Abstract
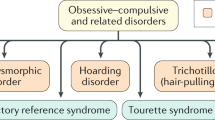
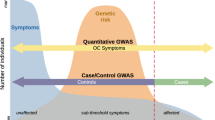
Obsessive–compulsive disorder (OCD) encompasses a broad range of symptoms representing multiple domains. This complex phenotype can be summarized using a few consistent and temporally stable symptom dimensions. The objective of this study was to assess the psychometric properties of the Dimensional Yale–Brown Obsessive–Compulsive Scale (DY-BOCS). This scale measures the presence and severity of obsessive–compulsive (OC) symptoms within six distinct dimensions that combine thematically related obsessions and compulsions. The DY-BOCS includes portions to be used as a self-report instrument and portions to be used by expert raters, including global ratings of OC symptom severity and overall impairment. We assessed 137 patients with a Diagnostic and Statistical Manual-IV diagnosis of OCD, aged 6–69 years, from sites in the USA, Canada and Brazil. Estimates of the reliability and validity of both the expert and self-report versions of the DY-BOCS were calculated and stratified according to age (pediatric vs. adult subjects). The internal consistency of each of the six symptom dimensions and the global severity score were excellent. The inter-rater agreement was also excellent for all component scores. Self-report and expert ratings were highly intercorrelated. The global DY-BOCS score was highly correlated with the total Yale–Brown Obsessive–Compulsive Scale score (Pearson r=0.82, P<0.0001). Severity scores for individual symptom dimensions were largely independent of one another, only modestly correlated with the global ratings, and were also differentially related to ratings of depression, anxiety and tic severity. No major differences were observed when the results were stratified by age. These results indicate that the DY-BOCS is a reliable and valid instrument for assessing multiple aspects of OCD symptom severity in natural history, neuroimaging, treatment response and genetic studies when administered by expert clinicians or their highly trained staff.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Kessler RC, Chiu WT, Demler O, Walters EE . Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry 2005; 62: 617–627.
Crino R, Slade T, Andrews G . The changing prevalence and severity of obsessive–compulsive disorder criteria from DSM-III to DSM-IV. Am J Psychiatry 2005; 162: 876–882.
Karno M, Golding JM . Obsessive–compulsive disorder. In: Robins LN, Regier DA (eds). Psychiatric Disorders in America: The Epidemiologic Catchment Area Study. The Free Press: New York, 1991; pp 204–219.
Murray CJ, Lopez AD . The global burden of disease: a comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 and projected to 2020. In: Murray CJ, Lopez AD (eds). Harvard University Press: Cambridge, MA, 1996.
Miguel EC, Leckman JF, Rauch S, do Rosario-Campos MC, Hounie AG, Mercadante MT et al. Obsessive–compulsive disorder phenotypes: implications for genetic studies. Mol Psychiatry 2005; 10: 258–275.
Rasmussen SA, Tsuang MT . Clinical characteristics and family history in DSM-III obsessive–compulsive disorder. Am J Psychiatry 1986; 143: 317–322.
Rosario-Campos MC, Leckman JF, Mercadante MT, Shavitt RG, Prado HS, Sada P et al. Adults with early-onset obsessive–compulsive disorder. Am J Psychiatry 2001; 158: 1899–1903.
Diniz JB, Rosario-Campos MC, Shavitt RG, Curi M, Hounie AG, Brotto SA et al. Impact of age at onset and duration of illness on the expression of comorbidities in obsessive–compulsive disorder. J Clin Psychiatry 2004; 65: 22–27.
Miguel EC, Baer L, Coffey BJ, Rauch SL, Savage CR, O'Sullivan RL et al. Phenomenological differences appearing with repetitive behaviours in obsessive–compulsive disorder. Br J Psychiatry 1997; 170: 140–145.
Miguel EC, do Rosario-Campos MC, Prado HS, do Valle R, Rauch SL, Coffey BJ et al. Sensory phenomena in obsessive–compulsive disorder and Tourette's disorder. J Clin Psychiatry 2000; 61: 150–156.
