Abstract
To investigate the role of P. aeruginosa virulence factors in the repair of human airway epithelial cells (HAEC) in culture, we evaluated the effect of stationary-phase supernatants from the wild-type strain PAO1 on cell migration, actin cytoskeleton distribution, epithelial integrity during and after repair of induced wounds, and the balance between matrix metalloproteinases (MMP) and their tissue inhibitors (TIMP). PAO1 supernatant altered wound repair by slowing the migration velocity in association with altered actin cytoskeleton polymerization in the lamellipodia of migrating airway epithelial cells and delaying or inhibiting the restoration of epithelial integrity after wound closure. PAO1 virulence factors overactivated two of the gelatinolytic enzymes, MMP-2 and MMP-9, produced by HAEC during repair. During HAEC repair in the presence of PAO1 virulence factors, enhanced MMP-2 activation was associated with decreased rates of its specific inhibitor TIMP-2, whereas enhanced MMP-9 activation was independent of changes of its specific inhibitor TIMP-1. These inhibitory effects were specific to P. aeruginosa elastase-producing strains (PAO1 and lipopolysaccharide-deficient AK43 strain); supernatants from P. aeruginosa strain elastase-deficient PDO240 and Escherichia coli strain DH5 α had no inhibitory effect. To mimic the effects of P. aeruginosa, we further analyzed HAEC wound closure in the presence of increasing concentrations of activated MMP-9 or MMP-2. Whereas increasing concentrations of active MMP-9 accelerated repair, excess activated MMP-2 generated a lower migration velocity. All these data demonstrate that P. aeruginosa virulence factors, especially elastase, may impede airway epithelial wound closure by altering cell motility and causing an imbalance between pro- and activated forms of MMP-2.
Similar content being viewed by others
Introduction
Pseudomonas aeruginosa is an opportunistic Gram-negative pathogen, which causes severe pneumonia in cystic fibrosis patients, ventilated patients, and AIDS patients. Once a P. aeruginosa airway infection is established, it is difficult to eradicate the bacteria despite the use of antimicrobial drugs, and P. aeruginosa pneumonia is often associated with mortality in high-risk patients. P. aeruginosa causes airway tissue damage by producing several extracellular and cell-associated virulence factors, [eg, exotoxins, proteases, phospholipases, and lipopolysaccharide (LPS)], many of which play major roles in the toxicity and aggressivity of the bacteria. These virulence factors probably contribute to the colonization of the airways and the pathogenesis of these infections (Azghani et al, 1990; Morihara and Homma, 1985).
After injury, wound repair of the airway epithelium is an important process by which epithelial barrier integrity is restored. The initial mechanisms involved in the wound repair process are cell spreading and migration at the wound edge, followed by cell proliferation (Zahm et al, 1991). The spreading cells acquire a flattened morphology by extending lamellipodia toward the injured area. These morphological changes involve rearrangement of the actin cytoskeleton (Zahm et al, 1991) and enable the cells to move, migrate and close the wound. Between 24 and 48 hours after physical wound closure, epithelial barrier integrity is restored when the junctional complexes become functional (Herard et al, 1996a). In addition, the migrating cells participating in airway epithelial wound closure are also characterized by enhanced expression and activation of matrix metalloproteinases (MMP) (Buisson et al, 1996a; Buisson et al, 1996b), especially gelatinase B (MMP-9), which has been reported to play a crucial role in controlling extracellular matrix degradation during tissue remodeling and wound healing (Legrand et al, 1999).
We previously reported that P. aeruginosa was often associated with remodeled and injured airway epithelium in vitro as well as in vivo (de Bentzmann et al, 1996a, 1996b, 2000). Therefore, the present study was undertaken to evaluate the effects of P. aeruginosa virulence factors. We mainly focused our interest on the effect of supernatants of cultured wild-type, elastase- or LPS-deficient strains of P. aeruginosa on airway cell migration, actin cytoskeleton distribution, and epithelial integrity during and after repair. We also analyzed the effect of these bacterial supernatants on the balance between MMP and their tissue inhibitors (TIMP) during airway epithelial repair.
Results
Effect of P. Aeruginosa Supernatant on the Migration Velocity of Human Airway Epithelial Cells
To evaluate the effect of virulence factors produced by the P. aeruginosa wild-type strain PAO1 on the wound-repair process of human airway epithelial cells (HAEC), injured cultures were incubated with increasing concentrations of PAO1 supernatant. The elastase content of PAO1 corresponded to the range of values detected in airway secretions of cystic fibrosis patients with bronchopulmonary exacerbations (Jaffar-Bandjee et al, 1995). The migration velocity of HAEC at the advancing wound edge, recorded 48 hours after injury and after 24 hours of contact with trypticase soy broth (TSB) or PAO1 supernatant, decreased significantly as the PAO1 supernatant concentration increased. Supernatants from the P. aeruginosa elastase-deficient PDO240 strain and from E. coli strain DH5α had no effect, whereas supernatant of the LPS-deficient AK43 strain induced the same effect as that of the wild-type P. aeruginosa strain (Fig. 1).
