Abstract
There are currently no universally accepted indications and criteria for additional surgical resection of the colorectum after endoscopic resection of the submucosal invasive cancer. The purpose of the present study is to establish accurate indications and criteria for additional surgical resection of the colorectum, based on the prediction of lymph node metastasis, after endoscopic resection of the submucosal invasive cancer. We investigated 140 submucosal invasive colorectal cancers and analyzed the pathologic factors of lymph node metastasis. The tumors were evaluated for pathologic factors in the invasive area of the submucosal carcinoma and were compared between the cases with lymph node metastasis and those without lymph node metastasis. Lymph node metastasis was observed in 13 cases (9%). Univariate logistic regression analysis showed that the depth of invasion, cribriform-type structural atypia, absence of lymphoid infiltration, lymphatic permeation, and venous permeation were statistically significant as risk factors for lymph node metastasis. Multivariate logistic regression analysis showed that the important risk factors included, in decreasing order, lymphatic permeation, absence of lymphoid infiltration, cribriform-type structural atypia, venous permeation, and depth of invasion. Submucosal invasion of 2 mm or more, and/or, depth of lymphatic permeation of 2 mm or more are risk factors for lymph node metastasis. The pathologic criteria based on our results for additional colectomy enables greater accuracy selection of patients who will undergo further surgical treatment after endoscopic resection.
Similar content being viewed by others
Main
Endoscopic resection has become the established standard treatment for mucosal carcinoma and adenoma of the colon. Submucosal invasive cancer may not be diagnosed, in some cases, until after endoscopic resection. Thus, pathologists are increasingly encountering submucosal invasive colorectal carcinomas, which are endoscopically resected. Since 10% or less of cases of submucosal invasive cancer had metastasized to the lymph nodes according to previous reports,1, 2, 3, 4, 5, 6, 7 additional surgical resection of the colorectum after endoscopic resection of submucosal invasive cancer is needed for curative treatment. However, there are currently no universally accepted indications and criteria for additional surgical resection of the colorectum after endoscopic resection of submucosal invasive cancer. As a result, many cases (the remainder, except cases with lymph node metastasis, ie, about 90% of the total cases) involving additional surgical resection of the colorectum constitute overtreatment. Establishment of accurate criteria for additional surgical resection of the colorectum, based on the prediction of lymph node metastasis, after endoscopic resection of submucosal invasive cancer is more than necessary. Thus, toward this goal, we investigated and analyzed the pathologic factors of lymph node metastasis of submucosal invasive colorectal cancer.
Materials and methods
A total of 140 submucosal invasive carcinomas of the colorectum that were surgically resected with regional lymph nodes were examined. The reason why we collected surgically resected specimens rather than endoscopically resected specimens for materials of this study is that lymph node metastasis can be accurately evaluated. The resected materials were fixed in formalin, embedded in paraffin, and stained with HE. Sections (2 μm thick) of the maximum diameter of the tumor were evaluated for the following pathologic factors. All cases were blindly reviewed twice by three of the authors (YE, TY and YK). If discrepancies arose, the cases were discussed to achieve consensus while being viewed at multihead microscope.
-
1)
Depth of submucosal invasion
-
2)
Width of submucosal invasion: The depth and width of invasion were measured by the method shown in Figure 1.
-
3)
Area of submucosal invasion: The product of the depth and width of submucosal invasion was assumed to be the area of invasion.
-
4)
Histological classification of the invasive area of submucosal carcinoma: Invasive areas of submucosal carcinoma were classified as well-differentiated adenocarcinoma, moderately differentiated adenocarcinoma, poorly differentiated adenocarcinoma, and mucinous adenocarcinoma according to histological typing of intestinal tumors of the World Health Organization (WHO).8 Moreover, mucinous adenocarcinoma was classified into two subgroups: undifferentiated-type mucinous adenocarcinoma to designate undifferentiated nontubular adenocarcinomas (the majority of which was signet ring cell carcinoma) and differentiated-type mucinous adenocarcinoma to designate differentiated tubular adenocarcinomas (Figure 2). In classifying the carcinoma, the predominant pattern is adopted as its representative histological type and grade. For example, for a tumor consisting mainly of well-differentiated adenocarcinoma with a part of moderately differentiated adenocarcinoma, a diagnosis of well-differentiated adenocarcinoma should be made.
