Abstract
No previous reports on lymph-node metastasis (LNM) from superficial squamous cell carcinoma of the esophagus have proposed definite criteria for additional treatment after endoscopic mucosal resection (EMR). We investigated the association between histopathological factors and LNM in 464 consecutive patients with superficial squamous cell carcinoma of the esophagus who had undergone a radical esophagectomy with lymph-node dissection (14 ‘M1’ lesions: intraepithelial tumors, 36 ‘M2’ lesions: tumors invading the lamina propria, 50 ‘M3’ lesions: tumors in contact with or invading the muscularis mucosa, 32 ‘SM1’ lesions: tumors invading the most superficial 1/3 of the submucosa and 332 ‘SM2/3’ lesions: tumors invading deeper than SM1 level). Histopathological factors including invasion depth, size, lymphatic invasion (LY), venous invasion, tumor differentiation, growth pattern, degree of nuclear atypia and histological grade were assessed for their association with LNM in 82 M3 or SM1 lesions to determine which patients need additional treatment after EMR. LNM was found in 0.0, 5.6, 18.0, 53.1 and 53.9% of the M1, M2, M3, SM1 and SM2/3 lesions, respectively. A univariate analysis showed that each of the following histopathological factors had a significant influence on LNM: invasion depth (M3 vs SM1), LY, venous invasion and histological grade. Invasion depth and LY were significantly associated with LNM in a multivariate analysis. Four out of 38 patients (10.3%) with M3 lesions without LY had LNM, whereas five out of 12 patients (41.7%) with M3 lesions and LY had LNM. Only patients with M1/2 lesions are good candidates for EMR. Invading the muscularis mucosa (M3) is a high-risk condition for LNM the same as submucosal invasion, but M3 lesions without LY can be followed up after EMR without any additional treatment.
Similar content being viewed by others
Main
The proportion of patients with superficial squamous cell carcinoma of the esophagus (SSCCE) and lymph-node metastasis (LNM) has been reported to be 26–53%, whereas the proportion of SSCCE patients with intraepithelial carcinoma or carcinoma invading the lamina propiria and LNM is only 0–5%.1, 2, 3, 4, 5, 6 Consequently, intraepithelial carcinoma or carcinoma invading the lamina propria is generally treated by endoscopic mucosal resection (EMR).1, 2, 3, 4, 5, 6 Radical esophagectomy with lymph-node dissection is still regarded as an invasive treatment, given the high operative mortality and morbidity rates.6, 7, 8, 9, 10, 11 In addition, the poor quality of life of patients after such aggressive surgery prompted us to search for expanded indications for EMR. No previous reports, however, have proposed definite criteria for additional treatment after EMR in patients with SSCCE because of the small number of cases in these studies, inconsistent methods of lymph-node dissection, inconsistent evaluations of invasion depth or inconsistent histological typing, including not only squamous cell carcinoma but also adenocarcinoma.1, 2, 3, 4, 6
We previously evaluated a total of 240 patients with SSCCE, including 20 patients with ‘M3’ lesions (ie tumors in contact with or invading the muscularis mucosa) and 166 patients with ‘SM’ lesions (ie tumors invading the submucosa) to clarify the association between histopathological findings and LNM.3 Lymphatic invasion (LY) was significantly associated with LNM in a multivariate analysis, and LY and histological grade (HG) were found to be prognostic factors in patients with SSCCE. Furthermore, none of the 21 lesions with HG1/2 and a vertical tumor invasion depth from the muscularis mucosa (VTID) of <200 μm without LY or venous invasion (V) had LNM. Therefore, our previous study concluded that those 21 lesions could be treated by EMR.
In this study, we reanalyzed the histopathological features of patients with SSCCE to investigate whether histopathological criteria for additional treatment after EMR could be determined based on associations between histopathological findings and LNM in a larger population of patients with SSCCE. We especially focused on minimally invasive lesions such as M3 and SM1 lesions, which can be resected by EMR without leaving any cancer tissue in the esophagus.
