Abstract
While the monoamine deficiency hypothesis of depression is still most commonly used to explain the actions of antidepressant drugs, a growing body of evidence has accumulated that is not adequately explained by the hypothesis. This article draws attention to contributions from another apparently common pharmacological property of antidepressant medications—the inhibition of nicotinic acetylcholine receptors (nAChR). Evidence is presented suggesting the hypercholinergic neurotransmission, which is associated with depressed mood states, may be mediated through excessive neuronal nicotinic receptor activation and that the therapeutic actions of many antidepressants may be, in part, mediated through inhibition of these receptors. In support of this hypothesis, preliminary evidence is presented suggesting that the potent, centrally acting nAChR antagonist, mecamylamine, which is devoid of monoamine reuptake inhibition, may reduce symptoms of depression and mood instability in patients with comorbid depression and bipolar disorder. If this hypothesis is supported by further preclinical and clinical research, nicotinic acetylcholine receptor antagonists may represent a novel class of therapeutic agents for treating mood disorders.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Schildkraut JJ . The catecholamine hypothesis of affective disorders: a review of supporting evidence, Am J Psychiatry 1965 122: 509–522
Coppen A . The biochemistry of affective disorders Br J Psychiatry 1967 113: 1237–1264
Feighner JP . Mechanism of action of antidepressant medications J Clin Psychiatry 1999 60: 4–11 discussion 12–13
Gittos MW . Toward a better understanding of depression: new mechanistic considerations of antidepressant action provide a basis for development of delay-free drugs Drug Devel Res 2000 51: 1–6
Gjerris A, Sorensen AS, Rafaelsen OJ, Werdelin L, Alling C, Linnoila M . 5-HT and 5-HIAA in cerebrospinal fluid in depression J Affect Disord 1987 12: 13–22
Clerc G, Noury J, Gittos M . Antidepressant effect of a tryptophan hydroxylase activation inhibitor, AGN 2979 Am J Psychiatry 1986 143: 264–265
Mennini T, Mocaer E, Garattini S . Tianeptine, a selective enhancer of serotonin uptake in rat brain Naunyn Schmiedebergs Arch Pharmacol 1987 336: 478–482
Gershon S, Hekimian LJ, Floyd A . Non-correlation of preclinical-clinical evaluation of a prosposed anti-depressant 4-phenyl-bicyclo(2,2,2)octan-1-amine hydrochloride monohydrate (EXP 561) Arzneimittelforschung 1968 18: 243–245
Duman RS, Heninger GR, Nestler EJ . A molecular and cellular theory of depression Arch Gen Psychiatry 1997 54: 597–606
Duman RS, Malberg J, Nakagawa S, D'Sa C . Neuronal plasticity and survival in mood disorders Biol Psychiatry 2000 48: 732–739
Eldefrawi ME, Warnick JE, Schofield GG, Albuquerque EX, Eldefrawi AT . Interaction of imipramine with the ionic channel of the acetylcholine receptor of motor endplate and electric organ Biochem Pharmacol 1981 30: 1391–1394
Arita M, Wada A, Takara H, Izumi F . Inhibition of 22Na influx by tricyclic and tetracyclic antidepressants and binding of [3H]imipramine in bovine adrenal medullary cells J Pharmacol Exp Ther 1987 243: 342–348
Izaguirre V, Fernandez-Fernandez JM, Cena V, Gonzalez-Garcia C . Tricyclic antidepressants block cholinergic nicotinic receptors and ATP secretion in bovine chromaffin cells FEBS Lett 1997 418: 39–42
