Abstract
Multiple mechanisms, such as gene mutations, amplifications, and rearrangements, as well as perturbed mitogen and receptor function, are likely to contribute to glioma formation. The MET (also known as c-met) proto-oncogene located at 7q31-34 has been shown to be amplified in human gliomas, and activating mutations within the tyrosine kinase domain of MET have been causally related to tumorigenesis in hereditary papillary renal cell carcinoma. To elucidate the role of MET gene in glioma formation, sporadic gliomas from 11 patients were examined for MET gene mutations and allelic duplications or deletions by polyermase chain reaction-single strand conformational polymorphism analysis and fluorescence in situ hybridization. Three of 11 sporadic gliomas showed a deletion of one copy of the MET gene, and a specific MET gene missense mutation in the remaining gene copy was detected in one of those tumors. The corresponding sequence in non-tumor DNA was normal in all cases. Three of 11 sporadic gliomas showed duplication of one copy of the MET gene, but none of them contained mutations. One tumor showed MET amplification without mutation. Three showed neither allelic change nor mutation. These data suggest that somatic MET gene mutation may play a role in the development of a subgroup of sporadic gliomas. However, MET mutations appear to be absent in the majority of sporadic gliomas.
Similar content being viewed by others
INTRODUCTION
Gliomas are the most frequent primary tumors of the central nervous system in humans (1). The most consistent chromosomal abnormalities in aggressive gliomas are gains of chromosome 7 or losses of chromosome 10, which are present in 80 to 90% of cases (2, 3, 4). As has been demonstrated in a number of other cancers, multiple oncogenes, such as MET, SAS, N-MYC, and c-MYC, have been implicated in glioma formation (5, 6, 7, 8).
Increased MET-hepatocyte growth factor/scatter factor signaling, as well as MET amplifications, overexpression, or activation by point mutation, have been demonstrated in a number of tumors, both in vivo and in vitro (9, 10, 11). Di Renzo et al. (12) have shown elevated levels of MET mRNA in glioma tissues, and hepatocyte growth factor/scatter factor has been shown to stimulate growth, migration, and invasiveness of cultured glioma cell lines (8). MET gene amplification has been detected in some glioblastomas (GBMs) (13). Increased expression of MET has been shown to correlate with astrocytoma progression (14) and may be related to greater biologic aggressiveness found with GBMs (15).
Recently, mutations within the tyrosine kinase domain of MET have been implicated in tumorigenesis of both sporadic and hereditary papillary renal cell carcinoma (HPRC) (11, 16). Because a strong correlation between the enzymatic and biologic transforming activity of mutations in the tyrosine kinase domain of MET has been shown to relate tumorigenesis to the level of MET activation, we screened a variety of human gliomas for mutations in exons 15–19 of the MET gene by polyermase chain reaction (PCR)-based single strand conformational polymorphism (SSCP) analysis and examined allelic deletion or duplication by fluorescence in situ hybridization (FISH) and PCR-based allelic quantitative analysis.
MATERIALS AND METHODS
Patients and Specimens
Surgical specimens were obtained from patients who underwent craniotomy and tumor resection in the Surgical Neurology Branch at the National Institutes of Health, as part of institutional review board-approved protocols, for which informed consent was obtained. At the time of tumor resection, specimens were frozen at −70° C until later use.
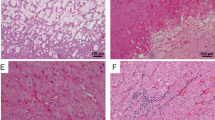
Nine-micron thick sections were placed on glass slides and air dried. These slides were compared with sections that were stained with hematoxylin and eosin to guide the area of dissection. Histologic fields of interest also were compared with the original hematoxylin and eosin pathologic slides to ensure uniformity of tumor selection.
Specimens were suspended in 30 μL of DNA extraction solution, which contained 50 mm Tris-HCl, 1 mm ethylenediamine-tetraacetic acid, 1.0% Tween-20, and 0.1 mg/mL proteinase K (pH 8.0). This mixture was incubated overnight at 37° C; proteinase K was inactivated by heating at 95° C for 10 min (17).
