Abstract
Diagnosis of infections caused by mycobacteria, especially nontuberculous mycobacteria still represents a difficult task both in microbiology and pathology. The aim of this study was to determine the frequency of mycobacterial DNA detectable by PCR in formalin-fixed paraffin-embedded tissues showing suspicious granulomatous lesions. A total of 190 archival specimens were analyzed, using a nested PCR protocol, which amplifies a fragment of the mycobacterial 65-kDa heat-shock protein gene. Restriction fragment-length polymorphisms and sequencing were utilized to further analyze the obtained PCR products. Corresponding microbiological culture results were available for 41 cases. We detected mycobacterial DNA in 119 cases (63%), of which 71 (60%) were positive for Mycobacterium tuberculosis complex DNA and 41 (34%) for DNA of nontuberculous mycobacteria. Seven cases (6%) could not be subtyped for technical reasons. The largest group of nontuberculous mycobacteria comprised 29 cases (25% of the 119 positive cases), which were assigned to Mycobacterium fortuitum complex. Mycobacterium avium–intracellulare complex was detected in eight (7%) cases, Mycobacterium gordonae in three (2.5%) and Mycobacterium rhodesiae in a single case (0.8%). All cases of Mycobacterium tuberculosis were unequivocally identified by restriction fragment-length polymorphism analysis. In contrast, sequencing provided a gain of information over restriction fragment-length polymorphism analysis in 37% of the nontuberculous mycobacteria cases (15 of 41). Alignment studies on DNA of nontuberculous mycobacteria showed frequent sequence variations, supporting the existence of sequevars. Comparison of molecular data to available results of microbiological culture assays showed a good concordance of 83%. In conclusion, amplification and sequencing of the mycobacterial 65-kDa heat-shock protein gene is an excellent tool for species identification of mycobacteria, especially nontuberculous mycobacteria, in formalin-fixed paraffin-embedded tissues.
Similar content being viewed by others
Main
The diagnosis of mycobacterial infections in archival pathological specimens still represents a challenge. This is especially true for infections caused by nontuberculous mycobacteria, which frequently show nonspecific clinical symptoms.1, 2 Furthermore, microbiological culture assays can have a fairly low sensitivity in nontuberculous mycobacteria especially in the setting of cervical lymphadenitis, where detection rates are between 50 and 60%.3 Morphologically, caseating and noncaseating granulomatous reactions can occur, which often do not allow a differentiation between various infectious etiologies and hypersensitivity reactions. Stains for acid-fast bacilli remain frequently negative.4
In order to improve the diagnostic sensitivity, many different PCR protocols have been developed for amplification of mycobacterial DNA. Only some of them are suitable for routine application on formalin-fixed paraffin-embedded material.5, 6, 7, 8, 9, 10, 11 and only few PCR protocols are able to amplify hypervariable gene regions, necessary for identification of nontuberculous mycobacteria. One of the protocols that fulfills these requirements was published by Cook et al.5 This method amplifies a short fragment (133 bp) of the hypervariable region, that belongs to the 65-kDa heat-shock protein gene (hsp65).12, 13
The aim of this study was to test the suitability of this protocol for the detection of mycobacterial DNA, especially of nontuberculous mycobacteria in archival pathological specimens with suspicious granulomatous reactions and to analyze the distribution of mycobacterial species. Furthermore, we compared the specificity of restriction fragment-length polymorphism analysis (RLFP) with sequencing for nontuberculous mycobacteria speciation.
Materials and methods
Materials
Our collection consisted of formalin-fixed and paraffin-embedded material of 190 cases diagnosed histologically as granulomatous reactions suspicious for possible mycobacterial infection, which had been collected over a period of 3 years (1998–2000). The samples originated from a variety of anatomical sites such as respiratory tract, lymph nodes, gastrointestinal tract, genitourinary tract, bone, skin and other miscellaneous localizations (Table 1). Histologically, 61 cases (32%) showed well-defined granulomas with caseation necrosis, 66 cases (35%) well-defined granulomas without caseation necrosis and 63 cases (33%) ill-defined granulomas, including 26 pyogranulomas, and three spindle cell pseudotumors. Majority of specimens were submitted by outside pathologists for consultation. Cases with a history or clinical diagnosis of sarcoidosis, necrotizing sarcoidal granulomatosis, Crohn's disease, Wegener's disease and other variants of arteritis were excluded from this study (n=9). Analysis of stains for acid-fast bacilli as well as standard morphological analysis were performed independently by two pathologists.