Schofield GG, Witkop B, Warnick JE, Albuquerque EX . Differentiation of the open and closed states of the ionic channels of nicotinic acetylcholine receptors by tricyclic antidepressants Proc Natl Acad Sci USA 1981 78: 5240–5244
Park TJ, Shin SY, Suh BC, Suh EK, Lee IS, Kim YS, Kim KT . Differential inhibition of catecholamine secretion by amitriptyline through blockage of nicotinic receptors, sodium channels, and calcium channels in bovine adrenal chromaffin cells Synapse 1998 29: 248–256
Rana B, McMorn SO, Reeve HL, Wyatt CN, Vaughan PF, Peers C . Inhibition of neuronal nicotinic acetylcholine receptors by imipramine and desipramine Eur J Pharmacol 1993 250: 247–251
Garcia-Colunga J, Awad JN, Miledi R . Blockage of muscle and neuronal nicotinic acetylcholine receptors by fluoxetine (Prozac) Proc Natl Acad Sci USA 1997 94: 2041–2044
Hennings EC, Kiss JP, Vizi ES . Nicotinic acetylcholine receptor antagonist effect of fluoxetine in rat hippocampal slices Brain Res 1997 759: 292–294
Maggi L, Palma E, Miledi R, Eusebi F . Effects of fluoxetine on wild and mutant neuronal alpha 7 nicotinic receptors Mol Psychiatry 1998 3: 350–355
Fryer JD, Lukas RJ . Antidepressants noncompetitively inhibit nicotinic acetylcholine receptor function J Neurochem 1999 72: 1117–1124
Hennings EC, Kiss JP, De Oliveira K, Toth PT, Vizi ES . Nicotinic acetylcholine receptor antagonistic activity of monoamine uptake blockers in rat hippocampal slices J Neurochem 1999 73: 1043–1050
Kiss JP, Hennings EC, De Oliveira K, Toth PT, Vizi ES . Nicotinic acetylcholine receptor antagonistic activity of the selective dopamine uptake blocker GBR-12909 in rat hippocampal slices J Physiol 2000 526: 69P
Slemmer JE, Martin BR, Damaj MI . Bupropion is a nicotinic antagonist J Pharmacol Exp Ther 2000 295: 321–327
Fryer JD, Lukas RJ . Noncompetitive functional inhibition at diverse, human nicotinic acetylcholine receptor subtypes by bupropion, phencyclidine, and ibogaine J Pharmacol Exp Ther 1999 288: 88–92
Martin BR, Onaivi ES, Martin TJ . What is the nature of mecamylamine's antagonism of the central effects of nicotine? Biochem Pharmacol 1989 38: 3391–3397
Rose JE, Behm FM, Westman EC . Nicotine-mecamylamine treatment for smoking cessation: the role of pre- cessation therapy Exp Clin Psychopharmacol 1998 6: 331–343
Hurt RD, Sachs DP, Glover ED, Offord KP, Johnston JA, Dale LC et al. A comparison of sustained-release bupropion and placebo for smoking cessation N Engl J Med 1997 337: 1195–1202
Mitchell AJ . The role of corticotropin releasing factor in depressive illness: a critical review Neurosci Biobehav Rev 1998 22: 635–651
Nemeroff CB . The neurobiology of depression Sci Am 1998 278: 42–49
Gilad GM . The stress-induced response of the septo-hippocampal cholinergic system. A vectorial outcome of psychoneuroendocrinological interactions Psychoneuroendocrinology 1987 12: 167–184
Janowsky DS, Risch SC . Cholinomimetic and anticholinergic drugs used to investigate and acetylcholine hypothesis of affective disorders and stress Drug Devel Res 1984 4: 125–142
Janowsky DS, el-Yousef MK, Davis JM, Sekerke HJ . A cholinergic-adrenergic hypothesis of mania and depression Lancet 1972 2: 632–635
Janowsky DS, Overstreet DH, Nurnberger JI Jr . Is cholinergic sensitivity a genetic marker for the affective disorders? Am J Med Genet 1994 54: 335–344
