Abstract
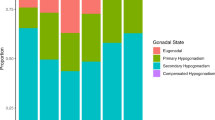
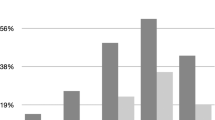
The International Society for the Study of the Aging Male (ISSAM) recommends that a diagnosis be based on a patient's total testosterone (TT), calculated free testosterone (cFT), or calculated bioavailable testosterone (cBT) for partial androgen deficiency of the aging male (PADAM). The purpose of this study was to confirm whether hypogonadism of patients with PADAM is related to symptoms and clarify which criteria of testosterone recommended by ISSAM is suitable for Japanese patients. A total of 90 patients with PADAM symptoms were included in this study. Endocrinologic profiles were reviewed as appropriate, and PADAM symptoms were judged by means of several questionnaires. Laboratory values and symptoms were compared between patients with and without hypogonadism. Even when any criterion of testosterone was used for diagnosis of hypogonadism, AMS (total and subscales), IIEF-5, or SDS scores of PADAM symptoms did not differ significantly between patients classified as having and not having hypogonadism. No other endocrinologic variables than testosterone differed significantly between them, either. PADAM symptoms are not related to testosterone level and it is still obscure whether ISSAM's criterion can be adopted for Japanese patients with PADAM. Other pathology needs to be addressed for evaluation and diagnosis of PADAM in Japan.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Morales A, Lunenfeld B . Investigation, treatment and monitoring of late-onset hypogonadism in males. Official recommendations of ISSAM. International Society for the Study of the Aging Male. Aging Male 2002; 5: 74–86.
Vermeulen A, Verdonck L, Kaufman JM . A critical evaluation of simple methods for the estimation of free testosterone in serum. J Clin Endocrinol Metab 1999; 84: 3666–3672.
Heinemann LA et al. A new ‘aging males' symptoms’ (AMS) rating scale. Aging Male 1999; 2: 105–114.
Heinemann LA et al. The Aging Males' Symptoms (AMS) scale: update and compilation of international versions. Health Qual Life Outcomes 2003; 1: 15.
Morley JE . Androgens and aging. Maturitas 2001; 38: 61–71, discussion 71–63.
Morley JE, Perry III HM . Androgen deficiency in aging men. Med Clin North Am 1999; 83: 1279–1289, vii.
Vermeulen A . Andropause. Maturitas 2000; 34: 5–15.
Morales A, Heaton JP, Carson III CC . Andropause: a misnomer for a true clinical entity. J Urol 2000; 163: 705–712.
Lamberts SW, van den Beld AW, van der Lely AJ . The endocrinology of aging. Science 1997; 278: 419–424.
Barrett-Connor E, Von Muhlen DG, Kritz-Silverstein D . Bioavailable testosterone and depressed mood in older men: the Rancho Bernardo Study. J Clin Endocrinol Metab 1999; 84: 573–577.
Baumgartner RN et al. Predictors of skeletal muscle mass in elderly men and women. Mech Ageing Dev 1999; 107: 123–136.
Abbasi AA et al. Predictors of lean body mass and total adipose mass in community-dwelling elderly men and women. Am J Med Sci 1998; 315: 188–193.
Greendale GA, Edelstein S, Barrett-Connor E . Endogenous sex steroids and bone mineral density in older women and men: the Rancho Bernardo Study. J Bone Miner Res 1997; 12: 1833–1843.
Khosla S, Melton III LJ, Atkinson EJ, O'Fallon WM . Relationship of serum sex steroid levels to longitudinal changes in bone density in young versus elderly men. J Clin Endocrinol Metab 2001; 86: 3555–3561.
Khosla S et al. Relationship of serum sex steroid levels and bone turnover markers with bone mineral density in men and women: a key role for bioavailable estrogen. J Clin Endocrinol Metab 1998; 83: 2266–2274.
Tsujimura A et al. Bioavailable testosterone with age and erectile dysfunction. J Urol 2003; 170: 2345–2347.
T'Sjoen G, Goemaere S, De Meyere M, Kaufman JM . Perception of males' aging symptoms, health and well-being in elderly community-dwelling men is not related to circulating androgen levels. Psychoneuroendocrinology 2004; 29: 201–214.
T'Sjoen G et al. Self-referred patients in an aging male clinic: much more than androgen deficiency alone. Aging Male 2003; 6: 157–165.
Acknowledgements
We are very grateful to M Omune, M Oki, and S Tanabe of our laboratory for assistance in sample collection and for useful discussions.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tsujimura, A., Matsumiya, K., Miyagawa, Y. et al. Comparative study on evaluation methods for serum testosterone level for PADAM diagnosis. Int J Impot Res 17, 259–263 (2005). https://doi.org/10.1038/sj.ijir.3901300
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ijir.3901300
Keywords
This article is cited by
-
Association Between Serum Testosterone and Serum PSA Among Men With and Without Partial Androgen Deficiency
Indian Journal of Clinical Biochemistry (2020)
-
Alternative Treatment Modalities for the Hypogonadal Patient
Current Urology Reports (2014)
-
Recent topics related to testosterone deficiency syndrome in Japan
Asian Journal of Andrology (2011)
-
The prevalence and risk factors for glucose intolerance in young Korean women with polycystic ovary syndrome
Endocrine (2009)
-
The aging males’ symptoms scale for Japanese men: reliability and applicability of the Japanese version
International Journal of Impotence Research (2008)