Abstract
Lymphatic mapping and sentinel node biopsy are well-established techniques for staging and managing patients with melanoma, breast cancer and other malignancies that spread initially to the regional lymph nodes. Identification of tumor in the sentinel node is the most precise staging technique currently available. The sentinel node is the site of metastatic melanoma in approximately 20% of melanoma patients and if tumor is present in the sentinel node it is customary to perform a complete dissection of the lymph nodes of the affected nodal basin. This may be overtreatment for some patients as tumor is identified in the nonsentinel nodes of only one-third of sentinel node-positive melanoma patients treated by completion lymphadenectomy. If it were possible accurately to identify the minority of patients with tumor in the nonsentinel nodes, the patients most likely to benefit from lymphadenectomy, the remaining patients could be spared a potentially morbid operation that is unlikely to confer clinical advantage. In 90 patients with a melanoma-positive sentinel node, who subsequently had a completion lymphadenectomy, we evaluated and compared the capacity of characteristics of the primary melanoma and of the sentinel node to predict individuals likely to have tumor in nonsentinel nodes. We assessed the Breslow thickness of the primary, the amount of tumor in the sentinel node (relative tumor area) and, as an index of immune modulation of the sentinel node, the density of dendritic leukocytes in the nodal paracortex. The relative area of tumor in the sentinel node and Breslow thickness of the primary melanoma most accurately predicted the presence of tumor in the nonsentinel nodes (P=0.0001 in both cases—Wilcoxon rank sums). The presence of melanoma in the nonsentinel nodes was also predicted by the density of dendritic leukocytes in the paracortex (P=0.008–Wilcoxon rank sums). These three observations assessed alone and in combination predict the presence of tumor in the nonsentinel nodes with high accuracy. The same characteristics also significantly correlated with tumor recurrence (tumor burden, P=0.0001, Breslow, P=0.0001 and dendritic cell density, P=0.0007) and death from melanoma (tumor burden, P=0.0001, Breslow, P=0.0001 and dendritic cell density, P=0.0026)
Similar content being viewed by others
Main
The techniques of lymphatic mapping and sentinel node biopsy were developed to improve the management of patients with high-risk (thick and deep) primary melanoma with a high potential for metastases, but no clinical evidence of metastatic spread.1, 2 These techniques have widely been adopted and applied to the management of melanoma, cancer of the breast,3 colon,4, 5 penis,6 vulva7 and other tumors that metastasize via the lymphatics.8 The approaches accurately stage tumor extension to the regional lymphatic basin and spare many patients the morbidity of extensive nodal surgery. The impact of the approach on overall survival will remain unknown until outcome analysis of ongoing clinical trials is complete.9
The frequency of a melanoma-positive sentinel node is remarkably similar in many published clinical reports, in the region of 20%, with minor variations that reflect the thickness of the primary melanomas that comprise each individual study. At present, all patients who have a melanoma-positive sentinel node undergo subsequent complete dissection of the affected node basin (completion lymphadenectomy). When the nonsentinel lymph nodes excised at complete dissection are evaluated microscopically (hematoxylin and eosin (HE) and immunohistochemically stained slides), only one-third of completion lymphadenectomy specimens contain nodes that harbor melanoma cells.9 Thus, in two-thirds of the patients who have a melanoma-positive sentinel node, metastatic tumor is found only in the sentinel node. It is probable that patients with metastatic melanoma confined to the sentinel node do not require completion lymphadenectomy. There is a need for techniques that identify patients who, despite a tumor-positive sentinel node, have a low probability of metastatic tumor in the nonsentinel nodes. If this identification could be made with high accuracy completion, lymphadenectomy could be reserved for patients with a substantial likelihood of metastases in the nonsentinel node.
How could such a prediction be made? Characteristics of the primary tumor and the sentinel node are promising sources of information. Micrometer-measured thickness remains the most durable single characteristic of the primary melanoma that correlates with clinical outcome.10 We have previously shown that the amount of tumor in lymph nodes, measured as tumor area relative to lymph nodal area is a highly accurate predictor of clinical outcome.11 Micrometer-assessed evaluation of relative tumor burden in lymph nodes is an excellent surrogate for more cumbersome assessments of tumor area or volume.11 Sentinel nodes show selective immune modulation, most readily seen as alterations of the relative area of the nodal paracortex and the area, frequency and dendritic morphology of paracortical dendritic leukocytes.12, 13, 14
In this report, we have analyzed these indices in patients with metastatic melanoma in the sentinel node and assessed their capacity, individually and in combination, to predict the tumor status of nonsentinel node and the likelihood of tumor recurrence and death from melanoma.
