Abstract
True hermaphroditism (TH) refers to individuals who have both unequivocal ovarian tissue and testicular elements regardless of their karyotypes; whereas mixed gonadal dysgenesis (MGD) refers to individuals who usually have a differentiated gonad on one side and a streak gonad or streak testis on the other side. A differential diagnosis between the TH and MGD has important clinical implications for gender assignment and the decision for early gonadectomy; however, variable clinical and histological features frequently lead to the confusion of TH with MGD. We reviewed the clinicopathological features of TH (n = 4) and MGD (n = 6) in young children to identify which morphological features are important for a differential diagnosis between the two conditions. In both conditions, the testicular compartment was composed of immature seminiferous tubules lined by immature Sertoli cells and primitive germ cells; this finding was not helpful for a differential diagnosis. The ovarian compartment in TH cases showed numerous primordial follicles containing primary oocytes with a few primary or antral follicles; however, ovarian compartments in patients with MGD were characterized by primitive sex-cordlike structures with or without germ cell components within the ovarian-type stroma, mimicking gonadoblastomas in two cases and granulosa cell or Sertoli cell tumors in three cases. Hormonal profiles, cytogenetic results, and an internal duct system were not helpful in a differential diagnosis. In conclusion, a differential diagnosis between TH and MGD is largely dependent on the histological features of the gonads. Therefore, examination of all resected or biopsied tissue and the application of strict histological criteria are important.
Similar content being viewed by others
INTRODUCTION
There is much confusion about the nomenclature for patients with gonadal dysgenesis. Asymmetrical gonadal dysgenesis is the term used if one gonad displays more complete development and can be identified as an ovary or testis (usually testis), and the other gonad is a streak (1). Most patients with asymmetrical gonadal dysgenesis have testicular tissue on one side and a streak gonad on the other side. Some authors reserve the term mixed gonadal dysgenesis (MGD) for individuals who present a 45,X/46,XY karyotype with a testis on one side and a streak on the other side (1); other authors apply the term to all patients who have varying degrees of asymmetrical gonadal dysgenesis with testicular differentiation on either side, bilateral streak testis, or bilateral dysgenetic testis (2, 3); in contrast, true hermaphroditism (TH) is the rarest form of intersexuality in humans, and the term is applied to an individual who has both well-developed ovarian and testicular tissues. A differential diagnosis between the two conditions has important clinical implications for gender assignment; furthermore, early gonadectomy in MGD patients is needed to prevent the development of malignant germ cell tumors. However, the form of intersexuality is sometimes very difficult to determine without a knowledge of normal histological findings of the gonads in newborns and young children. It is also true in adults, especially when both gonads are replaced by malignant tumors or when the gonads have various secondary histological changes. In young children, histological features of the gonads remain relatively unchanged, and they are helpful for understanding the histological differences between the TH and MGD. We review the clinicopathological features of TH and MGD in 10 young children to identify the most important features for differentiating between the two conditions and to emphasize the role of the pathologist in the correct diagnosis.
MATERIALS AND METHODS
Ten cases of TH (n = 4) and MGD (n = 6) at the age of ≤3 years were found in the surgical pathology files from January 1991 to December 2001 in the Department of Pathology at the Asan Medical Center in Seoul, Korea. The pathology reports and clinical records, including age, reared sex, cytogenetic results, hormonal profiles, and operative findings, were reviewed for all 10 patients. Chromosomal analysis had been performed in all 10 cases on peripheral lymphocytes using conventional techniques. To check testicular function, a human chorionic gonadotropin (hCG) stimulation test, giving 1000 U/d for 3 days and measuring testosterone before and after stimulation, was performed in six patients (Cases 1–3, 6, 8, and 9).
Testicular tissue in TH was defined by the presence of seminiferous tubules with spermatogonia, and ovarian tissue was defined by the presence of numerous primordial and/or maturing follicles within the ovarian stroma.