Janowsky D, El-Yousef MK, Davis JM . Acetylcholine and depression Psychosom Med 1974 36: 248–257
Nurnberger JI Jr, Jimerson DC, Simmons-Alling S, Tamminga C, Nadi NS, Lawrence D et al. Behavioral, physiological, and neuroendocrine responses to arecoline in normal twins and bipolar patients Psychiatry Res 1983 9: 191–200
Risch SC, Kalin NH, Murphy DL . Pharmacological challenge strategies: implications for neurochemical mechanisms in affective disorders and treatment approaches J Clin Psychopharmacol 1981 1: 238–243
Oppenheimer G, Ebstein RP, Belmaker RH . Effect of lithium on the physostigmine-induced behavioral syndrome and plasma cyclic GMP J Psychiatr Res 1979 15: 133–138
Janowsky DS, Overstreet DH, Nurnberger JI Jr . Is cholinergic sensitivity a genetic marker for the affective disorders? Am J Med Genet 1994 54: 335–344
Charles HC, Lazeyras F, Krishnan KR, Boyko OB, Payne M, Moore D . Brain choline in depression: in vivo detection of potential pharmacodynamic effects of antidepressant therapy using hydrogen localized spectroscopy Prog Neuropsychopharmacol Biol Psychiatry 1994 18: 1121–1127
Steingard RJ, Yurgelun-Todd DA, Hennen J, Moore JC, Moore CM, Vakili K et al. Increased orbitofrontal cortex levels of choline in depressed adolescents as detected by in vivo proton magnetic resonance spectroscopy Biol Psychiatry 2000 48: 1053–1061
Kile JP, Turner BB . Serotonergic and cholinergic interaction in the regulation of pituitary-adrenal function in rats Experientia 1985 41: 1123–1127
Rhodes ME, O'Toole SM, Wright SL, Czambel RK, Rubin RT . Sexual diergism in rat hypothalamic-pituitary-adrenal axis responses to cholinergic stimulation and antagonism Brain Res Bull 2001 54: 101–113
Parrott AC . Stress modulation over the day in cigarette smokers Addiction 1995 90: 233–244
Glassman AH, Helzer JE, Cove LS, Cottler LB, Stetner F, Tipp JE et al. Smoking, smoking cessation, and major depression Jama 1990 264: 1546–1549
Bergen AW, Caporaso N . Cigarette smoking J Natl Cancer Inst 1999 91: 1365–1375
Anda RF, Williamson DF, Escobedo LG, Mast EE, Giovino GA, Remington PL . Depression and the dynamics of smoking. A national perspective Jama 1990 264: 1541–1545
Covey LS, Glassman AH, Stetner F . Cigarette smoking and major depression J Addict Dis 1998 17: 35–46
Covey LS, Glassman AH, Stetner F . Major depression following smoking cessation Am J Psychiatry 1997 154: 263–265
Labbate LA . Nicotine cessation, mania, and depression [letter] [published erratum appears in Am J Psychiatry 1992 Sep; 149(9): 1287] Am J Psychiatry 1992 149: 708
Salin-Pascual RJ, Rosas M, Jimenez-Genchi A, Rivera-Meza BL, Delgado-Parra V . Antidepressant effect of transdermal nicotine patches in nonsmoking patients with major depression J Clin Psychiatry 1996 57: 387–389
Tizabi Y, Overstreet DH, Rezvani AH, Louis VA, Clark E Jr, Janowsky DS et al. Antidepressant effects of nicotine in an animal model of depression Psychopharmacol (Berl) 1999 142: 193–199
Semba J, Mataki C, Yamada S, Nankai M, Toru M . Antidepressantlike effects of chronic nicotine on learned helplessness paradigm in rats Biol Psychiatry 1998 43: 389–391
Ferguson SM, Brodkin JD, Lloyd GK, Menzaghi F . Antidepressant-like effects of the subtype-selective nicotinic acetylcholine receptor agonist, SIB-1508Y, in the learned helplessness rat model of depression Psychopharmacol (Berl) 2000 152: 295–303