Materials and methods
The subjects of this study were 90 patients with cutaneous malignant melanoma who were found to have metastatic melanoma in at least one sentinel node in sections stained by HE or on immunohistochemistry using antibodies to S-100 protein and HMB-45. These patients are drawn from a group of 500 melanoma patients treated by lymphatic mapping and sentinel node identification and evaluation at the Center for Health Sciences, UCLA or The John Wayne Cancer Institute, St John's Hospital and Health Center, Santa Monica. The remaining 410 patients showed no evidence of metastatic melanoma in the sentinel node on evaluation by HE histology or immunohistochemistry and did not receive a completion lymph node dissection.
The sentinel nodes were bisected through the longest meridian and 10 fully representative sections were prepared from each cut face of the node. Using our standard protocol,15 sections 1, 3, 5 and 10 were stained with HE, section 2 for S-100 and section 3 for HMB-45. If suspicious, but not completely diagnostic appearances were encountered, additional series of 10 sections were cut from both halves of the sentinel node and stained in the same manner. This practical approach balances desirable extensive sampling with the requirements for cost containment.
For each patient, we evaluated the micrometer-measured thickness of the primary tumor.10 We next determined the area of the node that was occupied by tumor, using a computer-assisted image analysis program (Planar Morphometry, Version 2.1, Southern Micro Instruments, Atlanta, GA, USA) and expressed this as a percentage of the total area of the sentinel node. In sections stained for S-100 protein, we assessed the area of the node occupied by interdigitating dendritic cells of the paracortex and expressed this as a percentage of the total area of the node.1, 13 We also determined the density of interdigitating dendritic cells/mm2 in the nodal paracortex using the technique described by Huang et al.13
All 90 patients had a completion lymph node dissection. All excised nonsentinel nodes were evaluated for the presence of melanoma by examining HE-stained sections and sections immunostained for S-100 protein and HMB-45.
We obtained information on the subsequent clinical course of these patients, dividing them into those who remained tumor free and those who recurred and died of melanomatosis. Median follow-up was 7 years with a range from 1 to 13 years. Where melanoma had recurred, we recorded the time from nodal surgery to recurrence.
We assessed and correlated primary tumor thickness, the amount of tumor in the sentinel node and the area and density of integrating dendritic cells in the sentinel node with the presence of melanoma in the nonsentinel node. We also related these parameters of the primary melanoma and sentinel node to tumor recurrence and death from melanoma. The various features were compared for their ability to predict the presence or absence of tumor in the nonsentinel nodes, melanoma recurrence and death from melanoma.
Statistical techniques employed were the Wilcoxon rank sums, logistic regression, tree-based modeling, Cox proportional hazard regression modeling, the log rank test and receiver operating characteristic curves.
Results
Prediction of the Presence of Melanoma in NonSentinel Nodes (Table 1, Figures 1 and 2)
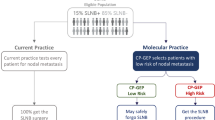
A tree-based modeling technique was used to explore rules that can be applied to predict metastatic melanoma in the NSN. The tree structure is depicted above. *Number of patients with positive NSN/total patients (percentage with positive NSN). †The P-value is derived from analysis of the split using χ2 test.
On a univariate basis (Wilcoxon rank sums), all four parameters evaluated were significantly correlated with nonsentinel node tumor status. The mean Breslow thickness of the primary melanoma of the 71 patients with no tumor in the nonsentinel node was 2.32±1.41 mm, compared to 3.85±1.79 mm for the 19 patients in whom tumor was identified in the nonsentinel (P=0.0001). The mean relative area of the sentinel node occupied by tumor was 4.3±13.2% for patients who had no tumor in the nonsentinel, compared to 30.46±26.13% for patients with tumor present in the nonsentinel (P=0.0001). The area of the sentinel node occupied by S-100+ interdigitating dendritic cells was significantly less in patients with tumor in the nonsentinel (mean 2.12±2.91%) than in the individuals with tumor-free nonsentinel node (mean 6.18±10.56%) (P=0.0245). The mean density of S-100+ interdigitating dendritic cells in the sentinel node was significantly higher in patients with tumor-free nonsentinel node (69.34±56.33/mm2 than in the sentinel node of individuals who had melanoma in the nonsentinel node (35.65±31.56/mm2) (P=0.008).