Migration velocity of human airway epithelial cells (HAEC) during repair in the presence of bacterial supernatants obtained from wild-type reference strain PAO1, elastase-deficient strain PDO240, lipopolysaccharide (LPS)-deficient strain A43 of P. aeruginosa, and from strain DH5α of E. coli. The migration velocity of repairing HAEC, measured after 24 hours of exposure to bacterial supernatant, was evaluated with video recordings of Hoechst labeled nuclear trajectories. *p < 0.05.
Effect of P. Aeruginosa Supernatant on the Actin Cytoskeleton During Repair
The actin cytoskeleton was immunolabeled in cultures exposed to 0.1, 1, or 10% PAO1 supernatant or 10% TSB. Whereas actin stress fibers were oriented toward the extremities of lamellipodia in migrating HAEC along the advancing wound edge in control cell cultures (Fig. 2A), the actin cytoskeleton was depolymerized, and stress fibers were not seen (Fig. 2B) after 24 hours of contact with 10% PAO1 supernatant. In 10% PAO1 supernatant-treated HAEC cultures, no actin disorganization was observed in confluent areas at a distance from the wound edges, where actin was pericellularly concentrated near lateral membranes. At 0.1 or 1% PAO1 supernatant, no actin disorganization was seen anywhere (data not shown). The potential implication of the effect of elastase on actin depolymerization was further investigated. The same dose-dependent actin disorganization occurred with pure elastase at 3 and 30 μg/ml as that observed with PAO1 supernatant, whereas 0.3 μg/ml of pure elastase had no effect (data not shown).
Reorganization of the actin cytoskeleton during HAEC repair in control (A) and 10% PAO1 supernatant-treated (B) cultures. At the wound margins (arrow), note that actin is distributed into stress fibers oriented toward the extremities of lamellipodia in the control. Note also the disorganization of the actin cytoskeleton and the absence of stress fibers in the presence of 10% PAO1 supernatant. (× 63)
Effect of P. Aeruginosa Supernatant on the Restoration of Epithelial Integrity
Twenty-four hours after wound closure, the restoration of HAEC integrity was investigated by analyzing the diffusion of lanthanum nitrate in repaired HAEC cultures. In control cultures, lanthanum nitrate was located apically on the surface of the cells in the repaired area (Fig. 3A) and at a distance from the repaired area (Fig. 3C). In 10% PAO1 supernatant-treated repaired HAEC cultures, lanthanum nitrate had penetrated into the intercellular spaces of the cells located in the repaired area (Fig. 3B), whereas at a distance from this site and with lower PAO1 supernatant concentrations, it remained excluded from the intercellular spaces (data not shown).
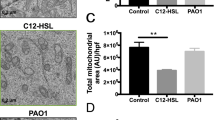
Alteration of HAEC integrity after exposure to PAO1 virulence factors during repair. Functionality of epithelial tight junction barrier after wound closure was investigated by transmission electron microscopy analysis of the diffusion of a low-molecular-weight tracer, lanthanum nitrate. Although junctions were functional, as shown by the apical distribution of the lanthanum precipitate, 24 hours after wound closure in control cultures (A), barrier integrity was still lacking at the center of the closed wound exposed to 10% PAO1 supernatant, as the lanthanum precipitate had diffused into the intercellular spaces (B). At a distance from the wound in control and 10% PAO1 supernatant-treated cultures, the tracer remained apically distributed (C). When complete wound closure could not be fully obtained in the presence of 10% PAO1, virulence factors and HAEC confluence was altered behind the wound edge (D and F) compared with control cell cultures (E and G). (A-C, F and G: × 3000; D and E: × 63).
When wound closure was not complete, cell confluence behind the wound edge was altered (Fig. 3D), with partial loss of cell to cell contact, especially for 10% PAO1 supernatant. However, control cultures or HAEC cultures treated with lower concentrations of PAO1 virulence factors appeared to be optically confluent (Fig. 3E). The loss of cell to cell contact in the repairing area of HAEC cultures treated with 10% PAO1 supernatant was also observed with transmission electron microscopy (TEM) (Fig. 3F); the HAEC remained attached to the collagen I matrix but became separated from adjacent cells and shrank within the repairing area. In matched control cell cultures, HAEC were still connected to the adjacent cells and constituted a confluent cell layer in the repairing area (Fig. 3G). No particular ultrastructural alteration was observed in repairing HAEC cultures treated with the different concentrations of P. aeruginosa supernatants.