SSCP Analysis for MET Mutations
PCR-SSCP analysis was performed by the modification of the method of Orita et al. (18) with intronic sequences designed to amplify exons 15 to 19 from tumor and normal DNA. Each PCR sample contained 1.0 μL of template DNA, 10 pmol of each primer, 20 nmol each of dGTP, dATP, dTTP, dCTP, 15 mm MgCl2, 0.1 unit of Taq DNA polymerase (Perkin-Elmer, Foster City, CA), 0.05 μL of [32P] dCTP (6000 Ci/mmol), and 1 μL of 10 × buffer in a total volume of 10 μL. PCR was performed for 35 cycles: denaturation at 94° C for 40 sec, annealing at 52 to 54° C for 40 sec, and extension at 72° C for 40 sec. The final extension was continued for 10 min. The labeled amplified DNA (2 μL) was mixed with an equal volume of formamide loading dye (95% formamide, 20 mm ethylenediamine-tetraacetic acid, 0.05% bromophenol blue, and 0.05% xylene cyanol). The samples were denatured for 5 min at 95° C and loaded onto a SSCP gel (MDE; FMC BioProducts, Rockland, ME) with 10% glycerol. Samples were electrophoresed at 8 W at room temperature overnight. After electrophoresis, the gels were transferred to 3-mm Whatman paper and dried, and autoradiography was performed with Kodak X-OMAT film (Eastman Kodak, Rochester, NY). After detection of a mutant allele, DNA was extracted from the excised aberrant band of the SSCP gel by overnight incubation in 50 μL of distilled water at room temperature and subsequently reamplified by PCR. The PCR products were directly sequenced (Cycle Sequencing Kit, Perkin-Elmer), and normal and tumor DNA sequences were compared.
FISH
FISH was performed with touch preparations of frozen brain tumor specimens. The probe for chromosome 7 was cosmid c182b3, which contains a portion of the MET proto-oncogene (a gift of S. W. Scherer, Hospital for Sick Children, Toronto, Canada). A chromosome 7 specific α-satellite probe (Oncor, Gaithersburg, MD), biotin-labeled, was used as a control.
In situ hybridization and detection procedures were performed according to the technique described by Pack et al. (19). In brief, cosmid DNA was labeled by nick translation (Boehringer Mannheim, Indianapolis, IN) with digoxigenin-11-dUTP and ethanol precipitated in the presence of 50 × herring sperm DNA (Boehringer Mannheim, Indianapolis, IN) and 50 × Cot-1 human DNA (Boehringer Mannheim, Indianapolis, IN). The DNA pellet was re-suspended in Hybrisol solution [50% deionized formamide/10% dextran sulfate/2 × standard saline citrate (SSC)] to a final concentration of 25 ng/mL. Slides were denatured in 70% formamide/2 × SSC at 72° C for 2 min, dehydrated in a cold (−20° C) ethanol series of 70, 80, 90, and 100% for 2 min each, then air-dried. Probes were denatured at 78° C for 10 min, then incubated for 30 min at 37° C for pre-annealing. A total of 250 μg of DNA probe was applied to the slide. Chromosome 7-specific, α-satellite repetitive DNA was denatured separately and mixed with the cosmid probe just before hybridization. Overnight hybridization was performed in a humidified chamber at 37° C.
Post-hybridization washes were at 45° C in 50% formamide/2 × SSC (5 min × 3), 1 × SSC (5 min × 2), and 0.1 × SSC (5 min × 2). Detection was performed using avidin-FITC (Vector Laboratories, Burlingame, CA) and anti-digoxigenin rhodamine (Boehringer Mannheim, Indianapolis, IN) (40 min at 37° C) followed by washing in 4 × SSC/0.1% Tween-20 at 45° C and counterstaining with DAPI-antifade (0.25 mg/mL).
Hybridization signals were scored using a Zeiss Axiophot epifluorescence microscope (Zeiss, Thornwood, NY), and two-color images were captured on a Photometrics charge-coupled device camera (Photometrics, Tucson, AZ) using IP Lab image software (Scanalitics Inc., Fairfax, VA). At least 100 interphases with strong hybridization signals were scored. Normal brain tissue control showed <6% of cells with one MET gene signal. Alterations of MET copy numbers were scored when present in at least 30% of cells.
RESULTS
Brain tissue containing normal and neoplastic cells was obtained at the time of surgery, snap-frozen, and frozen sections were cut. Selective tissue microdissection was used to obtain discrete populations of normal and neoplastic cells, which were analyzed for mutations of the MET proto-oncogene. There were seven patients with GBM multiforme, three with low-grade oligodendrogliomas, two with anaplastic astrocytomas, and one with anaplastic oligodendroglioma (Table 1).