A logistic regression model was used to evaluate the relative power of the various factors to predict the likelihood that there would be melanoma in the nonsentinel node. Tumor burden in the sentinel node and the Breslow thickness of the primary melanoma were selected as significant predictors of nonsentinel node tumor status by this approach. Tumor burden in the sentinel node was the most significant predictor (P=0.0013) with an odds ratio of 1.06 (95% CI, 1.02–1.09). Breslow thickness was almost as strong a predictor (P=0.0033) with an odds ratio of 1.49 with a 95% CI of 1.03–2.15.
A tree-based modeling technique was used to explore the prediction rules that could be applied (Figure 1). When melanoma occupied 4% or more of the sentinel node 17/26 patients (65.4%) had tumor spread to the nonsentinel node. In contrast, if less than 4% of the sentinel node was occupied by melanoma only 2/64 patients (3%) had tumor in the nonsentinel node (P=0.001–χ2). Tumor occupied less than 1% of the sentinel node in 52 patients and none of these individuals had tumor in the nonsentinel node. When tumor occupied 1–4% of the area of the sentinel node, 2/12 patients (16.7%) had tumor in the nonsentinel node (P=0.03). In patients with low tumor burden (1–4% of nodal area), tumor extension to nonsentinel nodes is more likely if the area of the node occupied by S-100+ interdigitating dendritic cells is small (a finding that likely reflects nodal immune downregulation) (data not shown in figure). Thus, in patients with low tumor burden, a nonsentinel node contained tumor in 2/5 patients (40%) if the interdigitating dendritic cells occupied less than 2% of total lymph node area. None of 7 patients in whom interdigitating dendritic cells occupied more than 2% of total lymph node area had tumor in a nonsentinel node.
To further assess the relative discriminatory capacities of tumor burden, Breslow thickness and dendritic cell area and density as predictors of nonsentinel node tumor status, we obtained the areas under the receiver operating characteristic curves and plotted ROC curves. Tumor burden was the most effective predictor of nonsentinel node tumor status, followed by Breslow thickness, dendritic cell area and dendritic cell density (Figure 2).
Prediction of Survival (Table 2)
Considering the individual parameters, both the thickness of primary melanomas and the amount of tumor in the sentinel node (as a percentage of the lymph node area) were very closely correlated with clinical outcome. The density of interdigitating dendritic cells in the paracortex was also significantly correlated with the outcome, but less closely than were primary tumor thickness or sentinel node tumor burden. In all, 34 of the 90 patients died of melanoma. The mean thickness of their primary melanomas was 3.42±1.64 mm. The mean thickness of the primary tumor in patients who survived was 2.17±1.41 mm (P=0.0001). In individuals who died of melanoma, the mean area of the sentinel node occupied by melanoma was 21.12±26.42%, compared to 2.97±9.23% in patients who survived (P=0.0001). Interdigitating dendritic cell density in patients who died of melanoma was 41.56±58.84/mm2, significantly less than the mean density of 74.78±46.6/mm2 observed in survivors (P=0.0026). The area of the sentinel node occupied by interdigitating dendritic cells did not differ significantly between patients who died of melanoma and survivors.
A proportional hazard regression model was used to examine the association of primary tumor thickness, amount of tumor in the sentinel node and density of interdigitating dendritic cells in the sentinel node with clinical outcome. The model selected tumor burden and micrometer-measured thickness as the most significant predictors of melanoma death or survival. Tumor burden was the strongest predictor with a risk ratio of 1.02 (95% CI, 1.01–1.04) (P=0.0015). Primary tumor thickness was the second most potent predictor with a risk ratio of 1.23 (95% CI, 1.02–1.48) (P=0.0297).
A regression tree structure (Figure 3) selected the predictors that were identified by the proportional hazard model. In all, 34 of the 90 patients (38%) died of melanoma and disease-specific death clearly related to the amount of tumor in the sentinel node. A total of 20 of 26 individuals (77%) who had melanoma that occupied more than 4% of the sentinel nodal area died of melanoma (77%). In contrast, 14/64 patients (22%) with melanoma that occupied less than 4% of the sentinel node area died of melanoma (22%) (P=0.0001). The 64 individuals who had a relatively small amount of tumor in the sentinel node (<4%) could be further subdivided on the basis of the density of paracortical dendritic cells. In total, 11 of 33 patients (33%) who had less than 65 paracortical interdigitating cells/mm2 in the sentinel node died of melanoma. This compares with 3/31 melanoma deaths in patients who had more than 65 paracortical interdigitating dendritic cells/mm2 in the sentinel node (10%) (P=0.0185).