Effect of P. Aeruginosa Supernatant on Expression and Activation of MMPs
The effects of 0.1 or 1% PAO1 supernatant on the MMP-2 and MMP-9 expressions and activities were investigated during HAEC wound repair. Zymography of cell culture supernatants collected during HAEC repair is illustrated in Figure 4. The levels of MMP-2 and MMP-9 expression vary considerably from one tissue to another, as previously reported (Buisson et al, 1996b). Although pro-MMP forms (92 and 72 kDa) increased during repair in control cell cultures from all the patients, shifts from pro-forms to activated MMP, (the 84-kDa form for the MMP-9 and the 62-, 59-kDa forms for the MMP-2), were observed in the presence of increasing concentrations of PAO1 supernatant (Fig. 4A). This activation of epithelial MMP during repair was specific to elastase-producing strains, since no pattern of MMP activation was observed when HAEC were incubated with supernatants from the elastase-deficient PDO240 strain (Fig. 4C) or E. coli strain DH5α (Fig. 4D). The same pattern of MMP activation was observed with the P. aeruginosa LPS-deficient AK43 strain (Fig. 4B). The percentages of pro- and activated forms of epithelial MMP during HAEC repair were further analyzed densitometrically. The total MMP-9 increased with time in all cultures, with no significant effect of PAO1 supernatant. In contrast, the respective percentages of pro- and activated (84 kDa) MMP-9 varied markedly with PAO1 supernatant concentration. The higher the concentration, the lower the percentage of pro-MMP-9 and the higher the percentage of activated MMP-9, with earlier activation within 24 hours of contact with 1% PAO1 supernatant (Figs. 4A and 5A). Similarly, total MMP-2 increased with the time of repair in all HAEC cultures. As for MMP-9, the respective percentages of pro- and activated MMP-2 (62 and 59 kDa) dramatically changed as a function of the PAO1 supernatant concentration (Fig. 5B). The higher the concentration, the lower the percentage of pro-MMP-2 and the higher the percentage of activated forms, especially the 59-kDa activated form (Fig. 5C).
Zymographic assessment of the effects of bacterial supernatants on the production and activity of epithelial matrix metalloproteinases (MMP) by HAEC during repair. Primary HAEC cultures were grown to confluence, chemically wounded and allowed to undergo repair for 24 hours. After 24 hours, cultures were exposed to 10% sterile TSB (control) or 0.1, 1 or 10% of bacterial supernatant. Aliquots of every culture supernatant were sampled every 24 hours thereafter and were investigated zymographically on SDS 12% polyacrylamide gels containing 1 mg/ml of porcine skin gelatin run for 6 hours with 36 mA constant current at 4° C. Arrows indicate the positions of MMP-2 and MMP-9 precursors. Supernatants were harvested at the stationary phase of growth after 48 hours of culture from PAO1 (A), LPS− AK43 strain of P. aeruginosa (B), lasB− PDO240 strain of P. aeruginosa (C), and DH5α strain of E. coli (D).
Effect of PAO1 virulence factors on epithelial MMP activation during HAEC repair. HAEC cultures were injured and underwent repair for 24 hours. Thereafter, the medium was replaced daily with 10% TSB (□) or 0.1 (•) or 1% (▪) of PAO1 supernatant obtained at the stationary growth phase. Quantities of activated forms of MMP in zymograms were determined densitometrically and compared with pure human MMP-2. The percentages of activated MMP-9 (A), MMP-2 (B) and 59-kDa MMP-2 were plotted as means and were statistically compared as a function of time of repair with the 24-hour repair values using a paired t test. *p <0.05, **p <0.01
Overactivation of MMP and their Tissue Inhibitors During HAEC Repair
Because we systematically observed an association between the overactivation of epithelial MMP by P. aeruginosa virulence factors and delayed HAEC wound closure, we further analyzed the latter in the presence of increasing concentrations of activated MMP-9 or MMP-2. The concentrations of exogenous MMP added were chosen to cover the range of endogenous activated MMP detected in the presence of PAO1 supernatant. In the presence of increasing concentrations of active MMP-9 (from 0.01 μg/ml to 1 μg/ml), accelerated migration velocities were observed. Although 0.01 μg/ml of activated MMP-2 increased migration velocity by 50% compared with the control, 0.1 μg/ml had no effect on it and 1 μg/ml completely stopped the repair process. For the highest dose of activated MMP-2, the migration velocity fell from 30 to 0 μm/hour within a period of 4 hours. After 24 hours of contact, severe desquamation occurred at the wound margins and to a lesser extent in the confluent non-repairing area. We also examined whether MMP overactivation could be due to an imbalance between MMP-2 and MMP-9 and their specific tissue inhibitors, TIMP-2 and TIMP-1, respectively. The TIMP-2 concentration increased significantly between 24 and 72 hours and between 24 and 120 hours of repair only in control HAEC cultures (p <0.05); no significant increase was observed in any PAO1 supernatant-treated-HAEC cultures (Fig. 6A). At 72 hours and 120 hours, the differences in TIMP-2 concentrations in the supernatants of 0.1 and 1% PAO1 supernatant-treated cell cultures were significantly lower (p <0.001) than that measured in the TSB-treated controls. The TIMP-1 concentration increased between 24 and 72 hours and decreased between 72 and 120 hours of repair in control HAEC cultures. However, these changes were not statistically significant, and treatment of HAEC cultures with 0.1 or 1% PAO1 supernatant did not significantly change the TIMP-1 concentration compared with TSB-treated control HAEC cultures (Fig. 6B).