MGD was diagnosed in all patients who have varying degrees of structural and functional abnormalities of the gonads, which included cases showing differentiated testis with a contralateral streak gonad, bilateral streak testes, a streak testis with a streak gonad, a streak testis with a differentiated prepubertal testis, and bilateral dysgenetic testes. Streak testis referred to the cases in which streak tissue was additionally identified at the peripheral portion of the differentiated testis (2). Streak or streak gonad referred to the case composed almost exclusively of ovarian-type stroma without differentiated gonadal structures.
RESULTS
Clinical Features
These are summarized in Table 1. The patients' ages at the time of their first visit to the hospital ranged from 1 to 36 months (mean, 18.1 mo). All 10 patients presented with ambiguous external genitalia that were detected by their parents, and all of the patients were reared as males because of the size of the phallus. In four cases of TH, cytogenetic studies using peripheral blood showed different karyotypes. The six patients with MGD had the 45,X/46,XY karyotype in four cases, chromosomal mosaicism consisting of 45,X(93)/46,X,add(Y)(p11.3) (7) in one, and 46,XY in one (Table 1). Remnants of the Müllerian or Wolffian ducts were variably identified regardless of karyotype or gonadal structures. A rudimentary uterus or a part of a fallopian tube was identified in all but one case.
The hormonal profiles of the patients were not consistent. A 17α-hydroxyprogesterone level was in the normal range in two cases, and thereby the possibility of congenital adrenal hyperplasia could be excluded there. Serum luteinizing hormone and follicle-stimulating hormone levels were low but normal for this age. Human chorionic gonadotropin stimulation tests were performed in three cases of TH (Cases 1–3) and in three cases of MGD (Cases 6, 8, and 9), but only one patient who had TH showed a positive response.
The ages of the four TH patients at the time of gonadectomy or biopsy ranged from 14 to 36 months (mean, 23.8 mo). In two patients, bilateral gonadectomies were performed because these two patients were clinically diagnosed as having MGD. In the remaining two cases, normal-appearing gonads were not removed. In one case, a unilateral gonadectomy with a biopsy on the opposite gonad was performed; and in the other case, only a unilateral gonadectomy was performed because the opposite gonad appeared radiologically and grossly normal.
The ages of the six patients with MGD at the time of gonadectomy or biopsy ranged from 1 to 24 months (mean, 14.3 mo). A bilateral gonadectomy was performed in three patients, and a unilateral gonadectomy with a biopsy of the contralateral normal-appearing gonads in the remaining three patients. The latter three patients are undergoing close clinical follow-ups for gonadal tumors by ultrasonography.
Histological Features
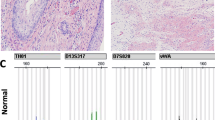
Of four cases of TH, two cases were classified as unilateral type and the other two as lateral according to the location of the gonadal tissue (4). In two cases having unilateral ovotestis, the ovarian and testicular tissue were arranged in an end-to-end fashion. Histological features of gonadal tissue were similar in all cases of TH. The testicular compartment showed numerous solid seminiferous tubules filled with immature Sertoli cells and a few primitive germ cells. The immature Sertoli cells had a regular, round to ovoid nucleus with inconspicuous nucleoli. The germ cells were found adjacent to the basement membrane and those were distinguishable from the immature Sertoli cells because of their larger nuclei and abundant cytoplasm. In three cases (Cases 2–4), the tubules were compact with scanty amount of interstitium (Fig. 1A), and one case (Case 1) showed edematous and abundant interstitium. The interstitium contained undifferentiated spindle cells, but mature Leydig cells were not identified in any case. In the ovarian compartment, numerous primordial follicles and a few primary and antral follicles were found in the condensed outer cortex (Fig. 1B). In the primordial follicles, a single layer of flattened follicular cells (pregranulosa cells) surrounded the oocytes. Oocytes in the follicles measured about 40–60 μm in diameter and had a large, centrally located or eccentric nucleus with finely dispersed chromatin and one or more large nucleoli (Fig. 1C).