We analyzed exons 15, 16, 17, 18, and 19, the most commonly affected regions of the MET gene, for mutations via SSCP and sequencing. One of 11 cases (Case 3) exhibited an aberrant band in SSCP (Fig. 1A).On sequencing the aberrant band (exon 17), a GGA to GTA mutation, resulting in glycine to valine substitution in codon 1137 was confirmed (Fig. 1B). The mutation was not detected in normal DNA from the same patient (Fig. 1B).
We also analyzed all the tumors for the changes in the number of MET allelic copies in gliomas by FISH using cosmid c182b3 containing MET gene. Three of 11 sporadic gliomas showed a deletion of one copy of the MET gene (Cases 3, 5, and 10), and a specific MET gene mutation in the remaining gene copy was detected in one of those tumors (Case 3). Three of 11 sporadic gliomas showed a duplication of one copy of the MET gene but none of them showed mutation (Cases 6, 7, and 8). One glioma (Case 11) showed MET amplification exhibiting 20 to 100 copies of MET signal in each affected cell. Three of 11 did not show either allelic change or mutation (Cases 1, 2, and 4). One of 11 (Case 9) was not analyzed because of the poor condition of the cell morphology in the touch preparation (Table 1).
DISCUSSION
Multiple mechanisms, such as gene mutations, amplifications, and rearrangements, as well as perturbed mitogen and receptor function, are likely to contribute to development of gliomas. Mutations in p53 (20), Rb (21), p16 (22), MMAC1 (23) and DCC (24) genes have been correlated with the initiation and progression of human gliomas. Amplification and/or activation of oncogenes, such as the genes for the epidermal growth factor receptor (25), transforming growth factor-α (26), MET (8), N-myc (5), c-myc (6), and gli (27) are thought to contribute to glioma formation by elevated expression of proteins that participate in mitogenic signalling pathways.
MET tyrosine kinase receptor, the product of the c-met proto-oncogene, has been implicated in a variety of human cancers. Chromosome 7 abnormalities in HPRC has shown that mutations of the MET gene (particularly in exons 17, 18, and 19) and nonrandom duplication of the mutant MET allele in the trisomy 7 found in HPRC appears to be a mechanism in human tumorigenesis related to MET (11, 16, 28).
Our data showed a missense mutation in 1 of 11 cases. The missense mutation in exon 17 (Case 3) is one of the most commonly mutated regions of the tyrosine kinase domain of MET. Mutation studies on known mutations identified in papillary renal carcinoma exhibited increased levels of tyrosine phosphorylation and enhanced kinase activity in response to exogenous ligands when compared with wild-type MET (29). Moreover, NIH 3T3 cells expressing mutant MET molecules formed foci in vitro and were tumorigenic in nude mice.
The tumors showing duplication involving the MET locus were high-grade tumors (i.e., GBMs) in our series. Although three cases with duplication of chromosome 7 did not reveal a mutant allele, MET amplification may be still associated with glioma formation, as shown in previous studies (8, 10).
The deletion of the MET locus on chromosome 7, as demonstrated by FISH data in the patient with a missense mutation (Case 3), may suggest the exclusive expression of the mutant allele by overrepresentation of the mutant allele (30) or loss of suppression effect of the wild-type allele, as shown in defective serine/threonine kinase gene (31).
Frequent allelic loss on chromosome 7q31 has been described for multiple cancers, including breast (32), gastric (33), and prostate (32) cancers. Likewise, allelic deletion without mutation of MET in our series may suggest the presence of a novel putative tumor suppressor gene at chromosome 7 near the MET locus, which may be involved in glioma formation.
This study represents the first investigation of the role of MET mutations and deletions in glioma tumorigenesis. Our results demonstrate that, although activating mutations are not common (1 of 11 tumors in this series), deletion, aneuploidy, and amplification of the MET gene are common (7 of 11 tumors) in tumor cells and may be a contributing factor in glioma formation, progression, or both. Furthermore, PCR-based allelic quantification, combined with FISH analysis, permits more sensitive analysis of the manner in which heterogenous alterations of the MET proto-oncogene may influence tumorigenesis.