Organism controls consisted of DNA extracts of the following cultured mycobacterial strains obtained from the American-type culture collection (ATCC): Mycobacterium tuberculosis, Mycobacterium gordonae, Mycobacterium fortuitum, Mycobacterium avium, Mycobacterium intracellulare, Mycobacterium chelonae
DNA Extraction
Deparaffinization was performed with xylene and ethanol on serial sections of 40–60 μm in total, depending on the amount of tissue. To avoid contamination of the samples during the preparation process, new disposable microtome blades were used for each sample, and the microtome was cleaned meticulously after each block. After lyophilization the probes were resuspended in 50 μl of 50 mM Tris 8.3 with 200 μg/ml proteinase K and incubated overnight at 37°C.5, 6 A modified temperature step model was used before and after proteinase K digestion three times each (2 min at 37°C, 30 s vortexing, 2 min at −80°C) to disrupt mycobacterial cell walls.14
Nested PCR and RFLP Analysis
After pelleting of insoluble debris by centrifugation, DNA integrity was tested by amplification of a 269 bp fragment of the β-globin gene (as housekeeping gene) in a single step PCR (35 cycles).15 All cases, which showed negative or weak results in β-globin amplifications due to poor DNA quality, were excluded from further analysis (n=7). PCR for the detection of mycobacterial DNA was performed using the primer combinations described by Cook et al,5 which amplify a fragment of the mycobacterial 65-kDa heat shock protein gene (hsp65). A measure of 5 and 0.5 μl of the DNA extract (soluble phase) was put as template in the first-round PCR reaction mix (50 μl total volume, containing 200 μM of each dNTP, 2.5 ng/μl of each primer, 1 U Taq polymerase and 1 × Taq polymerase buffer). The PCR protocol consisted of an initial denaturation (7 min, 94°C), 35 cycles (1 min at 94°C, 2 min at 57°C, 2 min at 72°C) and a final extension step of 7 min (72°C). For nested reamplification, 5 and 0.5 μl of first-round PCR product were transferred and subjected to the same PCR conditions (35 cycles). Cases positive for M. tuberculosis DNA in the hsp65 PCR but negative in microbiological cultures were confirmed with an additional single step PCR, specific for M. tuberculosis complex. It amplifies a sequence of 123 bp of the insertion sequence IS6110 by using a single-step approach (40 cycles).8 As positive control, we used DNA of M. tuberculosis (H37Rv). The negative controls consisted of template-free reaction mix with deionized water. Furthermore, we used normal formalin-fixed paraffin-embedded material tissues from lung (2 ×), lymph nodes (2 ×), soft tissue (2 ×), kidney (2 ×), liver (1 ×) and bone (1 ×) as negative tissue controls. PCR products were visualized by agarose gel electrophoresis. RFLP analysis of the hsp65 PCR products for identification of mycobacterial species was performed using three different endonucleases (HhaI, BstUI, MboI), according to the published protocol.5 Fragment sizes were estimated by comparison with the DNA size marker (Hae3 digest of Phi × 174).5
Sequencing Analysis and Homology Matches
All PCR products with restriction patterns other than M. tuberculosis were purified (QiaQuick Gel extraction kit, Qiagen, Hilden, Germany) and directly sequenced, using the fluorescence-based cycle sequencing procedure.16 Sequence analysis was performed on an automated sequencer (ABI prism 377™, Perkin-Elmer). For homology matches, we used the BLAST search program and the NCBI database. Multiple alignment studies and restriction site analysis were performed using the DNASIS™ software (Hitachi Softw. Eng.) and hsp65 sequences of the following reference strains (gi and gb accession numbers from BLAST search program, other designations are shown in parentheses): M. chelonae gi 4093110 (IP 140420003T, ATCC 35752T), M. fortuitum gi 4093116 (IP 140410001T, ATCC 6841T), Mycobacterium mucogenicum gi 4093120 (IP 140430001T, ATCC 49650T), Mycobacterium peregrinum gi 4093122 (IP 14041002T, ATCC 14467T), M. avium gi 2108161 (gb U 85641), M. intracellulare gi 19070717 (gb/AF 354277, strain 950A-9), M. gordonae gi 4093118 (gb/AF 071134, IP 14021001T), Mycobacterium rhodesiae gi 13560193 (emb/AJ 30764.1, MRH 307647).