Case 3. Ovotestis in true hermaphrodite. A, testicular compartment shows solid tubules filled with immature Sertoli cells and germ cells (arrow). B, ovarian compartment has numerous primordial and growing follicles containing primary oocytes within the ovarian cortical stroma. C, primordial follicles are invested by a single layer of flattened follicular cells (arrow), and each contains a primary oocyte.
In all six cases of MGD, the histological features of the differentiated gonad (testis) were indistinguishable from the testicular compartment in TH. Within the solid seminiferous tubules, germ cell components were contrasted with the immature Sertoli cells. As in cases of TH, the number of germ cells were low in the cases having compact tubules (Cases 5, 9), but the number was increased up to 10 per tubule in two cases with an edematous and abundant interstitium (Cases 6 and 10; Fig. 2A). In three cases (Cases 5, 6, and 10), psammomatous calcifications were noted in the center of the tubules. In two cases (Cases 5 and 10), the stroma of the peripheral portion of the differentiated testis imperceptibly merged into ovarian-type stroma, in which primitive germ cells and stromal cells were intimately admixed and formed primitive sex-cordlike structures (Figs. 2B, 3A). These features mimicked those of gonadoblastoma; however, the characteristic features of gonadoblastoma, such as cellular nests showing hyaline Call-Exner-like bodies or calcification, were not present. Mitotic figures were not seen in either germ cell or sex-cordlike components. In three cases (Cases 6, 8, and 9), the side contralateral to the differentiated gonads showed anastomosing trabeculae or cordlike structures composed of immature sex-cordlike elements. Germ cell components were rare or absent in the cordlike structures in those cases; these findings were reminiscent of the granulosa cell or Sertoli cell tumors (Fig. 3B). In one case (Case 9), germ cells were only rarely identified within the trabeculae, and these were intimately associated with lymphoid aggregates (Fig. 3C). The contralateral gonad in one case (Case 7) had streak tissue composed almost exclusively of ovarian-type stroma with rare foci of atrophic sex-cordlike structures composed of barely recognizable tubular or cordlike structures (Fig. 3D). Primordial or growing follicles were not identified in any cases of MGD.
Case 5. Mixed gonadal dysgenesis. A, testicular compartment has histological features similar to those of true hermaphrodite; the number of germ cells (arrow) is increased in a case with abundant edematous interstitium compared with in the cases that have compact tubules. B, the stroma of the differentiated testis imperceptibly merges into the adjacent dysgenetic gonadal tissue (left half), where germ cell and stromal cell components form primitive cordlike structures in the ovarian-type stroma; primordial or growing follicles are not identified.
Sex-cordlike components in mixed gonadal dysgenesis. A, trabeculae or cordlike structures consisting of an intimate mixture of primitive germ cells and stromal cells mimic features of gonadoblastoma (Case 5). B, sex-cordlike structures composed only of stromal cells are reminiscent of those in adult granulosa cell tumor or Sertoli cell tumor (Case 6). C, only a few germ cells (arrow) are identified in the sex-cordlike structures, and these are associated with many scattered lymphoid aggregates. D, streak gonad is almost exclusively composed of ovarian-type stroma and rare foci of atrophic sex-cordlike structures (arrow).