Representative results of FISH in sporadic gliomas. Green signal, α-satellite centrometric marker; red signal, chromosome 7-specific cosmid probe containing MET gene (cosmid c182b3). A and B, interphase touch preparations of sporadic gliomas. A, allelic deletion of one copy of the MET gene detected in a sporadic glioma. B, sporadic glioma showing three copies of chromosome 7.
References
Russel DS, Rubinstein LJ . Tumors of central neuroepithelial origin. Pathology of tumors of the nervous system. 5th ed. Baltimore: Williams & Wilkins, 1989. p. 82–289.
Bigner SH, Mark J, Burger P, Mahaley MS Jr, Bullard DE, Muhlbaier LH, et al. Specific chromosomal abnormalities in malignant human gliomas. Cancer Res 1988; 48: 405–411.
Thiel G, Losanowa T, Kintzel D, Nisch G, Martin H, Vorpahl K, et al. Karyotypes in 90 human gliomas. Cancer Genet Cytogenet 1992; 58: 109–120.
Hecht BK, Turc-Carel C, Chatel M, Grellier P, Gioanni J, Attias R, et al. Cytogenetics of malignant gliomas: I. The autosomes with reference to rearrangements. Cancer Genet Cytogenet 1995; 84: 1–8.
Garson JA, McIntyre PG, Kemshead JT . N-myc amplification in malignant astrocytoma. Lancet 1985; 8457: 718–719.
Trent J, Meltzer P, Rosenblum M, Harsh G, Kinzler K, Mashal R, et al. Evidence for rearrangement, amplification, and expression of c-myc in a human glioblastoma. Proc Natl Acad Sci U S A 1986; 83: 470–473.
Reifenberger G, Reifenberger J, Ichimura K, Meltzer PS, Collins VP . Amplification of multiple genes from chromosomal region 12q31–14 in human malignant gliomas: preliminary mapping of the amplicons shows preferential involvement of CDK4, SAS, and MDM2. Cancer Res 1994; 54: 4299–4303.
Moriyama T, Kataoka H, Tsubouchi H, Koono M . Concomitant expression of hepatocyte growth factor (HGF), HGF activator and c-met genes in human glioma cells in vitro. FEBS Lett 1995; 372: 78–82.
Jeffers M, Rong S, Anver M, Vande Woude GF . Autocrine hepatocyte growth factor/scatter factor-Met signalling induces transformation and the invasive/metastatic phenotype in C127 cells. Oncogene 1996; 13: 853–861.
Rosen EM, Laterra J, Joseph A, Jin L, Fuchs A, Way D, et al. Scatter factor expression and regulation in human glial tumors. Int J Cancer 1996; 67: 248–255.
Schmidt L, Duh F-M, Chen F, Kishida T, Glenn G, Choyke P, et al. Nat Genet 1997; 16: 68–73.
Di Renzo MF, Narsimhan RP, Olivero M, Bretti S, Giordano S, Medico E, et al. Expression of the Met/HGF receptor in normal and neoplastic human tissues. Oncogene 1991; 6: 1997–2003.
Wullich B, Muller H-W, Fischer U, Zang KD, Meese E . Amplified met gene linked to double minutes in human glioblastoma. Eur J Cancer 1993; 29A: 1991–1995.
Nabeshima K, Shimao Y, Sato S, Kataoka H, Moriyama T, Kawano H, et al. Expression of c-Met correlates with grade of malignancy in human astrocytic tumours: an immunohistochemical study. Histopathology 1997; 31: 436–443.
Koochekpour S, Jeffers M, Rulong S, Taylor G, Klineberg E, Hudson EA, et al. Met and hepatocyte growth factor/scatter factor expression in human gliomas. Cancer Res 1997; 57: 5391–5398.
Schmidt L, Junker K, Weirich G, Glenn G, Choyke P, Lubensky IA, et al. Two North American families with hereditary papillary renal carcinoma and identical novel mutations in the MET proto-oncogene. Cancer Res 1998; 58: 1719–1722.
Zhuang Z, Bertheau P, Emmert-Buck MR, Liotta LA, Gnarra J, Linehan WM, et al. A microdissection technique for archival DNA analysis of specific cell populations in lesions < 1 mm in size. Am J Pathol 1995; 146: 620–625.
