Abstract
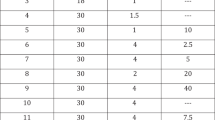
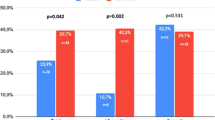
Erectile dysfunction (ED) has frequently been associated with Peyronie's Disease (PD) and may further compromise coitus. This is a retrospective analysis of ED in patients with PD since the release of sildenafil citrate (SC) focusing specifically on our patients' responses to SC. One-hundred seventy six patients with PD were evaluated between April 1998 and May 2001. All patients received a complete medical and sexual history, physical exam, penile duplex ultrasound (PDU, with 30–90 mg of papaverine) to assess penile vascular integrity, plaque dimensions, and erect penile deformity. Based on these findings, appropriate treatment options were offered for their PD and their ED including SC, which was offered to 73 men. Patient response to SC was specifically assessed during patient office interview and via a mailed EDITS (Erectile Dysfunction Inventory of Treatment Satisfaction) questionnaire. Seventy (39.8%) and 104 (59.1%) patients complained of decreased erectile capacity (ie rigidity) occurring before and after the onset of PD, respectively. Only two patients reported no change of erectile capacity. In all, 103 (58.5%) patients complained of significant reduction in sexual function due to diminished rigidity and sought treatment for their ED. Of the ED treatment options available, 73 (70.9%) patients were given a prescription for SC. Forty-eight (75.0%) patients returned the EDITS questionnaire while four of 73 (5.5%) patients did not fill their prescription and five of 73 (6.8%) did not engage in sexual activity following an initial trial of SC due to side effects (flushing, headaches). Based upon the EDITS response, 34 of 48 (70.8%) patients reported that they were either very satisfied or somewhat satisfied, five of 48 (10.4%) patients were neither satisfied nor dissatisfied, and nine of 48 (18.8%) patients were somewhat dissatisfied or very dissatisfied with the effectiveness of SC in enhancing their erectile response. No patient reported worsening of PD deformity or an increase in penile pain. The 30 patients who were not prescribed SC chose the following options to enhance rigidity: eight (7.8%) underwent prosthesis placement, four (3.9%) opted for vacuum constriction device (VCD), four (3.9%) chose intracorporal injections, and 14 (13.6%) used no adjunctive therapy. Erectile dysfunction is a problem associated with PD and all typical treatment options are acceptable. However, to our knowledge, there is no published study reviewing the efficacy of SC in patients with ED associated with PD. There appears to be no contraindication to using SC as being the least invasive and most convenient treatment option for ED with PD. Although the potential risk of coital trauma to the erect penis with PD is present, there is no evidence from this study that erections and coitus enhanced specifically by SC resulted in worsening deformity or progression of the PD. EDITS questionnaire results reveal that SC is an agent that allowed successful coitus in 70.8% of males with PD.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Schroder-Printzen I, Hauck EW, Weidner W . New aspects in Peyronie's disease—a mini-review Andrologia 1999; 31: 31–35.
Hellstrom WJG, Bivalacqua TJ . Peyronie's disease: etiology, medical, and surgical therapy J Androl 2000; 21: 347–354.
Lopez JA, Jarow JP . Penile vascular evaluation of men with Peyronie's disease J Urol 1993; 149: 53–55.
McMahon CG, Samali R, Johnson H . Efficacy, safety and patient acceptance of sildenafil citrate as treatment for erectile dysfunction J Urol 2000; 164: 1192–1196.
Levine LA, Coogan CL . Penile vascular assessment using color duplex sonography in men with Peyronie's disease J Urol 1996; 155: 1270–1273.
Althof SE et al. Edits: development of questionnaires for evaluating satisfaction with treatments for erectile dysfunction Urology 1999; 53: 793–799.
Weidner W, Schroeder-Printzen I, Weiske WH, Vosshenrich R . Sexual dysfunction in Peyronie's Disease: an analysis of 222 patients without previous local plaque therapy J Urol 1997; 157: 325–328.
Jarow JP, Burnett AL, Geringer AM . Clinical efficacy of sildenafil citrate based on etiology and response to prior treatment J Urol 1999; 162: 722–725.
The Process of Care Consensus Panel. Position paper: the process of care model for evaluation and treatment of erectile dysfunction Int J Impot Res 1999; 11: 59–74.
Sadovsky R, Miller T, Moskowitz M, Hackett G . Three-year update of sildenafil citrate (Viagra) efficacy and safety Int J Clin Pract 2001; 55: 114–128.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Levine, L., Latchamsetty, K. Treatment of erectile dysfunction in patients with Peyronie's disease using sildenafil citrate. Int J Impot Res 14, 478–482 (2002). https://doi.org/10.1038/sj.ijir.3900912
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ijir.3900912
Keywords
This article is cited by
-
Characterization of a novel rabbit model of Peyronie’s disease
International Journal of Impotence Research (2023)
-
Long-term outcomes of extracorporeal shock wave therapy for acute Peyronie’s disease: a 10-year retrospective analysis
International Journal of Impotence Research (2023)
-
Daily low-dose tadalafil may reduce the penile curvature progression rate in patients with acute Peyronie’s disease: a retrospective comparative analysis
International Journal of Impotence Research (2022)
-
Nonsurgical management of Peyronie’s disease
Nature Reviews Urology (2019)
-
Management of the Acute Phase of Peyronie’s Disease: a Contemporary Review
Current Sexual Health Reports (2019)