DISCUSSION
The differentiation of TH from MGD is important for three reasons. First, a bilateral gonadectomy is recommended as soon as possible in all individuals with MGD containing Y-chromosome material. There is no benefit in delaying surgery because approximately one third of patients with MGD develop gonadoblastoma during the 1st to 4th decades of life (3) and because 30% of gonadoblastomas are overgrown by more malignant germ cell tumors, such as germinoma, endodermal sinus tumor, immature teratoma, embryonal carcinoma, or choriocarcinoma (2, 3). In TH, however, only the removal of the opposite gonad from the assigned gender and a biopsy of remaining gonadal tissue for histological evaluation may be appropriate. Second, gender assignment is critical for the treatment of patients of TH because these patients usually do not possess any other developmental malformations, and thus normal sexual and reproductive functions can be achieved by proper management and sex assignment at a young age (4). After the removal of the testicular portion of an ovotestis, about 38% of the TH patients with a 46,XX karyotype menstruate by age 14 years (5); ovulation (6) and successful childbearing have also been described (8, 9, 10, 11). In contrast, it is important that bilateral gonadectomies be performed in patients with MGD before the patient reaches puberty, not only to prevent the development of malignant tumors but also to avoid virilization if the patient is to be raised as female. In the three patients with MGD in our study, however, contralateral differentiated gonads have been preserved under close clinical follow-up until the patients' puberty so that they can be raised as male. Third, certain medical problems, such as deficient immunoglobulin levels, aberrant bony development of inner ear structures, and cardiovascular and renal anomalies, are more common in MGD patients than in TH patients; therefore, patients with MGD should receive more medical attention (1, 3).
For a differential diagnosis, chromosomal constitutions are not helpful. Various types of chromosomal abnormalities have been described in cases of TH, such as 46,XX; 46,XY; 46,XX/46,XY; 45X/46,XY; and others (5, 6, 7, 8, 9, 10, 11). MGD cases also have heterogeneous chromosomal changes but are usually characterized by a 45,X/46,XY; 45,X/47,XYY; or 46,XY karyotype (12). The pathogenesis of TH and MGD still remains unclear, but recent study shows that sex determination is not from a simple hierarchical cascade of gene action but from a complex network of gene expression and protein-protein interaction in which SRY, SOX9, WT1, and SF1 are involved (13, 14). In cases of 46,XX true hermaphroditism, mosaicism with a Y-bearing cell line at low level (15) or partial inactivation of the Y-bearing X chromosome that was formed during paternal meiosis (16, 17) have been suggested to explain the mechanism of abnormal sexual development. In cases of MGD, mutations in SRY genes were usually absent (18); however the cytogenetic mosaicism, mutation in the genes downstream of SRY, and unpaired or incompletely paired X chromosome have been proposed as a mechanism to cause defective formation of the follicular mantle and degeneration of oocytes (19).
Approximately 400,000 primordial follicles, each containing a primary oocyte, are embedded in the stroma of the normal ovarian cortex at birth, and oogonia or primordial germ cells are usually absent (20, 21). Therefore, the presence of numerous primordial follicles containing primary oocytes with or without maturing follicles is considered well-developed ovarian tissue when making a definitive diagnosis of TH after birth and the finding of rare primordial follicles is insufficient to call it ovarian tissue. More mature follicular structures, such as primary or antral follicle, can be identified, but those are not absolutely required for the diagnosis of TH. Primitive sex-cordlike structures with many primordial germ cells after birth should not be confused with well-developed ovarian tissue, even if they are embedded in the ovarian-type stroma.
It is noteworthy that five of six cases with MGD in our study showed either gonadoblastoma-like or sex-cord stromal tumor-like areas. Numerous germ cell components were intimately admixed with sex-cordlike elements in the former, whereas most of the germ cell components were eliminated in the latter. Scattered lymphoid aggregates with a rare germ cell component within the ovarian-type stroma in a case (Case 9) raised the possibility of an immune mechanism involved in the degenerative process forming a streak gonad. The number of primordial germ cells varies depending on the age of the patient at the time of histological diagnosis, and virtually none are detectable at the time of puberty (2). Therefore, we thought that the germ cells migrated to the genital ridge and that then, accelerated atresia of primordial germ cells and sex-cord stromal cells occurred to form streak gonad during the prenatal or early postnatal period.
Gonadoblastoma was named as such because it appeared to recapitulate gonadal development more completely than any other type of tumor (22). However, the size of the gonadoblastoma-like or granulosa cell tumor-like areas in our cases was too small to diagnose as such, and they did not exhibit mitotic activity. Furthermore, those structures showed sequential changes of degeneration of the germ cells and sex-cord stromal cells in the ovarian-type stroma (Fig. 3A–D).