Effect of P. Aeruginosa Supernatant on MMP and their Inhibitor mRNA Levels
MMP and TIMP mRNA levels were evaluated with semi-quantitative RT-PCR or northern blot done on RNAT of TSB-treated control and 1% PAO1-treated HAEC cultures after 24 hours or 48 hours of contact. In the presence of 1% PAO1, MMP-9, MMP-2, MT1-MMP, TIMP-1 or TIMP-2, mRNA levels in HAEC cultures were unchanged as compared with that recovered in control HAEC cultures for 24 hours and 48 hours, respectively (Fig. 7). This result for MMP was in accordance with unchanged levels of the total (pro + active) form of gelatinases observed at the protein level. No significant up-regulation of MT1-MMP mRNA expression in the presence of 1% of PAO1 supernatant compared with that recovered in control HAEC cultures for 24 or 48 hours of culture was observed, confirming the MT1-MMP-independent MMP-2 activation. The unchanged TIMP mRNA levels in 1% PAO1-treated as compared with TSB-treated control HAEC cultures illustrated the possible TIMP-2 degradation or the absence of effect of P. aeruginosa virulence factors on the gene expression of TIMP-1 after almost 48 hours of contact.
Expression of epithelial MMP and their specific inhibitors during HAEC repair. Ten nanograms of RNAT from HAEC cultures exposed for 24 or 48 hours to 1% PAO1 or control medium (C) were reverse-transcribed. Bands of the expected sizes (212 bp for 28S standard and 225 bp, 261 bp, 221 bp, 208 bp and 176 bp for MMP-2 (A), TIMP-2 (B), MT1-MMP (C), MMP-9 (D), and TIMP-1 (E) were obtained, respectively. While a constant amplification rate was obtained for internal standard (F), no transcriptional regulation was observed for any of the MMP or their respective inhibitors after exposure to PAO1 supernatant.
Discussion
Our results clearly demonstrate that P. aeruginosa virulence factors produced up to the stationary phase of growth were able to alter HAEC wound repair by: (a) slowing migration velocity in association with altered actin-cytoskeleton polymerization in lamellipodia of migrating HAEC; (b) overactivating two of the gelatinolytic enzymes produced by HAEC during repair (MMP-2 and MMP-9); and, (c) delaying or inhibiting the restoration of HAEC integrity after wound closure. Among P. aeruginosa virulence factors, elastase appeared to be the predominant factor responsible for these modifications because supernatants obtained from P. aeruginosa elastase-deficient PDO240 strain and another Gram-negative bacterium (E. coli) had no effect.
HAEC spread and migrate rapidly after injury (Zahm et al, 1997). In the present study, cell migration was altered in a dose-dependent manner by P. aeruginosa virulence factors. One can speculate that these factors are able to interfere with epidermal growth factor (EGF) binding to its receptor and can therefore alter the EGF-dependent up-regulation of fibronectin expression and release during repair (Zahm et al, 1993) and the fibronectin-dependent enhancement of the migration velocity (Herard et al, 1996b). The slowed migration velocity in the presence of P. aeruginosa virulence factors could also be ascribed to a direct alteration of the extracellular matrix components by bacterial proteases or by specialized epithelial MMP. It has been reported that P. aeruginosa elastase and alkaline protease are able to degrade laminin, either in its soluble form or when complexed to the basement membrane (Heck et al, 1986a) and that P. aeruginosa elastase degrades type III and IV collagens (Heck et al, 1986b).
In migrating HAEC at the wound edges, actin cytoskeleton polymerization into stress fibers directed into the lamellipodia, which ended at adhesive contacts with the extracellular matrix, was shown to be essential for cell spreading and migration because cytochalasin B was reportedly able to paralyze the extension of lamellipodia and, consequently, inhibit repair (Zahm et al, 1991). In the presence of high concentrations of PAO1 supernatant, stress fibers and extending lamellipodia were not seen, and lamellipodia retraction progressively appeared with increasing amounts of these virulence factors. This effect has already been ascribed to the exoenzyme S of P. aeruginosa in macrophages (Frithz-Lindsten et al, 1997). In epithelial cells, we reported here that elastase was the bacterial virulence factor responsible for the actin skeleton disorganization. Bacterial toxins, such as exoenzyme S from P. aeruginosa, have been reported to induce disruption of actin microfilaments (Frithz-Lindsten, 1997) or to abolish the formation of actin stress fibers in migrating endothelial cells and the focal adhesion contacts by deactivating Rho proteins (Aepfelbacher et al, 1997).
Virulence factor-induced alterations of migration velocity and actin cytoskeleton essential for wound repair led to delayed epithelial wound closure, which generally occurred 2 days later than in their matched controls and was accompanied by the delayed restoration of epithelial integrity after wound closure. Epithelial integrity with functional tight junctions is usually reestablished within 1–2 days after wound closure (Herard et al, 1996a). As shown herein by the lanthanum nitrate-exclusion assay, even when the wound was completely closed, the junctional integrity of the HAEC was not complete when PAO1 virulence factors were present. P. aeruginosa virulence factors, particularly elastase, have been reported to increase alveolar epithelial permeability by damaging the tight junction-associated proteins ZO-1 and ZO-2 (Azghani et al, 1990, 1993; Azghani, 1996). P. aeruginosa exotoxin A is also able to down-regulate the expression of these two proteins, thus rendering the alveolar epithelial cells unable to restore functional tight junctions (Azghani, 1996). Moreover, in some cases, the epithelial wound healing was incomplete, and wound closure and epithelial junctional integrity were never achieved in the presence of P. aeruginosa virulence factors.
