Abstract
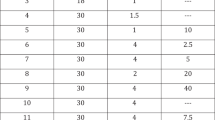
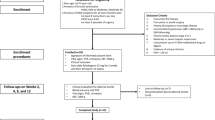
We evaluate the efficacy and safety of tamsulosin a selective α1A-receptor antagonist in patients with painful ejaculation (PE) as a sole entity. A total of 118 men with PE were included in the study. Patients were randomly assigned to receive 0.4 mg oral daily tamsulosin (group 1, n=59) or placebo (group 2, n=59), during a 6-week period for each agent. Pretreatment evaluation included history and physical examination, International Index of Erectile Function (IIEF) and a visual analog scale (VAS) for pain. The efficacy of two treatments was assessed every 2 weeks during treatment, and at the end of the study using responses to IIEF, VAS evaluation, mean intercourse satisfaction domain, mean weekly coitus episodes and adverse drug effects. In all, 104 patients (88%) completed the whole treatment schedule. Pain resolved in 16 and 13% of the patients treated with tamsulosin and placebo, respectively (P=0.1). Baseline mean intercourse satisfaction domain values of IIEF 10 and 11 reached to 12 and 10 at 6-week treatment in groups 1 and 2, respectively (P=0.08). The VAS after tamsulosin and placebo decreased from 5.7 and 5.8 to 5.1 and 5.5, respectively (P=0.1). The mean weekly intercourse episodes increased from pretreatment values of 1.8 and 1.6 to 1.9 and 1.7, for tamsulosin and placebo, respectively (P=0.08). Mean number of adverse events was 11 for tamsulosin and 5 for placebo (P<0.05). Tamsulosin is no better than placebo in improvement of PE as a sole entity.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Blanker MH, Bosch JL, Groewneveld FP, Bohnen AM, Prins A, Thomas S et al. Erectile and ejaculatory dysfunction in a community-based sample of men 50–78 years old: prevalence, concern, and relation to sexual activity. Urology 2001; 57: 763–768.
Rosen R, Altwein J, Boyle P, Kirby RS, Lukacs B, Meuleman E et al. Lower urinary tract symptoms and male sexual dysfunction: the multinational survey of the aging male (MSAM-7). Eur Urol 2003; 44: 637–649.
Vallancien G, Emberton M, Harving N, van Moorselaar RJ . Sexual dysfunction in 1274 European men suffering from lower urinary tract symptoms. J Urol 2003; 169: 2257–2261.
Koeman M, van Driel MF, Schultz WC, Mensink HJ . Orgasm after radical prostatectomy. Br J Urol 1996; 77: 861–864.
Goriunov VG, Davidov MI . Sexual readaptation after the surgical treatment of benign prostatic hyperplasia. Urol Nefrol Mosk 1997; 5: 20–24.
Luzzi G . Male genital pain disorders. Sexual Relationship Ther 2003; 18: 225–235.
Francisca EA, d'Ancona FC, Meuleman EJ, Debruyne FM, de la Rosette JJ . Sexual function following high energy microwave thermotherapy: results of a randomized controlled study comparing transurethral microwave thermotherapy to transurethral prostatic resection. J Urol 1999; 161: 486–490.
Merrick GS, Wallner K, Butler WM, Lief JH, Sutlief S . Short-term sexual function after prostate brachytherapy. Int J Cancer 2001; 96: 313–319.
Frankel SJ, Donovan JL, Peters TI, Abrams P, Dabhoiwala NF, Osawa D et al. Sexual dysfunction in men with lower urinary tract symptoms. J Clin Epidemiol 1998; 51: 677–685.
Brookes ST, Donovan JL, Peters TJ, Abrams P, Neal DE . Sexual dysfunction in men after treatment for lower urinary tract symptoms: evidence from randomized control trial. BMJ 2002; 324: 1059–1061.
Nickel JC, Narayan P, McKay J, Doyle C . Treatment of chronic prostatitis/chronic pelvic pain syndrome with tamsulosin: a randomized double blind trial. J Urol 2004; 171: 1594–1597.