Materials and methods
Patients
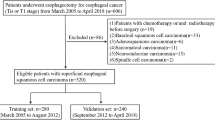
Our series consisted of 464 consecutive patients who had undergone a radical esophagectomy with lymphadenectomy, either thoraco-abdominal (two-field) or cervico-thoraco-abdominal (three-field), for the treatment of SSCCE at the National Cancer Center Hospital in Tokyo, Japan, between January 1980 and October 2004. The histopathological features of 255 of these patients were reported in our previous report.3 No preoperative radiotherapy, chemotherapy or EMR was performed in the present series. The patients comprised 415 (89.4%) men and 49 (10.6%) women. The mean age was 61.7 years (range: 40–86 years). We classified the SSCCE lesions based on the invasion depth as follows: ‘M1’ for intraepithelial carcinomas; ‘M2’ for tumors invading the lamina propria; ‘M3’ for tumors in contact with or invading the muscularis mucosa; ‘SM1’ for tumors invading the most superficial 1/3 of the submucosa; and ‘SM2/3’ for tumors invading deeper than the SM1 level (Figure 1). The association between LNM and clinical outcome was examined in each group. In addition, the histopathological findings described below were analyzed using 82 M3 or SM1 lesions to determine which patients required additional treatment after EMR. When a patient had multicentric esophageal carcinomas, the histopathological factors for the lesion with the greatest invasion depth were evaluated.
Subdivision of superficial esophageal carcinoma according to depth of invasion. M1: intraepithelial tumors; M2: tumors invading the lamina propria; M3: tumors in contact with or invading the muscularis mucosa; SM1: tumors invading the most superficial 1/3 of the submucosa; SM2/3: tumors invading deeper than the SM1 level.
Histopathological Review
Serial 5-mm-thick tissue sections of the entire lesion were cut from resected specimens fixed with 10% buffered formalin, embedded in paraffin and stained with hematoxylin and eosin using standard methods. The invasion depth- VTID, tumor size, LY, V, LNM, tumor differentiation, growth pattern, degree of nuclear atypia and HG3 were histopathologically evaluated. The distance from the invasive front to the muscularis mucosa was measured using microscopy with an ocular lens scale and defined as VTID. In specimens where the muscularis mucosa was disrupted by ulceration or tumor invasion, the muscularis mucosa level was estimated by drawing a line to connect the remaining muscularis mucosa. Tumor differentiation was assessed according to the World Health Organization classification.12 The degree of nuclear atypia was classified as low (sharp nuclei of uniform size with homogeneous chromatin: one point) or high (polymorphic nuclei with vesicular or dot-like chromatin: two points). The growth pattern was classified as expansive (large solid nests with a clear tumor margin: one point) or infiltrative (small nests and dissociated cells with an unclear tumor margin: two points). The degree of nuclear atypia and growth pattern were evaluated at the deepest area of the invading tumor. The HG of each tumor was calculated in the same manner as in our previous report by adding the nuclear atypia and growth pattern scores to obtain Grade 1: two points; Grade 2: three points; or Grade 3: four points.3 Independent histopathological reviews were performed by two experienced pathologists (YN and TS) who had no prior knowledge of the clinical outcomes of the patients. Their results were compared, and any discrepancies were resolved by consensus at a meeting following a further histopathological review.
Statistical Analysis
An unconditional logistic regression analysis was performed using the SAS LOGISTIC procedure (SAS Institute Inc., Cary, NC, USA) to examine the association between the histopathological factors and LNM. All P-values were two-sided, and the significance level was set at P<0.05.
Results
Clinicopathological Features Based on Invasion Depth
LNM was found in none of 14 patients with M1 lesions, two of the 36 patients (5.6%) with M2 lesions, nine of the 50 patients (18.0%) with M3 lesions, 17 of the 32 patients (53.1%) with SM1 lesions and 179 of the 332 patients (53.9%) with SM2/3 lesions. The number of dissected lymph nodes in each case was 48±21 (mean±standard deviation). None of the patients with M1, M2, M3 or SM1 lesions died of esophageal carcinoma, whereas 63 patients (40.7%) with SM2/3 lesions died from their primary disease. Six of the 464 patients (0.2%) died within 1 month of surgery owing to surgical complications. The median follow-up duration was 4.2 years (range: 2 days–23.5 years).
Clinical Characteristics of 82 Patients with M3 and SM1 Lesions
The clinical characteristics of 82 patients with M3 and SM1 lesions are shown in Table 1. Multicentric synchronous esophageal carcinomas were found in 30 patients (36.6%), whereas 28 patients (34.2%) had synchronous or metachronous multiple malignancies in other organs. The VTID was 130±106 μm (mean±standard deviation) for the SM1 lesions.
