y, Otsuki YS, Kataoka S, Ito Y and Tsujimoto Y . 1994 Multiple subcellular localization of Bcl-2: detection in nuclear outer membrane, endoplasmic reticulum, and mitochondrial membrane. Cancer Res. 54: 2468–2471
Bruel A, Karsenty E, Schmid M, McDonnell TJ and Lanotte M . 1997 Altered sensitivity to retinoid-induced apoptosis associated with changes in the subcellular distribution of Bcl-2. Exp. Cell. Res. 233: 281–287
Conti L, Rainaldi G, Matarrese P, Varano B, Rivabene R, Columba S, Sato A, Belardelli F, Malorni W and Gessani S . 1998 The HIV-1 vpr protein acts as a negative regulator of apoptosis in a human lymphoblastoid T cell line: a possible implication for the pathogenesis of AIDS. J. Exp. Med. 187: 403–413
Scaffidi C, Fulda S, Srinivasan A, Friesen C, Li F, Tomaselli KJ, Debatin KM, Krammer PH and Peter ME . 1998 Two CD95 (APO-1) signaling pathway. EMBO J. 17: 1675–1687
Schuitemaker H, Koot M, Kootstra NA, Dercksen MW, de Goede REY, van Steenwijk RP, Lange JMA, Eeftink Schattenkerk JKM, Miedema F and Tersmette M . 1992 Biological phenotype of human immunodeficiency virus type 1 clones at different stage of infection: progression of disease is associated with a shift from monocytotropic to T-cell-tropic virus populations. J. Virol. 66: 1354–1360
Valentin A, Lu W, Rosati M, Schneider R, Albert J, Karlsson A and Pavlakis GN . 1998 Dual effect of interleukin 4 on HIV-1 expression: implications for viral phenotypic switch and disease progression. Proc. Natl. Acad. Sci. USA 95: 8886–8891
Santini SM, Spada M, Parlato S, Logozzi M, Lapenta C, Proietti E, Belardelli F and Fais S . 1998 Treatment of severe combined immunodeficiency (SCID) mice with anti-murine granulocyte monoclonal antibody improves human leukocyte xenotransplantation. Transplantation 65: 416–420
Lapenta C, Fais S, Rizza P, Spada M, Logozzi M, Parlato S, Santini SM, Pirillo M, Belardelli F and Proietti E . 1997 U937-SCID mouse xenografts: a new model for acute in vivo HIV-1 infection suitable to test antiviral strategies. Antiviral Res. 36: 81–90
Puddu P, Locardi C, Sestili P, Varano F, Petrini C, Modesti A, Masuelli L, Gresser I and Belardelli F . 1991 Human immunodeficiency virus (HIV)-infected tumor xenografts as an in vivo model for antiviral therapy: role of alpha/beta interferon in restriction of tumor growth in nude mice injected with HIV-infected U937 tumor cells. J. Virol. 65: 2245–2253
Tuosto L, Gilardini Montani MS, Lorenzetti S, Cundari E, Moretti S, Lombardi G and Piccolella E . 1995 Differential susceptibility to monomeric HIV gp120-mediated apoptosis in antigen-activated CD4+ T cell populations. Eur. J. Immunol. 25: 2907–2916
Mapara MY, Bargou R, Zugck C, Dohner H, Ustaoglu F, Jonker RR, Krammer PH and Dorken B . 1993 APO-1 mediated apoptosis or proliferation in human chronic with B lymphocytic leukemia: correlation with bcl-2 oncogene expression. Eur. J. Immunol. 23: 702–708
Akbar AN, Borthwick NJ, Wickremasinghe RG, Panayiotidis P, Pilling D, Bofill M, Krajewski S, Reed J and Salmon M . 1996 Interleukin-2 receptor common gamma-chain signaling cytokines regulate activated T cell apoptosis in response to growth factor withdrawal: selective induction of anti-apoptotic (bcl-2, bcl-xL) but not pro-apoptotic (bax, bcl-xS) gene expression. Eur. J. Immunol. 26: 294–299
Benito A, Silva M, Grillot D, Nunez G and Fernandez-Luna JL . 1996 Apoptosis induced by erythroid differentiation of human leukemia cell lines is inhibited by Bcl-xL . Blood 87: 3837–3843
Fais S, Capobianchi MR, Abbate I, Castilletti C, Gentile N, Cordiali Fei P, Ameglio F and Dianzani F . 1995 Unidirectional budding of HIV-1 at the site of cell-to-cell contact is associated with co-polarization of intercellular adhesion molecule-1 and HIV-1 viral matrix protein. AIDS 9: 329–335
Negoescu A, Lorimier P, Labat-Moleur F, Drouet C, Robert C, Guillermet C, Brambilla C and Brambilla E . 1996 In situ apoptotic cell labelling by the Tunel method: improvement and evaluation on cell preparations. J. Histochem. Cytochem. 44: 959–968
Acknowledgements
This work was supported by grants from the Italian Ministry of Health (Progetto di Ricerca sull'AIDS 1997, 10A/L). We are indebted to Angela Lippa for secretarial assistance.
Author information
Authors and Affiliations
Corresponding author
Additional information
Edited by ML Gougeon
Rights and permissions
About this article
Cite this article
Parlato, S., Santini, S., Lapenta, C. et al. Primary HIV-1 infection of human CD4+ T cells passaged into SCID mice leads to selection of chronically infected cells through a massive Fas-mediated autocrine suicide of uninfected cells. Cell Death Differ 7, 37–47 (2000). https://doi.org/10.1038/sj.cdd.4400586
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.cdd.4400586