Leckman JF, McDougle CJ, Pauls DL, Peterson BS, Grice DE, King RA et al. Tic-related versus non-tic related obsessive–compulsive disorder. In: Goodman WK, Rudorfer MV, Mazur JD (eds). Obsessive–Compulsive Disorder: Contemporary Issues in Treatment. Lawrence Erlbaum: New York, 2000, pp 43–68.
Nestadt G, Addington A, Samuels J, Liang KY, Bienvenu OJ, Riddle M et al. The identification of OCD-related sub-groups based on comorbidity. Biol Psychiatry 2003; 53: 914–920.
Ravizza L, Maina G, Bogetto F . Episodic and chronic obsessive–compulsive disorder. Depress Anxiety 1997; 6: 154–158.
Andreasen NC, Arndt S, Alliger R, Miller D, Flaum M . Symptoms of schizophrenia. Methods, meanings, and mechanisms. Arch Gen Psychiatry 1995; 52: 341–351.
Liddle PF, Friston KJ, Frith CD, Hirsch SR, Jones T, Frackowiak RS . Patterns of cerebral blood flow in schizophrenia. Br J Psychiatry 1992; 160: 179–186.
Cassidy F, Forest K, Murry E, Carroll BJ . A factor analysis of the signs and symptoms of mania. Arch Gen Psychiatry 1998; 55: 27–32.
Alsobrook JP, Pauls DL . A factor analysis of tic symptoms in Gilles de la Tourette's Syndrome. Am J Psychiatry 2002; 159: 291–296.
Williamson DA, Womble LG, Smeets MAM, Netemeyer RG, Thaw JM, Kutlesic V et al. Latent structure of eating disorder symptoms: a factor-analytic and taxonomic investigation. Am J Psychiatry 2002; 159: 412–418.
Grigorenko EL, Wood FB, Meyer MS, Hart LA, Speed WC, Shuster A et al. Susceptibility loci for distinct components of developmental dyslexia on chromosomes 6 and 15. Am J Hum Genet 1997; 60: 27–39.
Mataix-Cols D, do Rosario-Campos MC, Leckman JF . A multidimensional model of obsessive–compulsive disorder. Am J Psychiatry 2005; 162: 228–238.
Leckman JF, Grice DE, Boardman J, Zhang H, Vitale A, Bondi C et al. Symptoms of obsessive–compulsive disorder. Am J Psychiatry 1997; 154: 911–917.
Mataix-Cols D, Rauch SL, Manzo PA, Jenike MA, Baer L . Use of factor-analyzed symptom dimensions to predict outcome with serotonin reuptake inhibitors and placebo in the treatment of obsessive–compulsive disorder. Am J Psychiatry 1999; 156: 1409–1416.
Summerfeldt LJ, Richter MA, Antony MM, Swinson RP . Symptom structure in obsessive–compulsive disorder: a confirmatory factor-analytic study. Behav Res Ther 1999; 37: 297–311.
Hasler G, Lasalle-Ricci VH, Ronquillo JG, Crawley SA, Cochran LW, Kazuba D et al. Obsessive–compulsive disorder symptom dimensions show specific relationships to psychiatric comorbidity. Psychiatry Res 2005; 135: 121–132.
Mataix-Cols D, Rauch SL, Baer L, Shera D, Eisen J, Goodman WK et al. Symptom stability in adult obsessive–compulsive disorder: data from a two year naturalistic study. Am J Psychiatry 2002; 159: 263–268.
Rufer M, Grothusen A, Mass R, Peter H, Hand I . Temporal stability of symptom dimensions in adult patients with obsessive–compulsive disorder. J Affect Disord 2005; 88: 99–102.
Alsobrook II JP, Leckman JF, Goodman WK, Rasmussen SA, Pauls DL . Segregation analysis of obsessive–compulsive disorder using symptom-based factor scores. Am J Med Genet 1999; 88: 669–675.
Leckman JF, Pauls DL, Zhang H, Rosario-Campos MC, Katsovich L, Kidd K et al. Obsessive–compulsive symptom dimensions in affected sibling pairs diagnosed with Gilles de la Tourette syndrome. Am J Med Genet 2003; 116: 60–68.