Relationships between Histopathological Findings and Lymph-Node Metastasis in Patients with M3 and SM1 Lesions
The relationships between the histopathological findings and LNM in 82 patients with M3 and SM1 lesions were determined using a univariate analysis and are shown in Table 2. The univariate analysis showed that each of the following histopathological factors had a significant influence on LNM: invasion depth (M3 vs SM1), LY, V and HG (odds ratios (OR)=5.16, 4.60, 10.0 and 3.76, respectively). A multivariate analysis revealed that only invasion depth and LY were independently correlated with LNM (OR=4.71 and 3.83, respectively; 95% confidence interval=1.55–14.3 and 1.18–12.4, respectively) (Table 3). Four patients out of a total of 38 patients (10.3%) with M3 lesions but without LY had LNM, whereas five out of 12 patients (41.7%) with M3 lesions and LY had LNM. Six patients out of a total of 21 patients (28.6%) with SM1 lesions but without LY had LNM, whereas all the 11 patients (100%) with SM1 lesions and LY had LNM (Table 4).
Discussion
LNM was observed in 0.0% of patients with M1 lesions, 5.6% of patients with M2 lesions, 18.0% of patients with M3 lesions, 53.1% of patients with SM1 lesions and 53.9% of patients with SM2/3 lesions. As 96% of patients with M1/2 lesions developed no LNM, EMR alone can be a definitive treatment for patients with M1 and M2 lesions, taking into account the operative mortality, morbidity and poor quality of life after surgery.6, 7, 8, 9, 10, 11 In contrast, more than half of the patients with SM1 or SM2/3 lesions developed LNM; therefore, these patients should receive additional systemic treatments after EMR. The proportion of patients with M3 lesions who developed LNM was not negligible; therefore, we tried to determine any associations in the histopathological features of M3 lesions and LNM. Invasion depth (M3 vs SM1) and LY were significantly associated with LNM in a multivariate analysis (OR=4.71 and 3.83, respectively; 95% confidence interval=1.55–14.3 and 1.18–12.4, respectively). Because LY might be a predictive factor for LNM, LY should be precisely examined in resected specimens. Almost half of the patients with M3 lesions and LY had LNM; therefore, these lesions should be treated as a systemic disease, like SM lesions. Regarding the M3 lesions without LY, LNM was found in 10.3% of the patients (four out of 38 cases). Patients with M3 lesions without LY should decide whether they won't undergo additional treatment after EMR or they will undergo additional systemic treatments such as esophagectomy or chemo-radiation therapy after EMR, considering the possibility of LNM and the invasiveness of systemic therapy, after receiving a thorough explanation of the possibility of LNM and the invasiveness of systemic therapy and providing their informed consent. Although we tried to find patients who did not require additional systemic treatment after EMR for SM1 lesions in order to expand the current criteria for EMR, rather limited criteria were established based on the results of the present study. In this study, we examined a large number of patients with SSCCE who had been treated using the same approach (esophagectomy with two- or three-field lymph-node dissection) and whose resected specimens had been examined in the same manner. Thus, the present study provides reliable data concerning LNM in patients with SSCCE treated at a single institution.
In the present analysis, the proportions of patients with LNM in each group were higher than those reported in previous reports.1, 2, 3, 4, 5, 6 This discrepancy might be explained by the fact that all the patients in the present study underwent a radical esophagectomy with two- or three-field lymph-node dissection, resulting in the sampling of a large number of lymph nodes: 48±21 (mean±standard deviation). The number of dissected lymph nodes was not reported in most of the previous reports1, 2, 3, 4, 5 except for one, in which the mean number of examined lymph nodes was 14.1.6 Thus, a precise comparison with previous reports is not feasible, as the number of examined lymph nodes differed. On the other hand, it is unlikely that patients preoperatively diagnosed as having LNM would be more likely to participate in the present analysis, as an esophagectomy with two- or three-field lymph-node dissection was performed regardless of the LNM diagnosis if surgery was selected for the treatment of SSCCE at our institution.13, 14
In 2000, we previously reported the results of uni- and multivariate analyses to identify histopathological factors associated with LNM in 186 patients with M3 or SM lesions who underwent an esophagectomy and a two- or three-field lymph-node dissection. Only LY was independently associated with LNM in the multivariate analysis, and LY and HG were found to be significant prognostic factors in patients with SSCCE. None of the 21 patients with HG 1/2 and a VTID from the muscularis mucosa of <200 μm without LY or V had LNM. LY, VTID and HG, therefore, were reported to be important factors for identifying patients who did not require additional systemic treatment after EMR. In the present study, in which almost twice the number of cases was examined, LY was confirmed to be independently associated with LNM in patients with M3 and SM1 lesions. In addition, the depth of invasion (M3 vs SM1) turned out to be a significant factor for predicting LNM. We also classified the cases with M3 and SM1 lesions based on VTID, according to the method used in our previous report, but VTID was not significantly associated with LNM in this study.