Figure 2 Subgroups of mucinous adenocarcinoma (muc). (a) Undifferentiated-type mucinous adenocarcinoma to designate undifferentiated nontubular adenocarcinomas (the majority of which were signet ring cell carcinoma). (b) Differentiated-type mucinous adenocarcinoma to designate differentiated tubular adenocarcinomas.
-
5)
Structural atypia in the invasive area of submucosal carcinoma: Structural atypia in the invasive area of the cancer was classified as one of two types: cribriform type, indicated by sieve-like internal branching (Figure 3a), and dendritic type, indicated by tree-like external branching (Figure 3b). The presence or absence of structural atypia of each of these two types was determined.
-
6)
Bud-like structure9 (micronest formation or single-cell infiltration of cancer cells) in the invasive area of submucosal carcinoma: The presence or absence of a bud-like structure (Figure 4) in the invasive area of the cancer was determined. This classification does not correlate to histological classification because it is made without depending on the amount of a bud-like structure.
-
7)
Mode of growth in the invasive area of submucosal carcinoma: Modes of growth in the invasive area of the cancer were classified into five types: expansive type (submucosal invasion consisting of solid cancer nests without fibrous stroma), infiltrating type (cancer cells infiltrated with much fibrous stroma), mixed type (mixture of expansive and infiltrating types), predominant expansive type (mixture of expansive and infiltrating types, but the expansive type is predominant), and predominant scirrhous type (mixture of expansive and infiltrating types, but the infiltrating type is predominant).
-
8)
Lymphoid cell infiltration in the invasive area of submucosal carcinoma: The degree of lymphoid infiltration in submucosal invasive part of the cancer was classified as either negative (−) (no or little infiltration) or positive (+) (infiltration with follicular structure or more lymphoid cells than the number of cancer cells).
-
9)
Presence and depth of lymphatic permeation: Presence or absence of lymphatic permeation was determined. The depth of lymphatic permeation was defined as the vertical distance from mucosal muscle to the deepest lymphatic permeation point.
-
10)
Presence and depth of venous permeation and depth of venous permeation: The presence or absence of venous permeation was evaluated. Venous permeation was detected using Elastica van Gieson staining. The depth of venous permeation was defined as the vertical distance from mucosal muscle to the deepest venous permeation point.
The above-mentioned pathologic factors were compared between the cases that were positive for lymph node metastasis and those that were negative for lymph node metastasis. Each pathologic factor was assessed separately by a univariate logistic regression analysis. Differences at P<0.05 were considered significant. Factors determined to be significant by univariate analysis were analyzed by a multivariate logistic regression, and an odds ratio with 95% confidence interval was calculated for each factor. Statview Version 5.010 was used for all statistical calculations. Finally, we produced pathologic criteria (algorithm) of the prediction of lymph node metastasis, based on these results, for additional colectomy after endoscopic resection of submucosal invasive cancer of the colorectum. The sensitivity, specificity, positive and negative predictive value, and overall accuracy of this criteria were calculated.
Results
Gross appearance
In all, 11 lesions were pedunculated, 44 were sessile with depression, and 85 were sessile without depression.
Lymph Node Metastasis
Submucosal invasive cancer with lymph node metastasis was observed in 13 cases, and submucosal invasive cancer with no lymph node metastasis occurred in 127 cases.
Depth of Invasion (Table 1)
The mean depth of submucosal invasion in all cases was 2.7 mm, and the mean depth was 4.0 mm2 in cases of cancer with lymph node metastasis and 2.5 mm in cases of cancer with no lymph node metastasis.
Width of Invasion (Table 1)
The mean width of submucosal invasion in all cases was 5.9 mm, and the mean width was 9.4 mm in cases of cancer with lymph node metastasis and 5.6 mm in cases of cancer with no lymph node metastasis.
Area of Invasion (Table 1)
The mean area of submucosal invasion in all cases was 19.55 mm2, and the mean area was 41.3 mmin cases of cancer with lymph node metastasis and 17.32 mm2 in cases of cancer with no lymph node metastasis.
Histological Classification in the Invasive Area of Submucosal Carcinoma (Table 2)
Histological examination in the invasive area of submucosal carcinoma showed 67 well-differentiated adenocarcinoma, 62 moderately differentiated adenocarcinoma, two poorly differentiated adenocarcinoma, two undifferentiated-type mucinous adenocarcinoma, and seven differentiated-type mucinous adenocarcinoma. Lymph node metastasis occurred in 2.9% of well-differentiated adenocarcinoma cases, 14.5% of moderately differentiated adenocarcinoma cases, 0% of poorly differentiated adenocarcinoma cases, 100% of undifferentiated-type mucinous adenocarcinoma cases, and 0% of differentiated-type mucinous adenocarcinoma cases.