Simpson GM, Blair JH, Amuso D . Effects of antidepressants on genito-urinary function. J Nerv Syst 1965; 26: 787–789.
Hucker HB, Stauffer SC, Clayton FG, Nakra BRS, Gaind R . Plasma levels of a new pelletized form of amitriptyline for maintenance therapy. J Clin Psychopharmacol 1975; 15: 168–172.
Kulik FA, Wilbur R . Case report of painful ejaculation as a side effect of amoxapine. Am J Psychiatry 1982; 139: 234–235.
Monteiro WO, Noshirvani HF, Marks IM, Lelliott PT . Anorgasmia from clomipramine in obsessive-compulsive disorder. A controlled trial. Br J Psychiatry 1987; 151: 107–112.
Aizenberg D, Zemishlany Z, Hermesh H, Karp L, Weizman A . Painful ejaculation associated with antidepressants in four patients. J Clin Psychiatry 1991; 52: 461–463.
Hsu JH, Shen WW . Male sexual side effects associated with antidepressants: a descriptive clinical study of 32 patients. Int J Psychiatry Med 1995; 25: 191–201.
Michael A . Venlafaxine induced painful ejaculation. Br J Psychiatry 2000; 177: 282–283.
Pulito VL, Li X, Varga SS, Mulcahy LS, Clark KS, Halbert SA et al. An investigation of the uroselective properties of four novel alpha (1a)-adrenergic receptor subtype-selective antagonists. J Pharmacol Exp Ther 2000; 294: 224–229.
Dunn CJ, Matheson A, Faulds DM . Tamsulosin: a review of its pharmacology and therapeutic efficacy in the management of lower urinary tract symptoms. Drugs Aging 2002; 19 (2): 135–161.
Kenny B, Ballard S, Blagg J, Fox D . Pharmacological options in the treatment of benign prostatic hyperplasia. J Med Chem 1997; 40: 1293–1315.
Ford APDW, Daniels DV, Chang DJ, Gever JR, Jasper JR, Lesnick JD et al. Pharmacological pleiotropism of the human recombinant α1A-adrenoceptor: implications for α1A-adrenoceptor classification. Br J Pharmacol 1997; 121: 1127–1135.
Price DT, Schwinn DA, Lomasney JW, Allen LF, Caron MG, Lefkowitz RJ . Identification, quantification, and localization of mRNA for three distinct α1A adrenergic receptor subtypes in human prostate. J Urol 1993; 150: 546–551.
Forray C, Bard JA, Wetzel JM, Chiu G, Shapiro E, Tang R et al. The α1-adrenergic receptor that mediates smooth muscle contraction in human prostate has the pharmacological properties of the cloned human α(1c) subtype. Mol Pharmacol 1994; 45 (4): 703–708.
Nasu K, Moriyama N, Kawabe K, Tfujimoto G, Murai M, Tanaka T et al. Quantification and distribution of α1-adrenoceptor subtype in RNA's in human prostate: comparison of benign hypertrophied and non-hypertrophied tissue. Br J Pharmacol 1996; 119: 797–803.
Malloy BJ, Price DT, Price RR, Bienstock AM, Dole MK, Funk BL et al. α1-Adrenergicsubtypes in human detrusor. J Urol 1998; 160: 937–943.
Foglar R, Shibata K, Horie K, Hirasawa A, Tsujimoto G . Use of recombinant α1-adrenoceptors to characterize subtype selectivity of drugs for the treatment of prostatic hypertrophy. Eur J Pharmacol 1995; 288: 201–207.
Michel MC, Grübbel B, Taguchi K, Verfürth T, Otto T, Kröpfl D . Drugs for treatment of benign prostatic hyperplasia: affinity comparison at cloned α1-adrenoceptor subtypes and in human prostate. J Auton Pharmacol 1996; 16: 21–28.
Richardson CD, Donatucci CF, Page SO, Wilson KH, Schwinn DA . Pharmacology of tamsulosin: saturation-binding isotherms and competition analysis using cloned α1-adrenergic receptor subtypes. Prostate 1997; 33: 55–59.