Detection of Mycobacteria in Clinical Samples Via Culture
Clinical samples were incubated for 25 min in decontamination solution (sodium citrate solution 1.55% (w/v) containing N-acetyl-L-cysteine 0.005% (w/v) and NaOH 2% (v/v)) to remove any contaminating bacteria. Subsequently, the specimens were cultured on two different solid media (BBL™ Löwenstein–Jensen Medium+PACT (cat # 220502, Becton Dickinson, Loveton Circle, USA), BBL™ Stonebrink TB Medium+PACT (cat # 220505, Becton Dickinson)) as well as one liquid medium (BACTEC™ 12B MYCOBACTERIA CULTURE VIALS Middlebrook 7H12 (cat # 442004, Becton Dickinson). Samples were incubated until the culture yielded growing mycobacteria or were discarded as negative after 6 weeks.
Results
A total of 190 cases were analyzed. Corresponding microbiological culture data were available for 41 (21.6%) cases. Therefore, samples with available culture results (group 1) and without microbiological data (group 2) were analyzed separately. Overall, a total of 119 (63%) cases were positive for mycobacterial DNA, including 25/41 (61%) cases of group 1 and 94/149 (63%) of group 2. Concordant molecular and microbiological results were found in 83% (34/41 cases) of group 1, including 16 cases positive for M. tuberculosis, two positive for M. avium–intracellulare and 16 negative cases (Table 2). Discrepant results occurred in 17% (7/41 cases), including three positive PCR results for M. tuberculosis complex DNA and four positive PCR results for M. fortuitum complex DNA, whereas corresponding microbiological culture assays remained negative. All three cases of M. tuberculosis with negative cultures were validated independently by positive results obtained in a separate PCR assay for the M. tuberculosis complex-specific insertion sequence (IS 6110).8
All 119 positive PCR products were subjected to RFLP analysis. In all, 71 cases (60% of the positive cases) showed the typical restriction pattern for M. tuberculosis complex (Table 1).5 This was confirmed by sequencing of the PCR product in 15 cases. All of them showed 100% homology to M. tuberculosis (data not shown). Eight patients positive for M. tuberculosis had a history of immunosuppression, including five with HIV infection. Two patients had received intravesical BCG therapy for urothelial carcinoma, and a positive PCR result was obtained from bladder biopsies. Seven patients had a confirmed history of tuberculosis, and in the majority of the remaining cases, there was a high clinical suspicion of tuberculosis.
DNA of nontuberculous mycobacteria was found in 41 cases (34% of 119 positive cases, Table 1). Sequencing and BLAST homology search assigned the nontuberculous mycobacteria cases to M. fortuitum complex in 25% (30/119), including M. chelonae, M. fortuitum, M. mucogenicum and M. peregrinum.6 The second largest group of nontuberculous mycobacteria belonged to M. avium–intracellulare complex (6.7%). DNA of M. gordonae was found in three cases (2.5%) and of M. rhodesiae in a single case (0.8%, Table 3).
In contrast to M. tuberculosis, species identification was not possible by RFLP analysis in 15 (36.5%) of nontuberculous mycobacteria cases. The range of different restriction patterns for members of the M. fortuitum complex was fairly wide. We observed three different patterns for M. chelonae, two of which had been reported previously (data not shown).2, 5 Accordingly, sequences from different M. chelonae isolates varied at 1–5 nucleotides (Table 4).
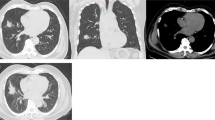
In addition, a new conserved restriction pattern specific for M. mucogenicum was identified in eight cases (Figure 1a, b). This subspecies had not been considered in the work of Cook et al.5 Homology matches of the sequenced PCR products (NCBI database) demonstrated a concordance of 93–100% with the reference sequence of M. mucogenicum (Table 4). Multiple alignments demonstrated sequence variants (sequevars) showing a divergence in up to 7 bp of the eight M. mucogenicum cases. Despite the existence of sequevars, species identification by RFLP was possible in all of the M. mucogenicum cases, since restriction sites were conserved.