Survival curves (Figure 4) show significant survival differences that relate to the amount of tumor present in the sentinel node. In the case of patients with a low tumor burden (<4%) individuals with abundant interdigitating dendritic cells (indicating nodal immune competence) survived better than those with fewer interdigitating dendritic cells (indicating immune downregulation) (P=0.0185), the area of the sentinel node being occupied by interdigitating dendritic cells. Patients with a higher tumor burden (>4%) survived less well than those with a relatively low tumor burden (<4%) (P=0.0001) in both comparisons.
Survival curves for patients with different amount of tumor in the sentinel node ((A), (B), (C)) and differing density of IDC ((A), (B)). Group A is patients with less than 4% of the SN replaced by tumor and IDC density of less than 65 IDC/mm2. Group B is patients with less than 4% of the SN replaced by tumor and IDC density greater than 65 IDC/mm2. Group C is patients with more than 4% of the SN replaced by tumor. Statistical comparisons using the log rank test: AvB, P=0.0185, AvC, P=0.0001 and BvC, P=0.0001
Prediction of Recurrence of Melanoma(Table 3 and Figures 5 and 6)
Curves reflecting time to melanoma recurrence related to different amounts of tumor in the sentinel node ((A), (B), (C)) and differing densities of IDC ((A), (B)). Group A is patients with less than 4% of the SN replaced by tumor and IDC density less than 65/mm2. Group B is patients with less than 4% of the SN replaced by tumor and IDC density greater than 65/mm2. Group C is patients with more than 4% of the SN replaced by tumor. Statistical comparisons using the log rank test: AvB, P=0.0078, AvC, P=0.0001 and BvC, P=0.0001.
A tree-based modeling technique was used to explore rules that can be applied to predict patients likely to develop recurrent melanoma. The tree structure is depicted above. * Patients with recurrent melanoma/total patients (percentage of patients who recurred). †The P-value is derived from analysis of the split using χ2 test.
The factors that are associated with melanoma recurrence, amount of tumor in the sentinel node and micrometer-measured thickness of the primary tumor are identical to those correlated with likelihood of death from melanoma.
Discussion
The techniques of lymphatic mapping and sentinel node biopsy have been accepted with remarkable enthusiasm. The appeal of the approaches lies in their ability to identify preoperatively the lymph node(s) most likely to contain early metastatic melanoma. The presence or absence of tumor in the sentinel node accurately predicts whether or not there will be tumor in other nodes of the lymph node group.2, 9 The underlying principle, that there is a lymph node (or nodes) that are uniquely susceptible to first colonization by lymphatic spread tumor cells, seems sound. The principle applies not just to cutaneous melanoma but to breast cancer,3 Merkel cell cancer,16 squamous carcinoma of the skin and vulva and tumors of the gastrointestinal tract.4, 5 The position of the sentinel node is determined by the course of the lymphatics that drain the body site of the primary tumor rather than the fixed anatomic position of individual node(s) relative to the primary tumor. It is necessary to use a visible dye and/or radioactive marker to highlight the relevant afferent lymphatics and the lymph node that is their destination.9 Regardless of the histologic type of the primary tumor, the findings are basically similar. The nodes identified by dye and/or isotope as sentinel are preferentially the site(s) of the earliest stages of metastasis.17
In the great majority of patients with a positive sentinel node, tumor cells are identified in a single node and it is very unusual to identify tumor cells in more than three lymph nodes.17 Tumor cells are usually few in number and are most often identified, dispersed singly or as microcolonies of up to 20 cells, in the subcapsular sinuses.8, 15 Less often tumor cells are identified in afferent lymphatics or deeper sinuses. The relatively small number of tumor cells that is characteristically present makes it essential to supplement conventional HE staining with appropriate immunohistochemical reagents.15
Regardless of the histological type of the primary tumor, the great majority of sentinel nodes contain no tumor and in this case the nonsentinel nodes of the regional node group will be free of tumor. If the sentinel node contains tumor, some patients will also have tumor cells in at least one of the nonsentinel nodes removed at completion of the lymph node dissection. The amount of tumor present in the nonsentinel nodes is usually limited, scattered single cells or microcolonies affecting only one or two nodes.17
It is customary to perform a complete lymph node dissection only if the sentinel node contains tumor. This spares the 80% of patients who have no tumor in the sentinel node complete lymphadenectomy, an operation that carries substantial morbidity (mainly edema and limb dysfunction) and is unlikely to confer survival benefit on this group of patients. Determination of sentinel node status thus crisply separates melanoma patients into high- and low- risk groups, providing, for the first time, a logical basis on which assessment of the need for additional surgery and adjuvant therapy can be based.