Tizabi Y, Rezvani AH, Russell LT, Tyler KY, Overstreet DH . Depressive characteristics of FSL rats: involvement of central nicotinic receptors Pharmacol Biochem Behav 2000 66: 73–77
Caldarone BJ, Picciotto MR . Role of high affinity nicotinic receptors in learned helplessness behavior Soc Neurosci 1999 Miami, FL
Wang MQ, Fitzhugh EC, Green BL, Turner LW, Eddy JM, Westerfield RC . Prospective social-psychological factors of adolescent smoking progression J Adolesc Health 1999 24: 2–9
Patton GC, Hibbert M, Rosier MJ, Carlin JB, Caust J, Bowes G . Is smoking associated with depression and anxiety in teenagers? Am J Public Health 1996 86: 225–230
Patton GC, Carlin JB, Coffey C, Wolfe R, Hibbert M, Bowes G . Depression, anxiety, and smoking initiation: a prospective study over 3 years Am J Public Health 1998 88: 1518–1522
Goodman E, Capitman J . Depressive symptoms and cigarette smoking among teens Pediatrics 2000 106: 748–755
Breslau N, Klein DF . Smoking and panic attacks: an epidemiologic investigation Arch Gen Psychiatry 1999 56: 1141–1147
Brown RA, Lewinsohn PM, Seeley JR, Wagner EF . Cigarette smoking, major depression, and other psychiatric disorders among adolescents J Am Acad Child Adolesc Psychiatry 1996 35: 1602–1610
Kendler KS, Neale MC, MacLean CJ, Heath AC, Eaves LJ, Kessler RC . Smoking and major depression. A causal analysis Arch Gen Psychiatry 1993 50: 36–43
Perkins KA . Baseline-dependency of nicotine effects: a review Behav Pharmacol 1999 10: 597–615
Dani JA . Overview of nicotinic receptors and their roles in the central nervous system Biol Psychiatry 2001 49: 166–174
Lukas RJ . Neuronal nicotinic aceytlcholine receptors. The Nicotinic Acetylcholine Receptor: Current Views and Future Trends Springer-Verlag, Berlin and RG Landes Co 1998
Colquhoun LM, Patrick JW . Pharmacology of neuronal nicotinic acetylcholine receptor subtypes Adv Pharmacol 1997 39: 191–220
Lukas RJ et al. International Union of Pharmacology. XX. Current status of the nomenclature for nicotinic acetylcholine receptors and their subunits Pharmacol Rev 1999 51: 397–401
Conroy WG, Berg DK . Neurons can maintain multiple classes of nicotinic acetylcholine receptors distinguished by different subunit compositions J Biol Chem 1995 270: 4424–4431
Vizi ES, Lendvai B . Modulatory role of presynaptic nicotinic receptors in synaptic and non-synaptic chemical communication in the central nervous system Brain Res Brain Res Rev 1999 30: 219–235
Picciotto MR, Caldarone BJ, King SL, Zachariou V . Nicotinic receptors in the brain. Links between molecular biology and behavior Neuropsychopharmacology 2000 22: 451–465
Lukas RJ, Ke L, Bencherif M, Eisenhour CM . Regulation by nicotine of its own receptors Drug Devel Res 1996 38: 136–148
Hsu YN, Amin J, Weiss DS, Wecker L . Sustained nicotine exposure differentially affects alpha 3 beta 2 and alpha 4 beta 2 neuronal nicotinic receptors expressed in Xenopus oocytes J Neurochem 1996 66: 667–675
Benowitz NL . Pharmacokinetic considerations in understanding nicotine dependence Ciba Found Symp 1990 152: 186–200 discussion 200–209
Dani JA, Radcliffe KA, Pidoplichko VI . Variations in desensitization of nicotinic acetylcholine receptors from hippocampus and midbrain dopamine areas Eur J Pharmacol 2000 393: 31–38