(a) A new restriction pattern for M. mucogenicum was observed by using RFLP on PCR products (hsp65 amplification) in eight cases. The agarose gel shows a comparison of the specific restriction pattern found for DNA of M. mucogenicum to the restriction pattern of control DNA derived from M. tuberculosis complex. Sizes of restriction fragments of M. mucogenicum: H: 133 bp (uncut), b: 124+9 bp, M: 85+31+18 bp. SM, size marker (Hae3 digest of Phi × 174). Restriction enzymes: H, HhaI; B, BstuI; M, MboI. (b) Conserved DNA sequence of the amplified hsp65 fragment of M. mucogenicum, which was found in three of eight cases (Table 4). Restriction sites are indicated in triangles, primer binding sites are shown in italics.
Five of eight cases with DNA of M. avium–intracellulare complex showed the previously reported restriction patterns.5 The remaining three cases, which could not be clearly distinguished by RFLP, showed a stronger intraspecies divergence from to the M. avium reference sequence (Tables 4 and 5). Two of the eight M. avium–intracellulare infections had developed in the setting of HIV infection. The advantage of sequencing analysis over RFLP was most obvious for M. peregrinum and M. rhodesiae, which could only be specified via sequencing (Tables 4 and 5). Despite repeated DNA extraction, seven of the 119 cases (6%) showed only weak, although reproducible PCR products unsuitable for subtype identification by sequencing or RFLP (Table 1). Negative controls as well as negative tissue controls remained completely and reproducibly negative in the hsp65 PCR.
Correlation of histomorphology with molecular results showed that only the characteristic finding of spindle cell pseudotumors in HIV infection (two cases) allowed to confidently predict an infection with M. avium–intracellulare. Furthermore, a fairly good correlation of 79% (48 of 61 cases) existed between the presence of well-defined caseating granulomas and the detection of M. tuberculosis complex DNA. Nevertheless, three of these well-defined granulomas turned out to be positive for DNA of nontuberculous mycobacteria (2 × M. fortuitum complex, 1 × M. avium–intracellulare complex), whereas nine cases were completely negative for mycobacterial DNA.
As expected, staining for acid-fast bacilli was of limited value. Only four out of 41 nontuberculous mycobacteria cases were positive, all of them caused by M. avium–intracellulare complex, either showing the morphology of spindle cell pseudotumors (three cases) or ill-defined granulomas with microabcess formation (one case). Acid-fast bacteria were found in 7/16 cases positive for M. tuberculosis by both PCR and microbiological culture assays.
Discussion
The diagnosis of mycobacterial infections still presents a frequently difficult task in clinical and pathological practice. This is especially true for nontuberculous mycobacteria infections, which usually lack both specific clinical symptoms and defining morphological features. The pathological changes, frequently ill-defined granulomas or pyogranulomas with a lack of caseation, few or no giant cells and a negativity for acid-fast bacteria in staining procedures may lead to a suspicion of nontuberculous mycobacteria infection, but usually are nonspecific.3, 4 Nowadays, molecular techniques allow the species identification of mycobacteria even in samples where culture methods and other conventional detection methods have either not been employed or remained negative.3, 4 The application of PCR techniques has demonstrated that the frequency of infections by nontuberculous mycobacteria has probably been underestimated in the past and that the clinical and morphological spectrum of these infections is broader than previously thought.17, 18, 19, 20, 21, 22 This is confirmed by our study, which identified nontuberculous mycobacteria species in a third of the cases of suspicious granulomatous tissue reactions positive for mycobacterial DNA, using a sensitive nested PCR technique amplifying a hypervariable fragment of the hsp65 gene.5
The only specific histological pattern in our study, which allowed confident identification of the causative organism on morphological grounds alone corresponded to the well-recognized spindle cell pseudotumor in the setting of HIV infection. The two cases showed abundant intracellular acid-fast bacilli and were positive for DNA of M. avium–intracellulare complex. The remaining 38 nontuberculous mycobacteria cases (93%) could not be linked to a specific histomorphologic pattern.