In parallel with the modified cell motility and restoration of functional tight barriers during and after HAEC repair, activation of epithelial MMP-9 and MMP-2 was strongly stimulated 24 hours after the addition of PAO1 supernatant. Although in the repairing control HAEC cultures, MMP-9 and MMP-2 were present in their respective precursor forms (92 kDa and 72 kDa), in the presence of increasing concentrations of PAO1 supernatants, the 84-kDa MMP-9 and the 62- and mostly 59-kDa MMP-2 activated forms became predominant (up to 62% of total MMP-9 and up to 80% of total MMP-2). Moreover, in PAO1-treated wounded HAEC cultures, this MMP-2 activation was found to be MT1-MMP–independent. In cellular extracts obtained from HAEC from wound edges, ie, those which mainly produce MMP-9 during wound healing, the maximal percentage of the activated MMP-9 was never higher than 40%, in parallel with increased total MMP-9 (Buisson et al, 1996a), suggesting that activation of this gelatinase is controlled. MMP-9 is thought to be primarily responsible for cleaning the damaged area and promoting cell migration (Legrand et al, 1999), whereas MMP-2 is considered to play a minor role in wound healing (Buisson et al, 1996a; Yu et al, 1998; Salo et al, 1994). The conversion of pro-MMP-9 and pro-MMP-2 into their activated forms by bacterial products has already been reported (Okamoto et al, 1997; Maeda et al, 1998; Ding et al, 1995). P. aeruginosa elastase, but not alkaline protease, is able to cleave pro-MMP-9 at the Thr90-Phe91 bond near the catalytic domain (Okamoto et al, 1997; Maeda et al, 1998) and cleave pro-MMP-2 to yield its final low-molecular-weight activated 59-kDa form (Matsumoto et al, 1992). We also observed this activation in vitro, after 1 hour of contact, when control wounded HAEC-culture supernatants were directly incubated with PAO1 supernatant. In that situation, both activated MMP-2 and MMP-9 increased during the first 4 hours of incubation (personal data). Pro-MMP-9 has been reported to be fully activated within 3 hours of contact with pure P. aeruginosa elastase (Okamoto et al, 1997). The elastase-deficient P. aeruginosa strain (PDO240) and the Gram-negative E. coli strain DH5α tested in this study did not produce any factor able to activate MMP-9 and MMP-2. The P. aeruginosa LPS-deficient strain retained its ability to activate epithelial MMP-9 and MMP-2. Taken together, these results strongly suggest that P. aeruginosa elastase is the bacterial virulence factor responsible for overactivation of epithelial MMP-9 and MMP-2, despite previous data indicating that LPS could enhance MMP-9 expression and activation (Yao et al, 1997). In our wound repair model, rather than gene up-regulation, P. aeruginosa virulence factors induced MMP-9 and MMP-2 overactivation concomitant with possible TIMP-2 degradation. It is also possible that P. aeruginosa elastase-overactivated MMP-2 itself induced activation of MMP-9, as previously reported (Fridman et al, 1995). We also examined whether overactivation of these two gelatinases could impede HAEC wound closure and re-epithelialization, as earlier reported for MMP-9 in thermal injury of the cornea (Fini et al, 1996; Matsubara et al, 1991). To mimic the overactivation of epithelial MMP, exogenous active MMP-9 was added to HAEC cultures. This led to a dose-dependent accelerated wound closure, whereas a high quantity of activated MMP-2 reproduced the PAO1 supernatant effects on HAEC repair. Taken together, these results suggest that MMP-2 overactivation rather than MMP-9 overactivation is responsible for P. aeruginosa wound-closure inhibition. It was recently reported that the addition of exogenous interstitial collagenases MMP-1 and MMP-13 promoted alveolar type II cell migration by decreasing cell adhesion to type I collagen and cell stiffness (Planus et al, 1999). However, in our study, uncontrolled MMP-2 activation by PAO1 virulence factors, especially elastase, might result in enhanced degradation of the provisional matrix synthesized and deposited under the repairing HAEC, because MMP-2 can degrade fibronectin (Yu et al, 1998) and laminin 5 (Giannelli et al, 1997). Although gelatinases are not the only MMP involved in airway wound repair (Dunsmore et al, 1998), excessive proteolysis due to overactivation of MMP has previously been reported to be responsible for degradation of matrix signals and receptors, thereby leading to disruption of cell-matrix interactions and inhibition of migration (Parks et al, 1998).
This MMP-2 overactivation could explain, in part, the delayed or inhibited HAEC wound healing in the presence of P. aeruginosa virulence factors. The direct activation of MMP-2 in the presence of these factors was not accompanied by TIMP-2 up-regulation. Indeed, TIMP-2 mRNA expression in the cornea remained essentially unchanged throughout a 5-day infection period with P. aeruginosa, with a consistent slight decrease between 12 hours and 1 day after infection (Kernacki et al, 1998). These findings are consistent with the unchanged TIMP-2 protein and mRNA expression observed after 24 or 48 hours of contact between PAO1 supernatant and HAEC cultures compared with untreated ones, in which TIMP-2 expression increased during wound healing. The limited increase of TIMP-2 and the direct proteolytic activation of MMP-2 during wound healing in the presence of P. aeruginosa virulence factors may favor the overactivation of this MMP.