Benwell ME, Balfour DJ, Birrell CE . Desensitization of the nicotine-induced mesolimbic dopamine responses during constant infusion with nicotine Br J Pharmacol 1995 114: 454–460
Hulihan-Giblin BA, Lumpkin MD, Kellar KJ . Effects of chronic administraion of nicotine on prolactin release in the rat: inactivation of prolactin response by repeated injections of nicotine J Pharmacol Exp Therapeut 1989 252: 21–25
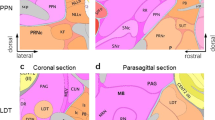
Wada E, Wada K, Boulter J, Deneris E, Heinemann S, Patrick J et al. Distribution of alpha 2, alpha 3, alpha 4, and beta 2 neuronal nicotinic receptor subunit mRNAs in the central nervous system: a hybridization histochemical study in the rat J Comp Neurol 1989 284: 314–335
Clarke PB, Schwartz RD, Paul SM, Pert CB, Pert A . Nicotinic binding in rat brain: autoradiographic comparison of [3H]acetylcholine, [3H]nicotine, and [125I]-alpha-bungarotoxin J Neurosci 1985 5: 1307–1315
Mulle C, Vidal C, Benoit P, Changeux JP . Existence of different subtypes of nicotinic acetylcholine receptors in the rat habenulo-interpeduncular system J Neurosci 1991 11: 2588–2597
Quick MW, Ceballos RM, Kasten M, McIntosh JM, Lester RA . Alpha3beta4 subunit-containing nicotinic receptors dominate function in rat medial habenula neurons Neuropharmacology 1999 38: 769–783
Albuquerque EX, Alkondon M, Pereira EF, Castro NG, Schrattenholz A, Barbosa CT et al. Properties of neuronal nicotinic acetylcholine receptors: pharmacological characterization and modulation of synaptic function J Pharmacol Exp Ther 1997 280: 1117–1136
Albuquerque EX, Pereira EF, Alkondon M, Schrattenholz A, Maelicke A . Nicotinic acetylcholine receptors on hippocampal neurons: distribution on the neuronal surface and modulation of receptor activity J Recept Signal Transduct Res 1997 17: 243–266
Raber J, Koob GF, Bloom FE . Interleukin-2 (IL-2) induces corticotropin-releasing factor (CRF) release from the amygdala and involves a nitric oxide-mediated signaling; comparison with the hypothalamic response J Pharmacol Exp Ther 1995 272: 815–824
Okuda H, Shioda S, Nakai Y, Nakayama H, Okamoto M, Nakashima T . The presence of corticotropin-releasing factor-like immunoreactive synaptic vesicles in axon terminals with nicotinic acetylcholine receptor-like immunoreactivity in the median eminence of the rat Neurosci Lett 1993 161: 183–186
Takada Y, Ihara H, Urano T, Takada A . Changes in blood and plasma serotonergic measurements in rats—effect of nicotine and/or exposure to different stresses Thromb Res 1995 80: 307–316
Sithichoke N, Marotta SF . Cholinergic influences on hypothalamic-pituitary-adrenocortical activity of stressed rats: an approach utilizing agonists and antagonists Acta Endocrinol (Copenh) 1978 89: 726–736
Newman MB, Nazian S, Sanberg PR, Diamond D, Shytle RD . Corticosterone-attenutating and anxiolytic properties of mecamylamine in the rat Neuro-Psychopharmacol Biol Psychiatry 2001 25: 609–620
Houdi AA, Dowell RT, Diana JN . Cardiovascular responses to cigarette smoke exposure in restrained conscious rats J Pharmacol Exp Ther 1995 275: 646–653
Kubo T, Katsumata Y . Fukumori R, Taguchi K, Hagiwara Y. Central nicotinic receptor blockade inhibits emotionally conditioned pressor responses in rats Experientia 1996 52: 348–352
Corrigall WA, Coen KM . Selective dopamine antagonists reduce nicotine self-administration Psychopharmacology 1991 104: 171–176