PCR-based detection of mycobacterial DNA offers significant diagnostic support in these cases. In our laboratory, the protocol of Cook et al5 proved to be a highly sensitive method for detecting DNA of nontuberculous mycobacteria in routinely fixed, paraffin-embedded specimens.2 In addition to identifying nontuberculous mycobacteria infections, this protocol is also a convenient way of testing for M. tuberculosis. In contrast to nontuberculous mycobacteria species, M. tuberculosis showed a 100% conservation of its characteristic RFLP pattern and complete sequence homology to the reference strain in all analyzed cases, confirming that our protocol in conjunction with RFLP is of equal specificity as PCR protocols amplifying only M.tuberculosis-specific sequences. We observed DNA of M. tuberculosis complex in 60% and DNA of nontuberculous mycobacteria in 34% of the cases, which showed positive PCR signals. This ratio of 2:1 for M. tuberculosis complex to nontuberculous mycobacteria DNA correlates well with other studies and supports the observation of an increasing rate of nontuberculous mycobacteria infections.23, 24
Our series was split into two groups, on the basis of presence (group 1) or absence (group 2) of corresponding microbiological culture assays. The latter is still considered the goldstandard by many microbiologists, although PCR protocols get increasingly implemented in microbiology laboratories.
Group 1 of the present series showed a concordance of 83% between microbiological culture assays and PCR results. Of note, culture assays remained negative in four cases with positive PCR results for M. fortuitum complex, whereas both M. avium–intracellulare cases in which cultures had been obtained were positive by both techniques. In additon to the four specimens with M. fortuitum complex mentioned above, the other discrepant cases consisted of three samples positive for M. tuberculosis by PCR, but with negative culture assays. An independent confirmation of the presence of mycobacterial DNA was achieved by a separate PCR assay specific for M. tuberculosis in these three cases.8
Although RFLP analysis is a fast and helpful method to discern M. tuberculosis from nontuberculous mycobacteria, it is limited in identifying nontuberculous mycobacteria species. Incomplete digestion can result in ambiguous patterns, and small restriction products (<30 bp) cannot be differentiated sufficiently on conventional agarose gels. Another factor of great importance for the identification of nontuberculous mycobacteria is the high frequency of sequevars, resulting in diverse restriction patterns for members of the same subtype, like for M. chelonae.25 In these circumstances, sequence analysis provided a means to overcome the limitations of RFLP. In cases with atypical restriction patterns, sequencing analysis and homology matching identified various species of nontuberculous mycobacteria but never M. tuberculosis, confirming that RFLP is probably sufficient to make the clinically important distinction between M. tuberculosis and nontuberculous mycobacteria. A problematic, although small group of cases are specimens, which render reproducible signals too weak for RFLP or sequencing. These results should be interpreted with great caution. In our experience, some weak bands which are not cut by any of the restriction enzymes used may actually contain nonmycobacterial sequences which probably represent ubiquitous bacterial DNA amplified at very low efficiency.5
Homology matching with large databases such as the NCBI-database are helpful instruments for analysis of mycobacterial DNA sequences. However, identification and differentiation of mycobacterial subspecies on a genetic basis is still evolving.25, 26, 27, 28, 29, 30 Although amplification of a hypervariable region of the hsp65 gene followed by sequencing allows identification of most species,13, 25, 26, 31 a minority cannot be differentiated because of only minor interspecies divergence in these small PCR fragments. This applies for instance to M. fortuitum and Mycobacterium senegalense, which only differ in a single bp of the analyzed hsp65 fragment.25 Whether some of the sequence variants for members of the M. fortuitum complex described above represent true biovariants or misidentification of nontuberculous mycobacteria species due to the short sequence available for homology matching remains to be determined. Unfortunately, amplification of the 16S rRNA gene does not represent a real alternative for practical purposes, because the usual PCR fragment sizes are too large (more than 500 bp) for the highly fragmented DNA obtained after formalin fixation (suitable fragment sizes usually below 400 bp). However, therapy regimens usually do not differ for species of the same mycobacterial complex, as long as there are no contradictory results of susceptibility testing.23, 32, 33 We therefore believe that reporting the complex, the identified mycobacterial species belongs to, is sufficient for most practical purposes.2, 34, 35, 36
An interesting finding of our study was the frequent identification of M. mucogenicum, a subtype of the M. fortuitum complex, suggesting that it might be occasionally involved in human infections.26, 37, 38 All eight M. mucogenicum cases in the present study showed an identical, previously unreported restriction pattern, despite a sequence divergence in up to 7 bp.