Orita M, Iwahana H, Kanazawa H, Hayashi K, Seikya T . Detection of polymorphisms of human DNA by gel electrophoresis as single-strand conformation polymorphisms. Proc Natl Acad Sci U S A 1989; 86: 2766–2770.
Pack S, Zbar B, Pak E, Ault DO, Humpherey JS, Pham T, et al. Constitutional VHL gene deletion in VHL families by fluorescence in situ hybridization (FISH). Cancer Res 1999; 5560–5564.
Mercer WE, Shields MT, Amin M, Sauve GJ, Appella E, Romano JW, et al. Negative growth regulation in a glioblastoma tumor cell line that conditionally express human wild-type p53. Proc Natl Acad Sci U S A 1990; 87: 6166–6170.
Henson JW, Schnitker BL, Correa KM, von Deimling A, Fassbender F, Xu HJ, et al. The retinoblastoma gene is involved in malignant progression of astrocytomas. Ann Neurol 1994; 36: 714–721.
Arap W, Nishikawa R, Furnari FB, Cavenee WK, Huang HJ . Replacement of the p16/CDKN2 gene suppresses human glioma cell growth. Cancer Res 1995; 55: 1351–1354.
Steck PA, Pershouse MA, Jasser SA, Yung WK, Lin H, Ligon AH, et al. Identification of a candidate tumour suppressor gene, MMAC1, at chromosome 10q22.3 that is mutated in multiple advanced cancers. Nat Genet 1997; 15: 356–362.
Ekstrand BC, Mansfield TA, Bigner SH, Fearon ER . DCC expression is altered by multiple mechanisms in brain tumours. Oncogene 1995; 11: 2393–2402.
Wong AJ, Bigner SH, Bigner DD, Kinzler KW, Hamilton SR, Vogelstein B . Structural alterations of the epidermal growth factor receptor gene in human gliomas. Proc Natl Acad Sci U S A 1993; 84: 6869–6873.
Ekstrand AJ, James CD, Cavenee WK, Seliger B, Pettersson RF, Collins VP . Genes for epidermal growth factor receptor, transforming growth factor alpha, and epidermal growth factor and their expression in human gliomas in vivo. Cancer Res 1991; 51: 2164–2172.
Kinzler KW, Ruppert JM, Bigner SH, Vogelstein B . The GLI gene is a member of the Kruppel family of zinc finger proteins. Nature 1988; 332: 371–374.
Zhuang Z, Park W-S, Pack SD, Schmidt L, Vortmeyer AO, Pak E, et al. Trisomy 7-harbouring non-random duplication of the mutant MET allele in hereditary papillary renal carcinomas. Nat Genet 1998; 20: 66–69.
Jeffers M, Schmidt L, Nakaigawa N, Webb CP, Weirich G, Kishida T, et al. Activating mutations for the met tyrosine kinase receptor in human cancer. Proc Natl Acad Sci U S A 1997; 94: 11445–11450.
Bianchi AB, Aldaz CM, Conti CJ . Nonrandom duplication of the chromosome bearing a mutated Ha-ras-1 allele in mouse skin tumors. Proc Natl Acad Sci U S A 1990; 87: 6902–6906.
Hemminki A, Markie D, Tomlinson I, Avizienyte E, Roth S, Loukola A, et al. A serine/threonine kinase gene defective in Peutz-Jeghers syndrome. Nature 1998; 391: 184–187.
Zenklusen JC, Thompson JC, Troncoso P, Kagan J, Conti CJ . Loss of heterozygosity in human primary prostate carcinomas: a possible tumor suppressor gene at 7q31.1. Cancer Res 1994; 54: 6370–6373.
Kuniyasu H, Yasui W, Yokozaki H, Akagi M, Akama Y, Kitahara K, et al. Frequent loss of heterozygosity of the long arm of chromosome 7 is closely associated with progression of human gastric carcinomas. Int J Cancer 1994; 59: 597–600.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Moon, YW., Weil, R., Pack, S. et al. Missense Mutation of the MET Gene Detected in Human Glioma. Mod Pathol 13, 973–977 (2000). https://doi.org/10.1038/modpathol.3880177
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.3880177
Keywords
This article is cited by
-
MET in glioma: signaling pathways and targeted therapies
Journal of Experimental & Clinical Cancer Research (2019)
-
MET: a promising anticancer therapeutic target
Nature Reviews Clinical Oncology (2012)