Corrigall WA, Franklin KB, Coen KM, Clarke PB . The mesolimbic dopaminergic system is implicated in the reinforcing effects of nicotine Psychopharmacology 1992 107: 285–289
Clarke PB, Fu DS, Jakubovic A, Fibiger HC . Evidence that mesolimbic dopaminergic activation underlies the locomotor stimulant action of nicotine in rats J Pharmacol Exp Ther 1988 246: 701–708
Pidoplichko VI, DeBiasi M, Williams JT, Dani JA . Nicotine activates and desensitizes midbrain dopamine neurons Nature 1997 390: 401–404
Leibenluft E, Albert PS, Rosenthal NE, Wehr TA . Relationship between sleep and mood in patients with rapid-cycling bipolar disorder Psychiatry Res 1996 63: 161–168
O'Hara BF, Edgar DM, Cao VH, Wiler SW, Heller HC, Kilduff TS et al. Nicotine and nicotinic receptors in the circadian system Psychoneuroendocrinology 1998 23: 161–173
O'Hara BF, Macdonald E, Clegg D, Wiler SW, Andretic R, Cao VH et al. Developmental changes in nicotinic receptor mRNAs and responses to nicotine in the suprachiasmatic nucleus and other brain regions Brain Res Mol Brain Res 1999 66: 71–82
Cirelli C, Tononi G . Gene expression in the brain across the sleep-waking cycle Brain Res 2000 885: 303–321
Keefe DL, Earnest DJ, Nelson D, Takahashi JS, Turek FW . A cholinergic antagonist, mecamylamine, blocks the phase-shifting effects of light on the circadian rhythm of locomotor activity in the golden hamster Brain Res 1987 403: 308–312
Zhang Y, Zee PC, Kirby JD, Takahashi JS, Turek FW . A cholinergic antagonist, mecamylamine, blocks light-induced fos immunoreactivity in specific regions of the hamster suprachiasmatic nucleus Brain Res 1993 615: 107–112
Patten CA, Choi WS, Gillin JC, Pierce JP . Depressive symptoms and cigarette smoking predict development and persistence of sleep problems in US adolescents Pediatrics 2000 106: E23
Wetter DW, Carmack CL, Anderson CB, Moore CA, De Moor CA, Cinciripini PM et al. Tobacco withdrawal signs and symptoms among women with and without a history of depression Exp Clin Psychopharmacol 2000 8: 88–96
Shytle RD, Silver AA, Sanberg PR . Comorbid bipolar disorder in tourette syndrome responds to nicotinic receptor antagonist, mecamylamine (Inversine® Biol Psychiatry 2000 48: 1028–1031
Shytle RD, Silver AA, Sheehan KH, Sheehan DV, Sanberg PR . Neuronal nicotinic receptor inhibition for treating mood disorders: preliminary controlled evidence with mecamylamine Depression and Anxiety 2001 (in press)
Shytle RD, Silver AA, Wilkinson BJ, Newman MB, Katherine-Philip M, Sanberg PR et al. Treatment of Tourette disorder with transdermal nicotine and haloperidol. In: IBC's 2nd International Symposium on Nicotinic Acetylcholine Receptors, Advances in Molecular Pharmacology and Drug Development Annapolis, MD 1999
Shytle RD, Silver AA, Philipp MK, McConville BJ, Sanberg PR . Transdermal nicotine for tourette's syndrome Drug Devel Res 1996 38: 290–298
Sanberg PR, Shytle RD, Silver AA . Treatment of Tourette's syndrome with mecamylamine [letter] Lancet 1998 352: 705–706
Young JM, Shytle RD, Sanberg PR, George TP . Mecamylamine: new therapeutic uses and toxicity/risk profile Clin Ther 2001 23: 532–565
Reid MS, Mickalian JD, Delucchi KL, Berger SP . A nicotine antagonist, mecamylamine, reduces cue-induced cocaine craving in cocaine-dependent subjects Neuropsychopharmacology 1999 20: 297–307