The predominance of species from the M. fortuitum complex in our collection, consisting of M. fortuitum, M. chelonae, M. mucogenicum and M. peregrinum, differs somehow from previously reported series.39, 40, 41, 42 Although this might in part reflect a sampling bias due to the inclusion of specimens submitted in consultation, the biological relevance of the detection of DNA of the above-mentioned species needs to be critically evaluated. Some of the nontuberculous mycobacteria species frequently identified in our series such as M. mucogenicum are regarded as typical apathogenic water contaminants,43 and their presence in surgical biopsies may result from tissue processing or other environmental sources. Although this possibility cannot be excluded entirely for our cases, some facts suggest that a potential pathogenic role for these nontuberculous mycobacteria should be taken into consideration. Besides the fact that our standard negative controls including identically processed control tissues remained negative, the high sequence variability found in our isolates support diverse origins. In addition, well-documented series of infections in nonimmunocompromised patients, such as an outbreak of otitis media caused by patient-to-patient transmission of M. chelonae through contaminated medical devices, underlines the facultative pathogenicity of these species.17 Furthermore, a recent report also demonstrated the facultative pathogenicity of M. mucogenicum by using a microbiological culture approach.38 Nevertheless, one has to keep in mind, that the identification of mycobacterial DNA by PCR does not allow any statements concerning viability or pathogenicity, and treatment decisions have to be based on the integration of clinical, microbiological, histological and molecular findings. Any positive molecular result has to be correlated with morphology and should be interpreted with utmost caution in the absence of adequate histological alterations. Furthermore, we emphasize the importance of periodical quality assessments in diagnostic molecular pathology of infectious disease, in order to advance rules for standardization and interpretation of the different amplification methods.44, 45
In conclusion, the applied hsp65 gene amplification protocol has proven to be a suitable method for detecting mycobacterial DNA in routinely processed pathological specimens.2, 5 RFLP analysis is very helpful for the discrimination of M. tuberculosis complex from nontuberculous mycobacteria; however, is limited for species identification of nontuberculous mycobacteria due to the high frequency of sequevars. In cases with ambiguous or novel restriction patterns, sequencing can confirm the presence of mycobacterial DNA and allows species identification.
References
Woods GL . Diagnostic Pathology of Infectious Diseases. Lea & Febiger: Philadelphia, 1993, pp 382–393.
Schulz S, Kremer M, Cabras AD, et al. Molecular diagnosis of a Mycobacterium chelonae infection. Pathol Res Pract 2001;197:123–126; discussion 127–128.
Kraus M, Benharroch D, Kaplan D, et al. Mycobacterial cervical lymphadenitis: the histological features of non-tuberculous mycobacterial infection. Histopathology 1999;35:534–538.
Connor DH, Chandler FW, Schwartz DA, et al. Pathology of Infectious Diseases, Vol. 1. Appleton & Lange: Stamford, CT, 1997, pp 657–674, 1613–1614.
Cook SM, Bartos RE, Pierson CL, et al. Detection and characterization of atypical mycobacteria by the polymerase chain reaction. Diagn Mol Pathol 1994; 3:53–58.
Perosio PM, Frank TS . Detection and species identification of mycobacteria in paraffin sections of lung biopsy specimens by the polymerase chain reaction. Am J Clin Pathol 1993;100:643–647.
Pao CC, Yen TS, You JB, et al. Detection and identification of Mycobacterium tuberculosis by DNA amplification. J Clin Microbiol 1990;28:1877–1880.
Eisenach KD, Cave MD, Bates JH, et al. Polymerase chain reaction amplification of a repetitive DNA sequence specific for Mycobacterium tuberculosis. J Infect Dis 1990;161:977–981.
Vago L, Barberis M, Gori A, et al. Nested polymerase chain reaction for Mycobacterium tuberculosis IS6110 sequence on formalin-fixed paraffin-embedded tissues with granulomatous diseases for rapid diagnosis of tuberculosis. Am J Clin Pathol 1998;109:411–415.