Taken together, these results demonstrate that altered cell motility and an imbalance between pro- and activated forms of MMP-2 and its related tissue inhibitor TIMP-2 are the major events caused by P. aeruginosa virulence factors, particularly elastase, that impede airway epithelial wound closure and cause airway epithelial ulceration. As previously reported for the cornea (Matsubara et al, 1991), our results suggest that during bronchial infections with P. aeruginosa, excessive proteolysis due to the imbalance between epithelial MMP-2 and its inhibitor TIMP-2 and secondary epithelial MMP-9 overactivation might result in enhanced degradation of the airway extracellular matrix and connective tissue, thus leading to airway ulceration. In this way, P. aeruginosa might maintain, during pulmonary exacerbation episodes, optimal conditions for its adherence and survival within airways.
Experimental Procedures
Bacterial Growth Conditions
P. aeruginosa wild-type reference strain PAO1 was used. To further examine the role of P. aeruginosa elastase and LPS, P. aeruginosa mutants PDO240 (lasBΔ9) (McIver et al, 1995) and AK43 (Dasgupta et al, 1994), respectively deficient in elastase production and LPS expression, were also tested. Another Gram-negative bacterium, Escherichia coli (strain DH5α) was also investigated. Bacterial supernatants were prepared by growing bacteria in TSB medium to stationary phase at 37° C for 48 hours under mild agitation. Supernatants of 5 × 109 colony-forming units (CFU)/ml were obtained by centrifugation at 3,000 rpm for 15 minutes at 4° C and filtration through a 0.2 μm filter (Pall Gelman Science, Ann Arbor, Michigan). These supernatants were controlled for their sterility by plating on solid agar gelose. The elastase content of supernatant obtained from PAO1 wild-type reference strain was measured with Western blot technique with reference to purified P. aeruginosa elastase (a generous gift from Professor K. Morihara, Yamaguchi, Japan). The different bacterial supernatants were used after dilution (1:10, 1:100, 1:1,000) in RPMI 1640 culture medium (Seromed, Biochrom KG, Berlin, Germany) supplemented with 10 ng/ml of EGF, 1 μg/ml of insulin, 0.5 μg/ml of hydrocortisone, 1 μg/ml of transferrin, 10 ng/ml of retinoic acid and antibiotics (200 U/ml of penicillin, 200 μg/ml of streptomycin) (complete medium), with the maximal 10% concentration corresponding to a bacterial inoculum of 108 CFU/ml and to an elastase concentration of 2 μg/ml. TSB medium was used as a negative control in all experiments at a dilution of 1:10 in complete medium.
Human Airway Epithelial Cell Cultures
Human airway tissue samples were nasal polyps obtained from 16 patients undergoing nasal polypectomy. Specimens were immediately immersed in RPMI 1640 culture medium containing 20 mm N-2-hydroxyethylpiperazine-N′-2-ethane sulfonic acid (HEPES) and antibiotics (200 U/ml of penicillin and 200 μg/ml of streptomycin). The nasal tissue was then digested with 0.1% pronase E for 12 hours, and the dissociated epithelial cells (106 cells/ml) were seeded in 35-mm culture dishes (Becton Dickinson and Company, Plymouth, United Kingdom) coated with type I collagen (2.5 mg/ml in 0.016 mm acetic acid) prepared from rat-tail tendons according to the technique of Chambard et al (1981). The cells were grown to confluence in complete medium at 37° C in a humidified 5% CO2 atmosphere.
In Vitro Epithelial Wound Induction
After 3 days in culture, when the cells had reached confluence, the culture medium was removed from the culture dish. The epithelial layer was locally injured, as previously described (Herard et al, 1996a) with a 2-μl drop of 1N NaOH that was deposited in the center of the culture dish and immediately neutralized with 1 ml of HEPES-complete medium. The cells that had been in contact with NaOH desquamated from the type I collagen matrix, creating a circular wound about 30 mm2 in area. The wounded culture was then rinsed and incubated at 37° C with 1 ml of complete medium that was changed daily. Twenty-four hours after injury induction, 0.1, 1 or 10% bacterial supernatant or 10% sterile TSB (negative control) in complete medium was added to wounded HAEC cultures, and their supernatants were collected, changed every 24 hours, and frozen for further analysis.
Measurement of Cell Migration Velocity
After 24 hours after incubation of wounded cultures with the different bacterial supernatant concentrations, the migration velocity of cells located at the wound edge was analyzed using a previously described technique (Zahm et al, 1997). Briefly, the HAEC nuclei incorporated a fluorescent dye (Hoechst 33258, Sigma Chemical, St. Louis, Missouri), which was rendered visible by UV illumination. The culture dish was then placed on the heated stage of an inverted microscope equipped with epifluorescence illumination and a low-level video camera (Lhesa SIT 4036, Cergy, Pontoise, France), both driven by a microcomputer. Immediately following ultraviolet excitation, the dishes were filmed every 15 minutes for 1 hour. A software program (Zahm et al, 1997) determined the nuclear displacement trajectories from the digitized images and allowed the quantitation of the cell-migration velocity.