The presence of testicular tissue does not completely inhibit ovarian function; therefore, the histological appearance of the ovarian compartment of an ovotestis is usually normal, and it may show evidence of ovulation at puberty in about 50% of cases (6). On the other hand, secretion of the testicular hormone is inhibited by the negative feedback effect of ovarian steroids through the inhibition of gonadotropin (4). In our study, the testicular compartments of patients with TH were those of normal prepubertal (immature) testes and were indistinguishable from those of patients with MGD (Fig. 1A). However, as patients get older, the testicular compartments in TH patients show more frequent abnormalities, such as tubular atrophy, poor germ cell development, Leydig cell hyperplasia, and sclerosis, because the pituitary gonadotropins can be suppressed by the negative feedback effect of ovarian steroids secreted by ovarian compartment (4, 6) and because these are the major regulators of spermatogenesis in human testes. Clinically, the presence of functional testicular tissue can be determined with the use of an hCG stimulation test in an adult. A rise in testosterone level indicates the presence of functioning Leydig cells. However, in young children, the test may not reflect the function of normal testicular tissue because of the poorly developed Leydig cells in the interstitium in both conditions. In our study, hCG stimulation tests were performed in 6 of 10 patients (three TH and three MGD patients), but only one patient with TH showed an elevated testosterone level, suggesting the presence of functioning Leydig cells.
The nature of the internal or external genitalia does not form the basis of a differential diagnosis between TH and MGD. In normal male embryos, anti-Mullerian hormone (AMH) secreted by the pre-Sertoli cells causes rapid regression of the müllerian ducts between the 8th and 10th weeks (20, 21). In our cases, remnants of the müllerian duct structure, rudimentary uterus, and fallopian tube were identified in all but one case in both TH and MGD. In individuals with TH or MGD, it is likely that AMH is deficient or that paramesonephric ducts do not respond to normal AMH.
In conclusion, the differentiation between TH and MGD is largely dependent on the histological appearances of the gonads. Clinical features, such as cytogenetic results, hormonal profiles, and internal duct systems do not appear to be useful in a differential diagnosis. Therefore, thorough examination of all the resected or biopsied gonadal tissue and the application of strict histological criteria for defining ovarian tissue, the presence of numerous primordial or maturing follicles containing primary oocytes when making a definitive diagnosis of TH after birth are important for the differentiation between the two conditions.
References
Plouffe L Jr, McDonough PG . Ovarian agenesis and dysgenesis.In: Adashi EY, Rock JA, Rosenwaks Z, editors. Reproductive endocrinology, surgery, and technology. Philadelphia: Lippincott-Raven; 1996. p. 1366–1384.
Tumors of the ovary, maldeveloped gonads, fallopian tube, and broad ligament.In: Scully RE, Young RH, Clement PB, editors. Atlas of tumor pathology. 3rd series. Washington, D.C.: Armed Forces of Institute of Pathology; 1998. p. 399–408.
Robboy SJ, Bentley RC, Russel P . Embryology of the female genital tract and disorders of abnormal sexual development.In: Kurman RJ, editor. Blaustein's pathology of the female genital tract. 5th ed. New York: Springer; 2002. p. 22–36.
Hasty LA, Rock JA . True hermaphroditism.In: Adashi EY, Rock JA, Rosenwaks Z, editors. Reproductive endocrinology, surgery, and technology. Philadelphia: Lippincott-Raven; 1996. p. 978–988.
van Niekerk WA . True hermaphroditism: an analytic review with a report of 3 new cases. Am J Obstet Gynecol 1976; 126: 890–907.
van Niekerk WA, Retief AE . The gonads of human true hermaphrodites. Hum Genet 1981; 58: 117–122.
Damiani D, Fellous M, McElreavery K, Barbaux S, Barreto ESA, Dichtchekenian V, et al. True hermaphroditism: clinical aspects and molecular studies in 16 cases. Eur J Endocrinol 1997; 136: 201–204.