Gori A, Franzetti F, Marchetti G, et al. Specific detection of Mycobacterium tuberculosis by mtp40 nested PCR. J Clin Microbiol 1996;34:2866–2867.
Roth A, Reischl U, Streubel A, et al. Novel diagnostic algorithm for identification of mycobacteria using genus-specific amplification of the 16S-23S rRNA gene spacer and restriction endonucleases. J Clin Microbiol 2000;38:1094–1104.
Shinnick TM . The 65-kilodalton antigen of Mycobacterium tuberculosis. J Bacteriol 1987;169:1080–1088.
Shinnick TM . Tuberculosis. Current Topics in Microbiology and Immunology, Vol. 215. Springer: Berlin, New York, 1996, pp 315–327.
Goldmann T, Richter E, Galle J, et al. Molecular technologies in pathology: detecting mycobacterial DNA in paraffin-embedded tissues. Pathol Res Pract 1998;194:261A (abstract).
Greer CE, Peterson SL, Kiviat NB, et al. PCR amplification from paraffin-embedded tissues. Effects of fixative and fixation time. Am J Clin Pathol 1991;95:117–124.
Sambrook J, Fritsch EF, Maniatis T . Molecular Cloning: a Laboratory Manual. Cold Spring Harbor Laboratory Press: Cold Spring Harbor, NY, 1989, p 7.46.
Lowry PW, Jarvis WR, Oberle AD, et al. Mycobacterium chelonae causing otitis media in an ear–nose-and–throat practice. N Engl J Med 1988;319:978–982.
Khoor A, Leslie KO, Tazelaar HD, et al. Diffuse pulmonary disease caused by nontuberculous mycobacteria in immunocompetent people (hot tub lung). Am J Clin Pathol 2001;115:755–762.
Frevel T, Schafer KL, Totsch M, et al. PCR based detection of mycobacteria in paraffin wax embedded material routinely processed for morphological examination. Mol Pathol 1999;52:283–288.
Eckburg PB, Buadu EO, Stark P, et al. Clinical and chest radiographic findings among persons with sputum culture positive for Mycobacterium gordonae: a review of 19 cases. Chest 2000;117:96–102.
Evans MJ, Smith NM, Thornton CM, et al. Atypical mycobacterial lymphadenitis in childhood—a clinicopathological study of 17 cases. J Clin Pathol 1998;51: 925–927.
Suskind DL, Handler SD, Tom LW, et al. Nontuberculous mycobacterial cervical adenitis. Clin Pediatr (Phila) 1997;36:403–409.
Sakatani M . Nontuberculous mycobacteriosis; the present status of epidemiology and clinical studies. Kekkaku 1999;74:377–384.
Ferreira-Gonzalez A, Garrett CT . Pitfalls in establishing a molecular diagnostic laboratory. Hum Pathol 1996; 27:437–440.
Ringuet H, Akoua-Koffi C, Honore S, et al. hsp65 sequencing for identification of rapidly growing mycobacteria. J Clin Microbiol 1999;37:852–857.
Shinnick TM, Good RC . Mycobacterial taxonomy. Eur J Clin Microbiol Infect Dis 1994;13:884–901.
Brown-Elliott BA, Griffith DE, Wallace Jr RJ . Newly described or emerging human species of nontuberculous mycobacteria. Infect Dis Clin North Am 2002;16: 187–220.
McNabb A, Eisler D, Adie K, et al. Assessment of partial sequencing of the 65-kilodalton heat shock protein gene (hsp65) for routine identification of mycobacterium species isolated from clinical sources. J Clin Microbiol 2004;42:3000–3011.
Khan IU, Yadav JS . Development of a single-tube, cell lysis-based, genus-specific PCR method for rapid identification of mycobacteria: optimization of cell lysis, PCR primers and conditions, and restriction pattern analysis. J Clin Microbiol 2004;42:453–457.
Brunello F, Ligozzi M, Cristelli E, et al. Identification of 54 mycobacterial species by PCR-restriction fragment length polymorphism analysis of the hsp65 gene. J Clin Microbiol 2001;39:2799–2806.