Given our present knowledge, it is reasonable to justify completion lymphadenectomy for the small minority of patients who have tumor in both sentinel and nonsentinel nodes. Two-thirds of melanoma patients with a positive sentinel node have no tumor identified in the nonsentinel nodes removed at completion lymphadenectomy and it is less easy to justify a major operation for these individuals. It is arguable that if these individuals could be identified preoperatively, they could and should be spared complete lymphadenectomy.
The data from this study and other studies18 suggest that it is possible to identify patients with a positive sentinel node who are unlikely to have metastatic tumor in the nonsentinel nodes. Our data indicate that a relatively simple assessment of tumor area relative to nodal area11, 19, 20 provides a strong indication of the likelihood of the presence of tumor in the nonsentinel nodes. Thus, 17/26 patients (65.4%) with metastatic melanoma that occupied more than 4% of the sentinel node (high tumor burden) had tumor in at least one nonsentinel node. Nonsentinel node tumor was significantly less frequent in patients in whom tumor occupied less than 4% of the sentinel node (low tumor burden) (2/64–3.1%, P=0.001). Patients with low tumor burden in the sentinel node could be further subdivided into more precise risk categories. Thus, 0/52 patients with sentinel node that were less than 1% replaced by tumor (very low tumor burden) had tumor in the nonsentinel node. This contrasts with 2/12 patients (16.7%) with sentinel node that contained 1–4% of tumor who had tumor in the nonsentinel node (P=0.03). Patients with a low tumor burden in the sentinel node who had tumor in the nonsentinel node additionally showed a reduced number and density of interdigitating cells, a finding that likely indicates relative immune suppression of the sentinel node.1, 13, 14 Patients with a low tumor burden in the sentinel node who had no tumor in the nonsentinel node had a higher frequency and density of interdigitating dendritic cells. These observations that correlate tumor extension with tumor burden and nodal immune status are biologically relevant as the same attributes relate clearly and significantly to the likelihood of recurrence and death from melanoma. We have chosen to develop the argument on the basis of nodal tumor burden as this seems to be the strongest predictor of nonsentinel node tumor status, but clearly it would be possible to construct a similar model on the basis of Breslow thickness of the primary melanoma. There is, however, some measure of disagreement in published reports on the predictive value of micrometer-measured thickness of the primary melanoma. Some studies report that thin primary melanomas are associated with a low incidence of tumor spread beyond the sentinel node,21, 22, 23, 24, 25 while others have not reported this correlation.26, 27
The algorithmic approach that we present is practical and yields reliable information. It may be criticized as less than ideal on the grounds that measurement of tumor area is cumbersome and not part of the day-to-day activities of practicing pathologists who are called upon to assess sentinel nodes. It is certainly encouraging that others report excellent predictive result, based on area of sentinel node metastases.20, 28 We have previously shown that that maximum tumor diameter, measured by an ocular micrometer is an acceptable surrogate for tumor area in evaluating tumor burden in lymph nodes.11, 29 The approach of using micrometric assessment of metastatic tumor diameter has been profitably developed by Starz et al,30, 31 in Augsburg, and alone or in combination with determination of the number of 1-mm-thick slices of the sentinel nodes that contain tumor applied to the evaluation of sentinel nodes. The use of ocular micrometers to evaluate the diameter of metastases in sentinel node has also been reported by Wagner et al,32 and Ranieri et al.33 We are currently collaborating with the Augsburg group to compare the predictive value of area measurements of nodal tumor with the information obtainable by evaluation of the micrometer-measured maximum diameter nodal tumor. If the micrometer approach provides guidance comparable to the tumor predictive accuracy of tumor area assessment, it would be preferable as a relatively simple approach since the technique is already widely used in routine anatomic pathology evaluation. The relative efficiency of these two approaches will be tested in an upcoming National Cancer Institute study.