Starceski PJ, Sieber WK, Lee PA . Fertility in true hermaphroditism. Adolesc Pediatr Gynecol 1988; 1: 55–56.
Williamson HO, Phansey SA, Manthur RS . True hermaphroditism with twin vaginal delivery and a review. Am J Obstet Gynecol 1981; 141: 262–265.
Tanaka Y, Fujiwara K, Yamauchi H, Mikami Y, Kohno I . Pregnancy in a woman with a Y chromosome after removal of an ovarian dysgerminoma. Gynecol Oncol 2000; 79: 519–521.
Tiltman AJ, Sweets SM . Multiparity in a covert true hermaphrodite. Obstet Gynecol 1982; 60: 752–754.
Méndez JP, Ulloa-Aguirre A, Kofman-Alfaro S, Mutchinick O, Fernández-del-Castillo C, Reyes E, et al. Mixed gonadal dysgenesis: clinical, cytogenetic, endocrinological, and histopathological findings in 16 patients. Am J Med Genet 1993; 46: 263–267.
Clarkson MJ, Harley VR . Sex with two SOX on: SRY and SOX9 in testis development. Trends Endocrinol Metab 2002; 13: 106–111.
Lovell-Badge R, Canning C, Sekido R . Sex-determining genes in mice: building pathways. Novartis Found Symp 2002; 244: 4–18.
Ortenberg J, Oddoux C, Craver R, Mcelreavey K, Salas-Cortes L, Guillen-Navarro E, et al. SRY gene expression in the ovotestes of XX true hermaphrodites. J Urol 2002; 167: 1828–1831.
Fechner PY, Rosemberg C, Stetten G, Cargile JB, Pearson PI, Smith KD, et al. Nonrandom inactivation of the Y-bearing X chromosome in a 46, XX individual: evidence for the etiology of 46, XX true hermaphroditism. Cytogenet Cell Genet 1994; 66: 22–26.
Margarit E, Coll MD, Oliva R, Gomez D, Soler A, Ballesta F . Sry gene transferred to the long arm of the X chromosome in a Y-positive XX true hermaphrodite. Am J Med Genet 2000; 90: 25–28.
Alvarez-Nava F, Soto M, Borjas L, Ortiz R, Rojas A, Martinez S, et al. Molecular analysis of SRY gene in patients with mixed gonadal dysgenesis. Ann Genet 2001; 44: 155–159.
Yeh J, Adashi EY . The ovarian life cycle.In: Yen SSC, Jaffe RB, Barbieri RL, editors. Reproductive endocrinology, physiology, pathophysiology, and clinical management. 4th ed. Philadelphia: W.B. Saunders; 1999. p. 153–190.
Larsen WJ . Development of the urogenital system.In: Larsen WJ, editor. Human embryology. 2nd ed. New York: Churchill Livingstone; 1997. p. 261–309.
Carlson BM . Urogenital system.In: Carlson BM, editor. Human embryology and developmental biology. 2nd ed. St. Louis, MO: Mosby; 1999. p. 380–385.
Scully RE . Gonadoblastoma. A review of 74 cases. Cancer 1970; 25: 1340–1356.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, KR., Kwon, Y., Joung, J. et al. True Hermaphroditism and Mixed Gonadal Dysgenesis in Young Children: A Clinicopathologic Study of 10 Cases. Mod Pathol 15, 1013–1019 (2002). https://doi.org/10.1097/01.MP.0000027623.23885.0D
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1097/01.MP.0000027623.23885.0D
Keywords
This article is cited by
-
The clinical and genetic heterogeneity of mixed gonadal dysgenesis: does “disorders of sexual development (DSD)” classification based on new Chicago consensus cover all sex chromosome DSD?
European Journal of Pediatrics (2012)
-
Dysgerminoma in a case of 46, XY pure gonadal dysgenesis (swyer syndrome): a case report
Diagnostic Pathology (2011)