Pai S, Esen N, Pan X, et al. Routine mycobacterium species assignment based on species-specific allelic variations in the 65-kilodalton heat shock protein gene (hsp65). Arch Pathol Lab Med 1997;121:859–864.
Jorup-Ronstrom C, Julander I, Petrini B . Efficacy of triple drug regimen of amikacin, ethambutol and rifabutin in AIDS patients with symptomatic Mycobacterium avium complex infection. J Infect 1993;26: 67–70.
Wallace Jr RJ, Brown-Elliott BA, Ward SC, et al. Activities of linezolid against rapidly growing mycobacteria. Antimicrob Agents Chemother 2001;45:764–767.
Werner M, Schulz S, Kremer M, et al. Role of molecular pathology in tissue diagnostic of diseases of the gastrointestinal tract. Leber Magen Darm 1999;29:18–24.
Griffith DE, Brown-Elliott BA, Wallace Jr RJ . Diagnosing nontuberculous mycobacterial lung disease. A process in evolution. Infect Dis Clin North Am 2002; 16:235–249.
Diagnosis and treatment of disease caused by nontuberculous mycobacteria. This official statement of the American Thoracic Society was approved by the Board of Directors, March 1997. Medical Section of the American Lung Association. Am J Respir Crit Care Med 1997;156:S1–S25.
Springer B, Bottger EC, Kirschner P, et al. Phylogeny of the Mycobacterium chelonae-like organism based on partial sequencing of the 16S rRNA gene and proposal of Mycobacterium mucogenicum sp. nov. Int J Syst Bacteriol 1995;45:262–267.
Goldblatt MR, Ribes JA . Mycobacterium mucogenicum isolated from a patient with granulomatous hepatitis. Arch Pathol Lab Med 2002;126:73–75.
Ergin A, Kocagoz T, Us D . Evaluation of 120 mycobacterial strains isolated from clinical specimens to the species level by polymerase chain reaction-restriction enzyme analysis. Scand J Infect Dis 2000;32:657–662.
Eriksson M, Bennet R, Danielsson N . Non-tuberculous mycobacterial lymphadenitis in healthy children: another ‘lifestyle disease’? Acta Paediatr 2001;90: 1340–1342.
Flint D, Mahadevan M, Barber C, et al. Cervical lymphadenitis due to non-tuberculous mycobacteria: surgical treatment and review. Int J Pediatr Otorhinolaryngol 2000;53:187–194.
Hidaka E, Honda T, Ueno I, et al. Sensitive identification of mycobacterial species using PCR-RFLP on bronchial washings. Am J Respir Crit Care Med 2000;161:930–934.
Covert TC, Rodgers MR, Reyes AL, et al. Occurrence of nontuberculous mycobacteria in environmental samples. Appl Environ Microbiol 1999;65:2492–2496.
Association for Molecular Pathology statement. Recommendations for in-house development and operation of molecular diagnostic tests. Am J Clin Pathol 1999;111:449–463.
Cabras AD, Kremer M, Schulz S, et al. Quality assessment in diagnostic molecular pathology: experience from a German–Austrian–Swiss multicenter trial. Virchows Arch 2000;437:46–51.
Acknowledgements
We thank Mrs B Geist and Mrs E Hübner for excellent technical assistance, Dr L Binder for helpful discussions and provision of interesting cases and all the pathologists from other institutes for sending the formalin-fixed paraffin-embedded material of granulomatous reactions.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schulz, S., Cabras, A., Kremer, M. et al. Species identification of mycobacteria in paraffin-embedded tissues: frequent detection of nontuberculous mycobacteria. Mod Pathol 18, 274–282 (2005). https://doi.org/10.1038/modpathol.3800289
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.3800289
Keywords
This article is cited by
-
Clinical and laboratory aspects of the diagnosis and management of cutaneous and subcutaneous infections caused by rapidly growing mycobacteria
European Journal of Clinical Microbiology & Infectious Diseases (2013)
-
Concomitant Mycobacterium avium Infection and Hodgkin’s Disease in a Lymph Node from an HIV-negative Child
Pathology & Oncology Research (2011)
-
Experimentelle Immunpathologie und molekulare Infektionspathologie
Der Pathologe (2010)
-
Ancillary techniques in bone marrow pathology: molecular diagnostics on bone marrow trephine biopsies
Virchows Archiv (2005)