Zhang H, Leckman JF, Tsai C-P, Kidd KK, Rosario Campos MC . The Tourette syndrome association international consortium for genetics. Genome wide scan of hoarding in sibling pairs both diagnosed with Gilles de la Tourette syndrome. Am J Hum Genet 2002; 70: 896–904.
Cavallini MC, Di Bella D, Siliprandi F, Malchiodi F, Bellodi L . Exploratory factor-analysis of obsessive–compulsive patients and association with 5-HTTLPR polymorphism. Am J Med Genet 2002; 114: 347–353.
Mataix-Cols D, Cullen S, Lange K, Zelaya F, Andrew C, Amaro E et al. Neural correlates of anxiety associated with obsessive–compulsive symptom dimensions in normal volunteers. Biol Psychiatry 2003; 53: 482–493.
Mataix-Cols D, Wooderson S, Lawrence N, Brammer MJ, Speckens A, Phillips ML . Distinct neural correlates of washing, checking and hoarding symptom dimensions in obsessive–compulsive disorder. Arch Gen Psychiatry 2004; 61: 564–576.
Black DW, Monahan P, Gable J, Blum N, Clancy G, Baker P . Hoarding and treatment response in 38 nondepressed subjects with obsessive–compulsive disorder. J Clin Psychiatry 1998; 59: 420–425.
Alonso P, Menchon JM, Pifarre J, Mataix-Cols D, Torres L, Salgado P et al. Long-term follow-up and predictors of clinical outcome in obsessive–compulsive patients treated with serotonin reuptake inhibitors and behavioral therapy. J Clin Psychiatry 2001; 62: 535–540.
Saxena S, Maidment KM, Vapnik T, Golden G, Rishwain T, Rosen RM et al. Obsessive–compulsive hoarding: symptom severity and response to multimodal treatment. J Clin Psychiatry 2002; 63: 21–27.
Mataix-Cols D, Marks IM, Greist JH, Kobak KA, Baer L . Obsessive–compulsive symptom dimensions as predictors of compliance with and response to behaviour therapy: results from a controlled trial. Psychother Psychosom 2002; 71: 255–262.
Foa EB, Huppert JD, Leiberg S, Langner R, Kichic R, Hajcak G et al. The obsessive–compulsive inventory: development and validation of a short version. Psychol Assess 2002; 14: 485–496.
Thordarson DS, Radomsky AS, Rachman S, Shafran R, Sawchuk CN, Ralph Hakstian A . The Vancouver obsessional compulsive inventory (VOCI). Behav Res Ther 2004; 42: 1289–1314.
Woody SR, Steketee G, Chambless DL . Reliability and validity of the Yale–Brown obsessive–compulsive scale. Behav Res Ther 1995; 33: 597–605.
Deacon BJ, Abramowitz JS . The Yale–Brown obsessive compulsive scale: factor analysis, construct validity, and suggestions for refinement. J Anxiety Disord 2005; 19: 573–585.
Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL et al. The Yale–Brown obsessive–compulsive scale-I-development, use, and reliability. Arch Gen Psychiatry 1989; 46: 1006–1011.
Goodman WK, Price LH, Rasmussen SA, Mazure C, Delgado P, Heninger GR et al. The Yale–Brown obsessive–compulsive scale-II-validity. Arch Gen Psychiatry 1989; 46: 1012–1016.
Pauls D, Hurst CR . Schedule for Tourette's Syndrome and Other Behavioral Syndrome. Yale University: New Haven, CT, 1994.
Foa EB, Kozak MJ . DSM-IV field trial: obsessive–compulsive disorder. Am J Psychiatry 1995; 152: 90–96.
Scahill L, Riddle MA, McSwiggin-Hardin M, Ort SI, King RA, Goodman WK et al. Children's Yale–Brown obsessive–compulsive scale: reliability and validity. J Am Acad Child Adolesc Psychiatry 1997; 36: 844–852.