Blomqvist O, Ericson M, Engel JA, Soderpalm B . Accumbal dopamine overflow after ethanol: localization of the antagonizing effect of mecamylamine Eur J Pharmacol 1997 334: 149–156
Silver AA, Shytle RD, Sheehan KH, Sheehan DV, Ramos A, Sanberg PR . Multi-center double blind placebo controlled study of mecamylamine monotherapy for Tourette's disorder J Am Acad Child Adolesc Psychiatry 2001 40: 1103–1110
Prochazka AV, Weaver MJ, Keller RT, Fryer GE, Licari PA, Lofaso D . A randomized trial of nortriptyline for smoking cessation Arch Intern Med 1998 158: 2035–2039
Hughes JR, Stead LF, Lancaster T . Antidepressants for smoking cessation (Cochrane Review) Cochrane Database Syst Rev 2000 4: CD000031
Dalack GW, Glassman AH, Rivelli S, Covey L, Stetner F . Mood, major depression, and fluoxetine response in cigarette smokers Am J Psychiatry 1995 152: 398–403
Perkins KA . Individual variability in responses to nicotine Behav Genet 1995 25: 119–132
Compton MT, Nemeroff CB . The treatment of bipolar depression J Clin Psychiatry 2000 61: 57–67
Thase ME, Sachs GS . Bipolar depression: pharmacotherapy and related therapeutic strategies Biol Psychiatry 2000 48: 558–572
Picard F, Bertrand S, Steinlein OK, Bertrand D . Mutated nicotinic receptors responsible for autosomal dominant nocturnal frontal lobe epilepsy are more sensitive to carbamazepine Epilepsia 1999 40: 1198–1209
Donnelly-Roberts DL, Arneric SP, Sullivan JP . Functional modulation of human “ganglionic-like” neuronal nicotinic acetylcholine receptors (nAChRs) by L-type calcium channel antagonists Biochem Biophys Res Commun 1995 213: 657–662
Malberg JE, Eisch AJ, Nestler EJ, Duman RS . Chronic antidepressant treatment increases neurogenesis in adult rat hippocampus J Neurosci 2000 20: 9104–9110
Belluardo N, Mudo G, Blum M, Fuxe K . Central nicotinic receptors, neurotrophic factors and neuroprotection Behav Brain Res 2000 113: 21–34
James JR, Nordberg A . Genetic and environmental aspects of the role of nicotinic receptors in neurodegenerative disorders: emphasis on Alzheimer's disease and Parkinson's disease Behav Genet 1995 25: 149–159
Ryan RE, Ross SA, Drago J, Loiacono RE . Dose-related neuroprotective effects of chronic nicotine in 6-hydroxydopamine treated rats, and loss of neuroprotection in alpha4 nicotinic receptor subunit knockout mice Br J Pharmacol 2001 132: 1650–1656
Prendergast MA, Harris BR, Mayer S, Holley RC, Hauser KF, Littleton JM . Chronic nicotine exposure reduces N-methyl-D-aspartate receptor-mediated damage in the hippocampus without altering calcium accumulation or extrusion: evidence of calbindin-D28K overexpression Neuroscience 2001 102: 75–85
Zoli M, Picciotto MR, Ferrari R, Cocchi D, Changeux JP . Increased neurodegeneration during ageing in mice lacking high-affinity nicotine receptors Embo J 1999 18: 1235–1244
O'Neill AB, Morgan SJ, Brioni JD . Histological and behavioral protection by (−)-nicotine against quinolinic acid-induced neurodegeneration in the hippocampus Neurobiol Learn Mem 1998 69: 46–64
Kihara T, Shimohama S, Sawada H, Kimura J, Kume T, Kochiyama H, Maeda T . Akaike A. Nicotinic receptor stimulation protects neurons against beta-amyloid toxicity Ann Neurol 1997 42: 159–163
Shimohama S, Akaike A, Kimura J . Nicotine-induced protection against glutamate cytotoxicity. Nicotinic cholinergic receptor-mediated inhibition of nitric oxide formation Ann NY Acad Sci 1996 777: 356–361
