Abstract
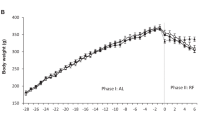
Semi-starvation induced hyperactivity (SIH) occurs in rodents upon caloric restriction. We hypothesized that SIH is triggered by the decline in leptin secretion associated with food restriction. To test this hypothesis, rats, which had established a stable level of activity, were treated with leptin or vehicle via implanted minipumps concomitantly to initiation of food restriction for 7 days. In a second experiment treatment was initiated after SIH had already set in. In contrast to the vehicle-treated rats, which increased their baseline activity level by 300%, the development of SIH was suppressed by leptin. Furthermore, leptin was able to stop SIH, after it had set in. These results underscore the assumed major role of leptin in the adaptation to semi-starvation. Because SIH has been viewed as a model for anorexia nervosa, we also assessed subjective ratings of motor restlessness in 30 patients with this eating disorder in the emaciated state associated with hypoleptinemia and after increments in leptin secretion brought upon by therapeutically induced weight gain. Hypoleptinemic patients ranked their motor restlessness higher than upon attainment of their maximal leptin level during inpatient treatment. Thus, hypoleptinemia might also contribute to the hyperactivity frequently associated with anorexia nervosa.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Beumont PJ, Arthur B, Russell JD, Touyz SW . Excessive physical activity in dieting disorder patients: proposals for a supervised exercise program Int J Eat Disord 1994; 15: 21–36
Davis C . Eating disorders and hyperactivity: a psychobiological perspective Can J Psychiatry 1997; 42: 168–175
Casper RC . Behavioral activation and lack of concern, core symptoms of anorexia nervosa? Int J Eat Disord 1998; 24: 381–393
Bergh C, Sodersten P . Anorexia nervosa, self-starvation and the reward of stress Nat Med 1996; 2: 21–22
Russell JC, Epling WF, Pierce D, Amy RM, Boer DP . Induction of voluntary prolonged running by rats J Appl Physiol 1987; 63: 2549–2553
Morse AD, Russell JC, Hunt TW, Wood GO, Epling WF, Pierce WD . Diurnal variation of intensive running in food-deprived rats Can J Physiol Pharmacol 1995; 73: 1519–1523
Ahima RS, Prabakaran D, Mantzoros C, Qu D, Lowell B, Maratos-Flier E et al. Role of leptin in the neuroendocrine response to fasting Nature 1996; 382: 250–252
Kolaczynski JW, Considine RV, Ohannesian J, Marco C, Opentanova I, Nyce MR et al. Responses of leptin to short-term fasting and refeeding in humans: a link with ketogenesis but not ketones themselves Diabetes 1996; 45: 1511–1515
Heiman ML, Ahima RS, Craft LS, Schoner B, Stephens TW, Flier JS . Leptin inhibition of the hypothalamic-pituitary-adrenal axis in response to stress Endocrinology 1997; 138: 3859–3863
Halaas JL, Gajiwala KS, Maffei M, Cohen SL, Chait BT, Rabinowitz D et al. Weight-reducing effects of the plasma protein encoded by the obese gene Science 1995; 269: 543–546
Klingenspor M, Niggemann H, Heldmaier G . Modulation of leptin sensitivity by short photoperiod acclimation in the Djungarian hamster Phodopus sungorus 2000; J Comp Physiol [B] 170: 37–43
Scarpace PJ, Matheny M, Pollock BH, Tumer N . Leptin increases uncoupling protein expression and energy expenditure Am J Physiol 1997; 273: E226–E230
Döring H, Schwarzer K, Nuesslein-Hildesheim B, Schmidt I . Leptin selectively increases energy expenditure of food-restricted lean mice Int J Obes Relat Metab Disord 1998; 22: 83–88
Zachwieja JJ, Hendry SL, Smith SR, Harris RB . Voluntary wheel running decreases adipose tissue mass and expression of leptin mRNA in Osborne–Mendel rats Diabetes 1997; 46: 1159–1166
Lewis DE, Shellard L, Koeslag DG, Boer DE, McCarthy HD, McKibbin PE et al. Intense exercise and food restriction cause similar hypothalamic neuropeptide Y increases in rats Am J Physiol 1993; 264: E279–E284
Fulton S, Woodside B, Shizgal P . Modulation of brain reward circuitry by leptin Science 2000; 287: 125–128
Ahima RS, Kelly J, Elmquist JK, Flier JS . Distinct physiologic and neuronal responses to decreased leptin and mild hyperleptinemia Endocrinology 1999; 140: 4923–4931
Huang Q, Rivest R, Richard D . Effects of leptin on corticotropin-releasing factor (CRF) synthesis and CRF neuron activation in the paraventricular hypothalamic nucleus of obese (ob/ob) mice Endocrinology 1998; 139: 1524–1532
Blum WF, Englaro P, Hanitsch S, Juul A, Hertel NT, Muller J et al. Plasma leptin levels in healthy children and adolescents: dependence on body mass index, body fat mass, gender, pubertal stage, and testosterone J Clin Endocrinol Metab 1997; 82: 2904–2910
Pirke KM, Broocks A, Wilckens T, Marquard R, Schweiger U . Starvation-induced hyperactivity in the rat: the role of endocrine and neurotransmitter changes Neurosci Biobehav Rev 1993; 17: 287–294
Ballauff A, Ziegler A, Emons G, Sturm G, Blum WF, Remschmidt H et al. Serum leptin and gonadotropin levels in patients with anorexia nervosa during weight gain Mol Psychiatry 1999; 4: 71–75
Hebebrand J, van der Heyden J, Devos R, Kopp W, Herpertz S, Remschmidt H et al. Plasma concentrations of obese protein in anorexia nervosa Lancet 1995; 346: 1624–1625
Hebebrand J, Blum WF, Barth N, Coners H, Englaro P, Juul A et al. Leptin levels in patients with anorexia nervosa are reduced in the acute stage and elevated upon short-term weight restoration Mol Psychiatry 1997; 2: 330–334
Köpp W, Blum WF, von Prittwitz S, Ziegler A, Lubbert H, Emons G et al. Low leptin levels predict amenorrhea in underweight and eating disordered females Mol Psychiatry 1997; 2: 335–340
Acknowledgements
We thank Franziska Wollnik (Universität Stuttgart, Germany) for generous provision of the running wheels. We thank Tilman Görg for his technical assistance. These studies were supported by the Deutsche Forschungsgemeinschaft.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Exner, C., Hebebrand, J., Remschmidt, H. et al. Leptin suppresses semi-starvation induced hyperactivity in rats: implications for anorexia nervosa. Mol Psychiatry 5, 476–481 (2000). https://doi.org/10.1038/sj.mp.4000771
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.mp.4000771
Keywords
This article is cited by
-
Low leptin levels are associated with elevated physical activity among lean school children in rural Tanzania
BMC Public Health (2022)
-
Blocking ActRIIB and restoring appetite reverses cachexia and improves survival in mice with lung cancer
Nature Communications (2022)
-
Activity-based anorexia animal model: a review of the main neurobiological findings
Journal of Eating Disorders (2021)
-
Joining forces: the need to combine science and ethics to address problems of validity and translation in neuropsychiatry research using animal models
Philosophy, Ethics, and Humanities in Medicine (2020)
-
Short-term metreleptin treatment of patients with anorexia nervosa: rapid on-set of beneficial cognitive, emotional, and behavioral effects
Translational Psychiatry (2020)