Mode of Growth In The Invasive Area of Submucosal Carcinoma (Table 2)
The number of cases showing each growth pattern and the percentage of cases involving lymph node metastasis within each growth pattern were 25 expansive type (0% lymph node metastasis), five infiltrating type (20% lymph node metastasis), 60 mixed type (6.7% lymph node metastasis), 20 predominant expansive type (5.0% lymph node metastasis), and 30 predominant infiltrating type (23.3% lymph node metastasis).
Structural Atypia in the Invasive Area of Submucosal Carcinoma (Table 3)
Cribriform-type structural atypia was observed in 43 cases (30.7%). The percentage of lymph node metastasis in cases with cribriform-type structural atypia was 20.9%(nine cases), whereas in the absence of cribriform-type structural atypia, it was 4.1% (four cases). Dendritic-type structural atypia was observed in 43 cases (30.7%). The percentage of lymph node metastasis in cases with dendritic-type structural atypia was 11.6% (five cases), whereas in the absence of dendritic-type structural atypia, it was 8.2% (eight cases).
Bud-like Structure (Table 3)
A bud-like structure was observed in 84 cases (60.0%). The percentage of lymph node metastasis in cases with a bud-like structure was 15.5% (13 cases), whereas in the absence of a bud-like structure, it was 0% (0 cases).
Lymphoid infiltration in the Invasive Area of Submucosal Carcinoma (Table 3)
Lymphoid infiltration was observed in 73 cases (52.1%). The percentage of lymph node metastasis in cases of lymphoid infiltration was 1.4% (one case), whereas in those without lymphoid infiltration, it was 17.9% (12 cases).
Lymphatic Permeation and Depth of Lymphatic Permeation (Table 4)
Lymphatic permeation was observed in 47 cases (34%). The percentage of lymph node metastasis in cases with lymphatic permeation was 26% (12 cases), whereas in those without lymphatic permeation, it was 1% (one case). The mean depth of lymphatic permeation in cases of cancer with lymph node metastasis was 3.72 mm (minimum, 2.1 mm), and in cases of cancer with no lymph node metastasis, it was 1.03 mm.
Venous Permeation and Depth of Venous Permeation (Table 4)
Venous permeation was observed in 16 cases (11%). The percentage of lymph node metastasis in cases with venous permeation was 31% (five cases), whereas in those without venous permeation, it was 7% (eight cases). The mean depth of venous permeation in cases of cancer with lymph node metastasis was 3.13 mm (minimum, 1.8 mm), and in cases of cancer with no lymph node metastasis, it was 1.11 mm.
Statistical Analysis
Univariate logistic regression analysis showed that the depth of submucosal invasion, cribriform-type structural atypia, absence of lymphoid infiltration, lymphatic permeation, and venous permeation were statistically significant as risk factors for lymph node metastasis (Table 5).
Multivariate logistic regression analysis showed that the important risk factors of lymph node metastasis included, in decreasing order, lymphatic permeation, absence of lymphoid infiltration, cribriform-type structural atypia, venous permeation, and depth of submucosal invasion (Table 5).
When cases were divided into the group in which submucosal invasion is deep on the boundary of 2.5 mm (about 2 mm) and the group in which submucosal invasion is shallow, the odds ratio of depth of submucosal invasion calculated with univariate logistic regression analysis for the lymph node metastasis indicated the highest value (ie, the risk of lymph node metastasis increases most when the depth of submucosal invasion grows more than 2 mm). Similarly, when cases were divided into the group in which the depth of lymphatic permeation is deep on the boundary of 2.2 mm (about 2 mm) and the group in which the depth of lymphatic permeation is shallow, the odds ratio of depth of lymphatic permeation calculated with univariate logistic regression analysis for the lymph node metastasis indicated the highest value (ie, the risk of lymph node metastasis increases most when the depth of lymphatic permeation grows more than 2 mm).