In conclusion, we propose that SM lesions should be treated as a systemic disease. Only patients with M1/2 lesions are good candidates for EMR. M3 lesions with LY should be treated in the same way as SM lesions because M3 lesions with LY were associated with LNM.
References
Kodama M, Kakegawa T . Treatment of superficial cancer of the esophagus: a summary of responses to a questionnaire on superficial cancer of the esophagus in Japan. Surgery 1998;123:432–439.
Nabeya K, Nakata Y . Extent of resection and lymphadenectomy in early squamous cell esophageal cancer. Dis Esophagus 1997;10:159–161.
Tajima Y, Nakanishi Y, Ochiai A, et al. Histopathologic findings predicting lymph node metastasis and prognosis of patients with superficial esophageal carcinoma: analysis of 240 surgically resected tumors. Cancer 2000;88:1285–1293.
Fujita H, Sueyoshi S, Yamana H, et al. Optimum treatment strategy for superficial esophageal cancer: endoscopic mucosal resection vs radical esophagectomy. World J Surg 2001;25:424–431.
Shiozaki H, Doki Y, Yamana H, et al. A multi-institutional study of immunohistochemical investigation for the roles of cyclin D1 and E-cadherin in superficial squamous cell carcinoma of the esophagus. J Surg Oncol 2002;79:166–173.
Bogomoletz WV, Molas G, Gayet B, et al. Superficial squamous cell carcinoma of the esophagus. A report of 76 cases and review of the literature. Am J Surg Pathol 1989;13:535–546.
Sugimachi K, Ohno S, Matsuda H, et al. Clinicopathologic study of early stage esophageal carcinoma. Br J Surg 1989;76:759–763.
Bonavina L . Early oesophageal cancer: results of a European multicentre survey. Group Europeen pour l'Etude des Maladies de l'Oesophage. Br J Surg 1995;82:98–101.
Altorki NK, Skinner DB . Occult cervical nodal metastasis in esophageal cancer: preliminary results of three-field lymphadenectomy. J Thorac Cardiovasc Surg 1997;113:540–544.
Kato H, Tachimori Y, Watanabe H, et al. Superficial esophageal carcinoma. Surgical treatment and the results. Cancer 1990;66:2319–2323.
Matsubara T, Ueda M, Abe T, et al. Unique distribution patterns of metastatic lymph nodes in patients with superficial carcinoma of the thoracic oesophagus. Br J Surg 1999;86:669–673.
Travis WD, Brambilla E, Konrad Muller-Hermelink H, et al. World Health Organization Classification of Tumours. IARC Press: Lyon, 2000.
Igaki H, Kato H, Tachimori Y, et al. Clinicopathologic characteristics and survival of patients with clinical Stage I squamous cell carcinomas of the thoracic esophagus treated with three-field lymph node dissection. Eur J Cardiothorac Surg 2001;20:1089–1094.
Kato H, Tachimori Y, Mizobuchi S, et al. Cervical, mediastinal, and abdominal lymph node dissection (three-field dissection) for superficial carcinoma of the thoracic esophagus. Cancer 1993;72:2879–2882.
Acknowledgements
We thank Dr Sandy Dawsey, National Institute of Health, Bethesda, MD, for his helpful comments on this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Duality of interest
We have no duality of interest to declare.
Rights and permissions
About this article
Cite this article
Eguchi, T., Nakanishi, Y., Shimoda, T. et al. Histopathological criteria for additional treatment after endoscopic mucosal resection for esophageal cancer: analysis of 464 surgically resected cases. Mod Pathol 19, 475–480 (2006). https://doi.org/10.1038/modpathol.3800557
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.3800557
Keywords
This article is cited by
-
Porphyromonas gingivalis predicts local recurrence after endoscopic submucosal dissection of early esophageal squamous cell carcinoma or precancerous lesion
BMC Cancer (2023)
-
Clinical Outcomes of Follow-Up Observation After Endoscopic Submucosal Dissection for Esophageal Squamous Cell Carcinoma Invading the Muscularis Mucosa Without Lymphovascular Involvement
Digestive Diseases and Sciences (2023)
-
Long-term clinical outcomes of patients diagnosed with pT1a-muscularis mucosae with lymphovascular invasion or pT1b after endoscopic resection for cT1N0M0 esophageal squamous cell carcinoma
Esophagus (2022)
-
A prospective multicenter study of the magnifying endoscopic evaluation of the invasion depth of superficial esophageal cancers
Surgical Endoscopy (2022)
-
Long-term outcomes of endoscopic submucosal dissection for superficial esophageal squamous cell carcinoma in Taiwan
BMC Gastroenterology (2021)