Akaike A, Tamura Y, Yokota T, Shimohama S, Kimura J . Nicotine-induced protection of cultured cortical neurons against N-methyl-D-aspartate receptor-mediated glutamate cytotoxicity Brain Res 1994 644: 181–187
Li Y, Papke RL, He YJ, Millard WJ, Meyer EM . Characterization of the neuroprotective and toxic effects of alpha7 nicotinic receptor activation in PC12 cells Brain Res 1999 830: 218–225
Papke RL, Meyer E, Nutter T, Uteshev VV . alpha7 Receptor-selective agonists and modes of alpha7 receptor activation Eur J Pharmacol 2000 393: 179–195
Papke RL, Thinschmidt JS, Moulton BA, Meyer EM, Poirier A . Activation and inhibition of rat neuronal nicotinic receptors by ABT- 418 Br J Pharmacol 1997 120: 429–438
Briggs CA et al. Functional characterization of the novel neuronal nicotinic acetylcholine receptor ligand GTS-21 in vitro and in vivo Pharmacol Biochem Behav 1997 57: 231–241
Briggs CA, McKenna DG . Activation and inhibition of the human alpha7 nicotinic acetylcholine receptor by agonists Neuropharmacology 1998 37: 1095–1102
Papke RL, Sanberg PR, Shytle RD . Analysis of mecamylamine stereoisomers on human nicotinic receptor subtypes J Pharmacol Exp Ther 2001 297: 646–656
Dwoskin LP, Wilkins LH, Pauly JR, Crooks PA . Development of a novel class of subtype-selective nicotinic receptor antagonist: pyridine-N-substituted nicotine analogs Ann NY Acad Sci 1999 868: 617–619
Giniatullin RA, Sokolova EM, Di Angelantonio S, Skorinkin A, Talantova MV, Nistri A . Rapid relief of block by mecamylamine of neuronal nicotinic acetylcholine receptors of rat chromaffin cells in vitro: an electrophysiological and modeling study Mol Pharmacol 2000 58: 778–787
Lukas RJ . Pharmacological distinctions between functional nicotinic acetylcholine receptors on the PC12 rat pheochromocytoma and the TE671 human medulloblastoma J Pharmacol Exp Ther 1989 251: 175–182
Lukas RJ . Expression of ganglia-type nicotinic acetylcholine receptors and nicotinic ligand binding sites by cells of the IMR-32 human neuroblastoma clonal line J Pharmacol Exp Ther 1993 265: 294–302
Gatto GJ, Letchworth SR, Bencherif M . Antidepressant-like effects of a sub-type selective neuronal nicotinic receptor ligand, TC-1707, in the Forced Swim Test Soc Neurosci Abs 2001 27: 488.10
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shytle, R., Silver, A., Lukas, R. et al. Nicotinic acetylcholine receptors as targets for antidepressants. Mol Psychiatry 7, 525–535 (2002). https://doi.org/10.1038/sj.mp.4001035
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.mp.4001035
Keywords
This article is cited by
-
Associations of Acetylcholinesterase Inhibition Between Pesticide Spray Seasons with Depression and Anxiety Symptoms in Adolescents, and the Role of Sex and Adrenal Hormones on Gender Moderation
Exposure and Health (2021)
-
Cholinergic regulation of mood: from basic and clinical studies to emerging therapeutics
Molecular Psychiatry (2019)
-
Molecular basis of atypicality of bupropion inferred from its receptor engagement in nervous system tissues
Psychopharmacology (2018)
-
Down-regulation of cholinergic signaling in the habenula induces anhedonia-like behavior
Scientific Reports (2017)
-
Methylene blue and its analogues as antidepressant compounds
Metabolic Brain Disease (2017)