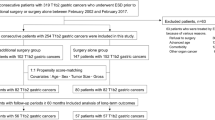
The pathologic criteria (algorithm) of the prediction of lymph node metastasis, based on these results, for additional colecotmy after endoscopic resection of submucosal invasive cancer of the colorectum is presented in Figure 5. If our criteria had been applied to resection of the colon in the 140 cases in this study, 47 cases showed lymphatic permeation; 13 of them revealed deep lymphatic permeation, and would have undergone additional colectomy. In addition, 54 cases in 127 with shallow lymphatic permeation or without lymphatic permeation showed no lymphoid infiltration; 31 of them revealed deep invasion and/or cribriform-type structural atypia, and would have undergone additional colectomy. Moreover, six cases in the 96 remainder showed venous permeation and would have undergone additional colectomy. Consequently, only 50 patients (including all 13 with lymph node metastasis) would have undergone additional colectomy, 37 of whom would have actually been overtreated. Applying the criteria of Haggit et al1 and Haggit2 (Level 4 invasion), 130 of 140 patients would have undergone additional colectomy (Table 6). The sensitivity, specificity, positive and negative predictive value, and overall accuracy of these criteria are shown in Table 6.
Case Presentation
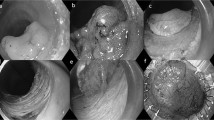
Case 1: Carcinoma with lymph node metastasis (Figure 6).
Carcinoma with lymph node metastasis. (a) Depth of invasion is 9.0 mm. Histological examination in the invasive area of submucosal carcinoma shows moderately differentiated adenocarcinoma. No lymphoid infiltration is seen. Lymphatic permeation is present (arrow), and venous permeation is absent. (b) Cribriform-type structural atypia is shown. (c) Lymphatic permeation is present, and the depth of lymphatic permeation is 8.5 mm (deep lymphatic permeation).
Case 2: Carcinoma without lymph node metastasis (Figure 7).
Carcinoma without lymph node metastasis. (a) Depth of invasion is 1.38 mm. Histological examination in the invasive area of submucosal carcinoma shows well differentiated adenocarcinoma. Lymphatic permeation and venous permeation is absent. (b) Dendritic-type structural atypia is present. (c) Lymphoid infiltration is shown.
Discussion
In 1985, Haggitt et al1 and Haggitt2 proposed a four-level classification system for polyps with invasive carcinoma based on the depth of invasion and reported Level 4 invasion to be an important clinical prognostic factor. Level 4 involves carcinoma invading into the submucosa of the bowel wall below the stalk of the pedunculated lesion. By definition, then, all sessile lesions with invasion are Level 4 lesions. In our present study, 130 lesions qualified as such Level 4. Nivatvongs et al5 have listed Level 4 invasion as a risk factor for lymph node metastasis and advocated Level 4 invasion as an indication for additional colectomy with lymph node resection after endoscopic resection of submucosal invasive colorectal cancer. Since they5 also reported that only 10% of cases of Level 4 submucosal tumor invasion had metastasized to the lymph nodes, it appears that applying the above Nivatvongs’ criteria to resection of the colon would constitute overtreatment in 90% of patients who undergo additional surgery. Therefore, it is necessary that more accurate pathologic criteria be established for additional colorectal resection. Towards this goal, we investigated and analyzed pathologic factors related to lymph node metastasis of submucosal invasive cancer of the colorectum. From univariate analysis, the depth of submucosal invasion, cribriform type structural atypia, lymphoid infiltration, lymphatic permeation, and venous permeation were statistically significant as risk factors for lymph node metastasis. Multivariate analysis indicated that the important risk factors for lymph node metastasis included, in decreasing order, lymphatic permeation, absence of lymphoid infiltration, cribriform-type structural atypia, venous permeation, and depth of submucosal invasion.
Many investigators1, 2, 5, 6, 11 agree that the depth of a submucosal invasion is an important risk factor for lymph node metastasis. We estimated the depth, width, and area of submucosal invasion as an index of the degree of submucosal invasion. However, univariate analysis revealed that the only significant risk factor for lymph node metastasis was the depth of invasion. When comparing the group in which submucosal invasion is deep on the boundary of 2.5 mm (about 2 mm) and the group in which submucosal invasion is shallow, the odds ratio was highest for the deep submucosal invasion to be associated with lymph node metastasis. The odds ratio we obtained for deep submucosal invasion suggests that submucosal invasion of 2 mm or more is a risk factor for the lymph node metastasis.