The criticism, that evaluation of tumor area is nonstandard, time consuming and an added expense, could also be applied to our observation that in the low tumor burden patients the presence of tumor in the nonsentinel node correlates with reduced frequency and density of interdigitating dendritic cells. We have shown that that there is a reduction in dendritic cells in nodes anatomically close to tumor12 and in the sentinel nodes of patients with breast cancer13 and melanoma.1, 14 Reduction in dendritic cell frequency, density and loss of antigen-presentation-associated polydendritic morphology point to dysfunction of interdigitating dendritic cells in sentinel nodes. The degree of interdigitating dendritic cell reduction is variable in different sentinel nodes and more severe degrees of reduction are correlated with enhanced likelihood of there being metastatic tumor in the sentinel and nonsentinel nodes. In this study, the contribution of the interdigitating dendritic cells data to the analytical process seems relatively small and it may be that at a practical level it will not be essential to include this type of analysis. If more extended studies confirm our preliminary findings it will be necessary to devise a relatively simple and practical technique to assess the interdigitating dendritic cells population of sentinel node. Continued study of nodal dendritic leukocytes and other immunologically active cells is in any case likely to yield important and potentially practical information in regard to the interaction of primary melanoma (and other tumor) and adjacent lymphoid tissues.
Relatively simple pathologic approaches can, in the experience of many investigators, provide valuable assistance in determining the extent of surgery required for patients with early metastases of melanoma in the sentinel node. It has been shown that similar approaches are also applicable to evaluation of the sentinel node in breast cancer18, 34 and Merkel cell carcinoma31 and it will be important to assess whether similar approaches can be successfully applied to sentinel node removed from patients with other kinds of cancer. The evaluations required to go some distance beyond routine pathological assessment, but if it is shown that there is value for patient evaluation and management, pathologist will undoubtedly incorporate these new tasks in the range of their activities.
References
Cochran AJ, Morton DL, Stern S, et al. Sentinel lymph nodes show profound downregulation of antigen-presenting cells of the paracortex: Implications for tumor biology and treatment. Mod Pathol 2001;14:604–608.
Morton DL, Wen D-R, Wong JH, et al. Technical details of intraoperative lymphatic mapping for early stage melanoma. Arch Surg 1992;127:392–399.
Giuliano AE, Kirgan DM, Guenther JM, et al. Lymphatic mapping and sentinel lymphadenectomy for breast cancer. Arch Surg 1994;220:391–398.
Saha S, Nora D, Wong JH, et al. Sentinel lymph node mapping in colorectal cancer—a review. Surg Clin North Am 2000;80:1811–1819.
Wong JH, Steineman S, Calderia C, et al. Ex vivo sentinel node mapping in carcinoma of the colon and rectum. Ann Surg 2001;233:515–521.
Cabanas RM . An approach for the treatment of penile carcinoma. Cancer 1977;39:456–466.
Ghurani GB, Penalver MA . An update on vulvar cancer. Am J Obstet Gynecol 2001;185:294–299 (Review).
Cochran AJ, Roberts AA, Saida T . The place of lymphatic mapping and sentinel node biopsy in oncology. Int J Clin Oncol 2003;8:139–150.
Morton DL, Thompson JF, Essner R, et al. Validation of the accuracy of intraoperative lymphatic mapping and sentinel lymphadenectomy for early stage melanoma: a multicenter trial. Ann Surg 1999;230:453–455.
Breslow A . Thickness, cross-sectional areas and depth of invasion in the prognosis of cutaneous melanoma. Ann Surg 1970;172:902–908.
Cochran AJ, Lana AMA, Wen D-R . Histomorphometry in the assessment of prognosis in Stage II melanoma. Am J Surg Pathol 1989;13:600–604.
Cochran AJ, Pihl E, Wen D-R, et al. Zoned immune suppression of lymph nodes draining malignant melanoma: histologic and immunohistologic studies. J Natl Cancer Inst 1987;78:399–405.
Huang RR, Wen D-R, Guo J, et al. Modulation of paracortical dendritic cells and T lymphocytes in breast cancer sentinel nodes. Breast J 2000;6:225–232.
Lana A-MA, Wen D-R, Cochran AJ . The morphology, immunophenotype and distribution of paracortical dendritic leukocytes in lymph nodes regional to cutaneous melanoma. Melanoma Res 2001;11:1–10.