Leckman JF, Riddle MA, Hardin MT, Ort SI, Swartz KL, Stevenson J et al. The Yale Global Tic Severity Scale: initial testing of a clinician-rated scale of tic severity. J Am Acad Child Adolesc Psychiatry 1989; 28: 566–573.
Poznanski EO, Cook SC, Carroll BJ . A depression rating scale for children. Pediatrics 1979; 64: 442–450.
Hamilton M . A rating scale for depression. J Neurol Neurosurg Psychiatry 1960; 23: 56–62.
Maier W, Buller R, Philipp M, Heuser I . The Hamilton anxiety scale: reliability, validity and sensitivity to change in anxiety and depressive disorders. J Affect Disord 1988; 14: 61–68.
Summerfeldt LJ, Kloosterman PH, Antony MM, Richter MA, Swinson RP . The relationship between miscellaneous symptoms and major symptom factors in obsessive–compulsive disorder. Behav Res Ther 2004; 42: 1453–1467.
McKay D, Abramowitz JS, Calamari JE, Kyrios M, Radomsky A, Sookman D et al. A critical evaluation of obsessive–compulsive disorder subtypes: symptoms versus mechanisms. Clin Psychol Rev 2004; 24: 283–313.
Cooper J . The Leyton obsessional inventory. Psychol Med 1970; 1: 48–64.
Hodgson RJ, Rachman S . Obsessional–compulsive complaints. Behav Res Ther 1977; 15: 389–395.
Insel TR, Murphy DL, Cohen RM, Alterman I, Kilts C, Linnoila M . Obsessive–compulsive disorder: a double-blind trial of clomipramine and clorgyline. Arch Gen Psychiatry 1983; 40: 605–612.
Frost RO, Steketee GS, Krause MS, Trepanier KL . The relationship of the Yale–Brown obsessive–compulsive scale (Y-BOCS) to other measures of obsessive–compulsive symptoms in a nonclinical population. J Personal Assess 1995; 65: 158–168.
Leckman JF, Mayes LC, Feldman R, Evans D, King RA, Cohen DJ . Early parental preoccupations and behaviors and their possible relationship to the symptoms of obsessive–compulsive disorder. Acta Psychiatr Scand 1999; 100: 1–26.
Acknowledgements
This research was funded by NIH grants MH493515, MH61940, RR00044, and RR00125; Fundação de Amparo à Pesquisa do Estado de São Paulo grant 03/07451-6 (MCR-C) and 99/12205-7 (ECM); grants from the Tourette Syndrome Association (MCR-C), the Obsessive–Compulsive Foundation (MCR-C), the Echlin Foundation and the Kaiser Family. The authors thank David Mataix-Cols, PhD, Steven A Rasmussen, MD, David L. Pauls, PhD, and Scott L Rauch, MD for their help in the development of this instrument.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supplementary Information accompanies the paper on Molecular Psychiatry website (http://www.nature.com/mp).
Supplementary information
Rights and permissions
About this article
Cite this article
Rosario-Campos, M., Miguel, E., Quatrano, S. et al. The Dimensional Yale–Brown Obsessive–Compulsive Scale (DY-BOCS): an instrument for assessing obsessive–compulsive symptom dimensions. Mol Psychiatry 11, 495–504 (2006). https://doi.org/10.1038/sj.mp.4001798
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.mp.4001798
Keywords
This article is cited by
-
Autistic, schizotypal traits, and insight level in patients with obsessive–compulsive disorder
Middle East Current Psychiatry (2024)
-
Everyday executive functioning in pediatric obsessive-compulsive disorder: diagnostic specificity, clinical correlations, and outcome
BMC Psychiatry (2023)
-
Obsessions and suicidality in youth suffering from bipolar I disorder
Middle East Current Psychiatry (2023)
-
Symptom Dimension Breakpoints for the Obsessive-Compulsive Inventory-Child Version (OCI-CV)
Child Psychiatry & Human Development (2023)
-
Restricted and Repetitive Behaviors and Interests in Young Children with Autism: A Comparative Study
Indian Journal of Pediatrics (2022)