According to previous reports, moderately or poorly differentiated adenocarcinoma 3, 7, 12, 13, and a bud-like structure9 in submucosal invasive areas are risk factors for lymph node metastasis. Although our data trends were similar, these factors did not show statistical significance in our study. Moreover, many investigators 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15 list mucinous adenocarcinoma as a risk factor for lymph node metastasis. In this study, mucinous adenocarcinoma was considered as two types, one composed of undifferentiated nontubular carcinoma (signet ring cell carcinoma in the majority) and one composed of differentiated tubular adenocarcinoma. Lymph node metastasis was not seen with the latter type, but the rate of lymph node metastasis was very high with the former type. Classification of mucinous adenocarcinoma into these two subgroups, then, appears to be very useful since the risk for lymph node metastasis was shown to be higher for undifferentiated nontubular adenocarcinoma than for differentiated tubular adenocarcinoma.
We classified structural atypia of invasive cancer areas into cribriform type and dendritic type, and we examined the types for risk of lymph node metastasis. Although we expected that the risk of lymphatic invasion in the dendritic type would be greater, only the cribriform type showed statistical significance as a risk factor for lymph node metastasis.
Since carcinoma with lymphoid infiltration is seldom accompanied by lymph node metastasis, it is considered a cancer with a good prognosis.16, 17 Lymphoid infiltration is thought to suppress the growth and invasion of cancer. In the digestive tract, carcinoma with lymphoid infiltration is often reported in the stomach,16, 17 and less often in the large intestine. Lymphoid infiltration is also often observed in the area of colorectal cancer invasion, although less is seen in carcinoma with lymphoid infiltration. We examined the relation between lymphoid infiltration in the colorectal cancer invasion area and lymph node metastasis. The incidence of lymph node metastasis in cases with lymphoid infiltration was lower than that in cases without lymphoid infiltration, and an absence of lymphoid infiltration correlated significantly with lymph node metastasis in both univariate and multivariate analysis. This suggests that lymphoid infiltration is an important inhibition factor for lymph node metastasis.
Lymph node metastasis is caused by the permeation of cancer cells in the lymphatic duct; it follows, then, that lymphatic permeation could be the greatest risk factor for lymph node metastasis.1, 7, 18 Since only 26% of submucosal invasive colorectal cancers with lymphatic permeation show metastasis to the lymph nodes, use of lymphatic permeation as an indicator of lymph node involvement would result in about 75% of patients undergoing unnecessary resection of the lymph nodes. Thus, we examined the relation between lymphatic distance and lymph node metastasis with a view to decrease overtreatment. When comparing the group in which the depth of lymphatic permeation is deep on the boundary of 2.2 mm (about 2 mm) and the group in which the depth of lymphatic permeation is shallow, the odds ratio was highest for the deep depth of lymphatic permeation to be associated with lymph node metastasis. This suggests that the depth of lymphatic permeation of 2 mm or more is a risk factor for lymph node metastasis.
The rate of lymph node metastasis in cases showing venous permeation was high at 31 %, and with univariate analysis, venous permeation was found to be significantly related to lymph node metastasis. Owing to the low frequency of cases showing venous permeation, however, its importance as a risk factor for lymph node metastasis was lessened with significant multivariate analysis. Since with staining elastic fibers, venous permeation can be more objectively evaluated than lymphatic permeation, venous permeation may indeed be an important prognostic factor for lymph node metastasis.
The pathologic criteria, based on our results, for additional colectomy after endoscopic resection of submucosal invasive cancer of the colorectum are presented in Figure 5. If these criteria of ours had been applied to resection of the colon in the 140 cases in this study, only 50 patients (including all 13 with lymph node metastasis) would have undergone additional colectomy, 37 of whom would have actually been overtreated. On the other hand, applying the criteria of Haggit et al.1 Haggit2 or Nivatvongs et al5, 130 of 140 patients would have undergone additional colectomy, 117 of whom would have been overtreated. Both specificity and over all accuracy of our criteria showed higher value than the criteria of Haggit et al. Therefore, the indication criteria that we present for additional colectomy after endoscopic resection of submucosal invasive cancer of the colorectum enable greater accurate selection of patients who will undergo further surgical treatment after endoscopic resection.
References
Haggitt RC, Glotzbach RE, Soffer EE, et al. Prognostic factors in colorectal carcinomas arising in adenomas: implications for lesions removed by endoscopic polypectomy. Gastroenterology 1985;89:328–336.