Cochran AJ . Surgical pathology remains pivotal in the evaluation of ‘sentinel’ lymph nodes. Am J Surg Pathol 1999;23:1169–1172.
Messina JL, Reintgen DS, Cruse CW, et al. Selective lymphadenectomy in patients with Merkel cell (cutaneous neuroendocrine) carcinoma. Ann Surg Oncol 1997;4:389–395.
Cochran AJ . sentinel lymph node biopsy for melanoma: pathologic aspects. In: H.S.C. III (ed). Sentinel Lymph Node Biopsy. Martin Duntz: New York, 2002, pp. 79–90.
Giuliano AE, Dale PS, Turner RR, et al. Improved axillary staging of breast cancer with sentinel lymphadenectomy. Ann Surg 1995;222:394–399 (discussion 399-01, review).
Cochran AJ, Morton DL, Johnson TD, et al. Prediction of outcome and tumor status of the non-sentinel node in melanoma patients with a positive sentinel node. Mod Pathol 2001;13:61A.
Wen D-R, Huang R-R, Starz H, et al. Prognostic factors predict nonsentinel node status in melanoma patients. Mod Pathol 2003;16:101A.
Joseph E, Brobeil A, Glass F, et al. Results of complete lymph node dissection in 83 melanoma patients with positive sentinel nodes. Ann Surg Oncol 1998;5:119–125.
Clary BM, Brady MS, Lewis JJ, et al. Sentinel lymph node biopsy in the management of patients with primary cutaneous melanoma: review of a large single-institutional experience with an emphasis on recurrence. Ann Surg 2001;233:250–258.
Haddad FF, Stall A, Messina J, et al. The progression of melanoma nodal metastasis is dependent on tumor thickness of the primary lesion. Ann Surg Oncol 1999;6:144–149.
Reeves ME, Delgado R, Busam KJ, et al. Prediction of nonsentinel lymph node status in melanoma. Ann Surg Oncol 2003;10:27–31.
Wagner JD, Gordon MS, Chuang TY, et al. Predicting sentinel and residual lymph node basin disease after sentinel lymph node biopsy for melanoma. Cancer 2000;89:453–462.
Wagner JD, Park HM, Coleman III JJ, et al. Cervical sentinel lymph node biopsy for melanomas of the head and neck and upper thorax. Arch Otolaryngol Head Neck Surg 2000;126:313–321.
McMasters KM, Wong SL, Edwards MJ, et al. Frequency of nonsentinel lymph node metastasis in melanoma. Ann Surg Oncol 2002;2:137–141.
Carlson GW, Murray DR, Lyles RH, et al. The amount of metastatic melanoma in a sentinel lymph node: does it have prognostic significance? Ann Surg Oncol 2003;10:575–581.
Cochran AJ, Binder S, Remotti F . The role of microscopic evaluation in the management of cutaneous melanoma. Cancer Treat Res 1993;65:69–102.
Starz H, Balda BR, Kramer KU, et al. A micromorphometry-based concept for routine classification of sentinel lymph node metastases and its clinical relevance for patients with melanoma. Cancer 2001;91:2110–2121.
Düker I, Starz H, Bachter D, et al. Prognostic and therapeutic implications of sentinel lymphonodectomy and S-staging in Merkel cell carcinoma. Dermatology 2001;202:225–229.
Wagner JD, Davidson D, Coleman III JJ, et al. Lymph node tumor volumes in patients undergoing sentinel lymph node biopsy for cutaneous melanoma. Ann Surg Oncol 1999;6:398–404.
Ranieri JM, Wagner JD, Azuaje R, et al. Prognostic importance of lymph node tumor burden in melanoma patients staged by sentinel node biopsy. Ann Surg Oncol 2002;9:975–981.
Viale G, Maiorano E, Mazzarol G, et al. Histologic detection and clinical implications of micrometastases in axillary sentinel lymph nodes for patients with breast carcinoma. Cancer 2001;92:1378–1384.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cochran, A., Wen, DR., Huang, RR. et al. Prediction of metastatic melanoma in nonsentinel nodes and clinical outcome based on the primary melanoma and the sentinel node. Mod Pathol 17, 747–755 (2004). https://doi.org/10.1038/modpathol.3800117
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.3800117
Keywords
This article is cited by
-
Current management of melanoma patients with nodal metastases
Clinical & Experimental Metastasis (2022)