In Situ Immunolabelling of Actin Cytoskeleton
For immunolabelling experiments, dissociated HAEC were seeded on culture dishes coated with type I collagen prepared with 0.25 μg/ml of carbodiimide and injured at cell confluence as above (Herard et al, 1996a). Twenty-four hours later, 10% sterile TSB or 0.1, 1 or 10% PAO1 supernatant was added to the HAEC cultures. After another 24-hour period, the wounded cultures were washed for 10 minutes in 10 mm HEPES buffer containing 100 mm KCl, 3 mm MgCl2, 1 mm CaCl2, pH 6.8, fixed for 1 minute in 4% paraformaldehyde and 0.1% Triton-X-100 in HEPES buffer, then washed for 5 minutes in HEPES buffer, fixed for 8 minutes in 4% paraformaldehyde and 0.1% Triton-X-100 in a 100 mm NaHCO3 buffer (pH 10.5), washed in HEPES buffer for 5 minutes and finally rinsed in 0.1 M phosphate-buffered saline (PBS) for 5 minutes. Then the wounded cultures were incubated for 1 hour with a mouse monoclonal anti-actin antibody (Amersham International, Buckinghamshire, United Kingdom) diluted 1:50 in 0.1 M PBS, and further incubated with a biotin-conjugated goat anti-mouse IgM (Amersham), diluted 1:25 in 0.1 M PBS. The cells were then reacted with streptavidin-fluorescein isothiocyanate for 45 minutes, mounted in glycerol-PBS-[1,4-diazabicyclo[2.2.2]octane] and observed under a Zeiss Axiophot microscope (Zeiss, Le Pecq, France) equipped with epifluorescence illumination.
Permeability to Lanthanum Nitrate
Restoration of epithelial barrier integrity was examined after wound closure by visualizing the diffusion of a low-molecular-weight tracer, lanthanum nitrate, into the intercellular spaces, according to the method described by Revel and Karnovsky (1967). Twenty-four hours after the wound became optically closed, HAEC cultures incubated with bacterial supernatants or TSB were fixed for 1 hour with 2.5% glutaraldehyde in 0.1 M PBS. When wound closure did not occur in the presence of bacterial supernatants, the cultures were fixed when the wounds of their corresponding controls had closed. After several washes with 0.1 M PBS and S-collidine (Sigma)-HCl buffer, pH 7.8, the cells were postfixed for 2 hours at room temperature with 1:1 (v:v) mixture of 0.2 M lanthanum nitrate (Sigma) in S-collidine-HCl buffer and 2% OsO4, pH 7.8. The cultures were then quickly dehydrated in ethanol gradient and embedded in Agar 100 resin (Agar Scientific, Stansted, United Kingdom). Ultrathin sections were obtained on an ultramicrotome (Ultracut E, Leica, Rueil Malmaison, France) and the specimens were observed using a TEM (Hitachi H300, Elexience, Verri res le Buisson, France) at 75 kV after counterstaining with lead citrate and uranyl acetate.
Zymogram Analysis of Gelatinolytic Activities
Wounded HAEC culture supernatants were analyzed zymographically for their MMP contents and activation status in the presence of 10% TSB or 0.1 or 1% bacterial supernatants. With 10% supernatant from PAO1 or elastase-producing mutant strains, the gelatinolytic activity of elastase was so intense that we could not quantify the bands corresponding to epithelial MMP-2 and MMP-9. Cell supernatants were collected every 24 hours during wound repair and stored frozen at −20° C until analysis. Each cell supernatant (24, 48, 72 hours and later if the wound had not closed by 72 hours post-injury) was mixed with Laemmli's buffer (BioRad, Hercules, California) and loaded onto sodium dodecyl sulfate-12% polyacrylamide gels (SDS-PAGE, Witham, Essex, United Kingdom) containing 1 mg/ml of porcine skin gelatin (Sigma) for electrophoresis at 4° C with a constant current of 18 mA per gel for 6 hours. After electrophoresis, the gels were shaken at room temperature in 2% Triton-X-100 in distilled water. The gels were placed in an incubation buffer containing 50 mm Tris-HCl, 5 mm CaCl2 and 0.1% Triton-X-100, pH 7.8, at 37° C for 18 hours. Gels were stained with 1% Coomassie Blue R-250 in a mixture containing 50% methanol and 10% acetic acid in distilled water for 1 hour at room temperature and destained with destaining solution containing 20% methanol and 10% acetic acid in distilled water for 1 hour. The positions of MMP were identified as clear bands against a blue-stained background with reference to purified human gelatinase A (72 kDa) or MMP-2. Optical density of the gelatinolytic bands corresponding to MMP was measured with a densitometer (BioRad), and MMP were quantified by extrapolation from known concentrations (9.2–4, 200 pm) of pure human gelatinase A.
Because MMP overactivation was systematically detected in the supernatants of HAEC cultures treated with PAO1 supernatants, we further investigated the effect of increasing quantities of activated epithelial MMP (0.01–1 μg/ml) on HAEC wound repair. Pure human MMP-2, a generous gift from Professor J. M. Foidart (Liège, Belgium), was activated with p-[aminophenylmercuric] acetate (APMA, Sigma) at 37° C for 5 hours, and pure human active MMP-9 was purchased from Oncogene Research Products (Cambridge, Massachusetts).