Haggitt RC . Management of the patient with Carcinomas in an adenoma. Prog Clin Biol Res 1988;279:89–99.
Coverlizza S, Risio M, Ferrari A, et al. Colorectal adenomas containing invasing carcinoma. Cancer 1989;64:1937–1947.
Kitamura K, Taniguchi H, Yamaguchi T, et al. Clinical outcome of surgical treatment for invasive early colorectal cancer in Japan. Hepatogastroenteroly 1997;44:108–115.
Nivatovongs S, Rojanasakul A, Reiman HL, et al. The risk of lymph node metastasis in colorectal polyp with invasive carcinoma. Dis Colon Rectum 1991;34:323–328.
Shatney CH, Lober PH, Gilvertson VA, et al. The treatment of pedunculated adenomatous colorectal polyps with focal cancer. Surg Gynecol Obset 1974;139:845–850.
Tanaka S, Haruma K, Teixeria CR, et al. Endoscopic treatment of submucosal invasive colorectal carcinoma with special reference to risk factors for lymph node metastasis. J Gastroenterol 1995;30:710–717.
Jass JR (ed). In collaboration with pathologists in nine countries. Histological typing of intestinal tumours. In: World Health Organization International Histological Classification of Tumours, 2nd edn. Springer-Verlag: Berlin, Heiderberg New York, London, Paris, Tokyo, and Hong Kong, 1981.
Hase K, Shatney C, Johnson D, et al. Prognostic value of tumor ‘budding’ in patients with colorectal cancer. Dis Colon Rectum 1993;36:627–635.
Statview (computer program). Version 5.0. Berkeley, CA, USA. Abacus Concepts, 1998.
Shatney CH, Lober PH, Gilvertson V, et al. Management of focally malignant pedunculated adenomatous colorectal polyps. Dis Colon Rectum 1976;19:334–341.
Morson BC, Whiteway JE, Jones EA, et al. Histopathology and prognosis of malignant colorectal polyp treated by endoscopic polypectomy. Gut 1984;35:437–444.
Volk EE, Goldblum JR, Petras RE, et al. Management and outcome of patients with invasive carcinoma arising in colorectal polyps. Gastroenterology 1995;109:1801–1807.
Consorti F, Lorenzotti A, Midiri G, et al. Prognostic significance of mucinous carcinoma of colon and rectum: A prospective control study. J Surg Oncol 2000;73:70–74.
Suma KS, Nirmala V . Mucinous component in colorectal carcinoma–prognostic significance: a study in a South Indian population. J Surg Oncol 1992;51:60–64.
Lertprasetsuke N, Tsutsumi Y . Gastric carcinoma with lymphoid stroma. Virchow Arch A Pathol Anat 1989;414:231–241.
Watanabe H, Enjyoji M, Imnai T . Gastric carcinoma with lymphoid stroma. Its morphologic characteristic and prognostic correlation. Cancer 1976;38:232–243.
Minsky BD, Miles C, Rich TA, et al. Lymphatic vessel invasion as an independent prognostic factor for survival in colorectal cancer. Int J Radiat Oncol Biol Phys 1989;17:311–318.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Egashira, Y., Yoshida, T., Hirata, I. et al. Analysis of pathological risk factors for lymph node metastasis of submucosal invasive colon cancer. Mod Pathol 17, 503–511 (2004). https://doi.org/10.1038/modpathol.3800030
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.3800030
Keywords
This article is cited by
-
Multi-center study on predicting breast cancer lymph node status from core needle biopsy specimens using multi-modal and multi-instance deep learning
npj Breast Cancer (2023)
-
A proposal for grading the risk of lymph node metastasis after endoscopic resection of T1 colorectal cancer
International Journal of Colorectal Disease (2023)
-
Composite scoring system and optimal tumor budding cut-off number for estimating lymph node metastasis in submucosal colorectal cancer
BMC Cancer (2022)
-
Prediction of lymph node metastasis in early colorectal cancer based on histologic images by artificial intelligence
Scientific Reports (2022)
-
Utility of artificial intelligence with deep learning of hematoxylin and eosin-stained whole slide images to predict lymph node metastasis in T1 colorectal cancer using endoscopically resected specimens; prediction of lymph node metastasis in T1 colorectal cancer
Journal of Gastroenterology (2022)