Yamada S, Suzuki M, Tanaka C, Mori R, Kimura R, Inagaki O et al. Comparative study on α1-adrenoceptor antagonist binding in human prostate and aorta. Clin Exp Pharmacol Physiol 1994; 21: 405–411.
Andersson KE . Uroselectivity. In: Cockett AT, Khoury S, Aso Y, Chatelain C, Denis L, Griffiths K, Murphy G (eds). Proceedings of the 3rd International Consultation on Benign Prostatic Hyperplasia (BPH). Scientific Communications International: New Jersey, 1996, pp 541–542.
Barnas J, Parker M, Guhring P, Mulhall JP . The utility of tamsulosin in the management of orgasm-associated pain: a pilot analysis. Eur Urol 2005; 47 (3): 361–365.
Demyttenaere K, Huygens R . Painful ejaculation and urinary hesitancy in association with antidepressant therapy: relief with tamsulosin. Eur Neuropsychopharmacol 2002; 12: 337–341.
National Cancer Institute. Cancer therapy evaluation program common toxicity criteria, version 2.0. 1998. Available at http://ctep.info.nih.gov/reporting/index.html.
Wilt TJ, MacDonald R, Nelson D . Tamsulosin for treating lower urinary tract symptoms compatible with benign prostatic obstruction: a systematic review of efficacy and adverse effects. J Urol 2002; 167: 177–183.
Segraves RT . Effects of psychotropic drugs on human erection and ejaculation. Arch Gen Psychiatry 1989; 46: 275–284.
Krieger JN, Ross SO, Penson DF, Riley DE . Symptoms and inflammation in chronic prostatitis/chronic pelvic pain syndrome. Urology 2002; 60: 959–963.
Alexander RB, Propert KJ, Schaeffer AJ, Landis JR, Nickel JC, O'Leary MP et al. Chronic Prostatitis Collaborative Research Network. Ciprofloxacin or tamsulosin in men with chronic prostatitis/chronic pelvic pain syndrome: a randomized, double-blind trial. Ann Intern Med 2004; 141 (8): 581–589.
Granados EA, Riley G, Salvador J, Vincente J . Prostatic abscess: diagnosis and treatment. J Urol 1992; 148: 80–82.
Schaeffer AJ, Knauss JS, Landis JR, Propert KJ, Alexander RB, Litwin MS, et al., Chronic Prostatitis Collaborative Research Network Study Group. Leukocyte and bacterial counts do not correlate with severity of symptoms in men with chronic prostatitis: the National Institutes of Health Chronic Prostatitis Cohort Study. J Urol 2002; 168: 1048–1053.
Nickel JC, Alexander RB, Schaeffer AJ, Landis JR, Knauss JS, Propert KJ, Chronic Prostatitis Collaborative Research Network Study Group. Leukocytes and bacteria in men with chronic prostatitis/chronic pelvic pain syndrome compared to asymptomatic controls. J Urol 2003; 170: 818–822.
Petrie WM . Sexual effects of antidepressant and psychomotor stimulant drugs. Mod Probl Pharmacopsychiatry 1980; 15: 77–90.
Shahed AR, Shoskes DA . Correlation of β-endorphin and prostaglandin E2 levels in prostatic fluid of patients with chronic prostatitis with diagnosis and treatment response. J Urol 2001; 166: 1738–1741.
Acknowledgements
I am indebted to the patients who participated in this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Safarinejad, M. Safety and efficacy of tamsulosin in the treatment of painful ejaculation: a randomized, double-blind, placebo-controlled study. Int J Impot Res 18, 527–533 (2006). https://doi.org/10.1038/sj.ijir.3901466
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ijir.3901466
Keywords
This article is cited by
-
Painful Ejaculation: a Contemporary Review
Current Sexual Health Reports (2021)
-
Evaluation and treatment of male pelvic pain syndromes and sexual dysfunction
Current Prostate Reports (2008)
-
Ejaculatory dysfunction: progress in a rarely recognized sexual problem
International Journal of Impotence Research (2006)