TIMP Immunoquantitations
TIMP-1 and TIMP-2 concentrations in the culture supernatants obtained from the different primary HAEC cultures at different times during repair and in the presence of 0.1 or 1% PAO1 supernatant or 10% sterile TSB were determined by ELISA. Human TIMP-1 was detected using the human TIMP-1 ELISA kit (Amersham) and absorbance was read at 450 nm. For TIMP-2 immunoquantitation, after overnight coating with rabbit anti-TIMP-2 antibody (1:750) (a generous gift from Professor J. M. Foidart, Liège, Belgium) at 4° C, microplates were rinsed with 0.1 M PBS-3% BSA-0.05% Tween 20, incubated with 50 μl of samples or pure TIMP-2 (0.31–20 ng/ml) for 2 hours at 37° C. After repeated washes with 0.1 M PBS-0.05% Tween 20, microplates were incubated with chicken anti-TIMP-2 antibody (1:200) (a generous gift from Professor J. M. Foidart) for 2 hours at room temperature, rinsed and incubated with peroxidase-coupled swine anti-chicken antibody (1:10,000) in PBS-BSA-Tween 20 for 1 hour at room temperature. Absorbance was read at 405 nm after incubation of microplates with 2,2′-azino-bis-[ethybenthiazoline-6-sulfonic acid] (ABTS) (Sigma) solution supplemented with H2O2.
RNA Extraction
Total RNA were extracted from repairing HAEC cultures after 24 or 48 hours of contact with 1% PAO1 supernatant or with 1% TSB medium. This bacterial supernatant concentration was the most efficient for activation of MMP. Repairing cells were detached from the collagen I matrix, and RNAT were extracted using the cesium chlorure gradient technique, quantified at 260 nm/280 nm and stored at −80° C until use.
Semi-Quantitative RT-PCR
RT-PCR was performed using 10 ng of total RNA. Forward and reverse primers for human MMP-2, MMP-9, MT1-MMP, TIMP-2, TIMP-1 and 28S were designed as follows: MMP-2 primers [Forward 5′-GGCTGGTCAGTGGCTTGGGGTA-3′, Reverse 5′-AGATCTTCTTCTTCAAGGACCGGTT-3′], MMP-9 primers: [Forward 5′-GACGCGCTGTGTACAC-CCACA-3′, Reverse 5′-GCGGAGATTGGGAACCAG- CTGTA-3′], MT1-MMP primers [Forward 5′-CCATTG- GGCATCCAGAAGAGAGC-3′, Reverse 5′-GGATA- CCCAATGCCCATTGGCCA-3′], TIMP-2 primers [Forward 5′-GTCATCTTGATCTCATAACGCTGG-3′, Reverse 5′-AGCCCATCTGGTACCTGTGGTTCA-3′], TIMP-1 primers [Forward 5′-CATCCTGTTGTTGCT- GTGGCTGAT-3′, Reverse 5′-GGCATCCTCTTGTT- GCTATCACTG-3′], 28S primers [Forward 5′-GT- TCACCCACTAATAGGGAACGTGA-3′, Reverse 5′-GGATTCTGACTTAGAGGCGTTCAGT-3′]. The following cycling parameters were used: MMP-2, MMP-9, MT1-MMP, TIMP-2, TIMP-1, 94° C for 15 seconds, 68° C for 20 seconds, 72° C for 10 seconds, 30 cycles; 28S, 94° C for 15 seconds, 68° C for 20 seconds, 72° C for 10 seconds, 17 cycles.
Northern Blotting Analyses
Each RNA (10 μg) was then analyzed by electrophoresis through 1% agarose gels containing 10% formaldehyde and transferred onto nylon membranes (Amersham). The membranes were then hybridized either with MMP-9, MMP-2, TIMP-1 and TIMP-2 cDNA probes. MMP-2 (1, 500 bp), MMP-9 (1, 700 bp), MT1-MMP (1, 760 bp), TIMP-1 (670 bp), and TIMP-2 (1,035 bp) cDNA were gifts from Dr. G. Murphy (Cambridge, United Kingdom), Dr. G.I. Goldberg (St. Louis, Missouri) and Dr. Y. de Clerck (Los Angeles, California), respectively. Probes were labeled with 32P using a random priming labeling kit (Boehringer-Mannheim Biochemica, Mannheim, Germany). The filters were then exposed for several days at −80° C. Membranes were rehybridized to a ubiquitous 36B4-gene probe which served as a control.
Statistical Analyses
A two-way ANOVA was used to analyze the dose- and time-dependent effects of bacterial supernatants on the repair of wounded HAEC cultures. A paired t test was used to assess the effects of bacterial supernatants on the different parameters during repair for each patient. A p value of < 0.05 was considered to be significant.
References
Aepfelbacher M, Essler M, Huber E, Sugai M, and Weber PC (1997). Bacterial toxins block endothelial wound repair. Arterioscler Thromb Vasc Biol 17:1623–1629.
Azghani AO, Connelly JC, Peterson BT, Gray LD, Collins MC, and Johnson AR (1990). Effects of Pseudomonas aeruginosa elastase on alveolar epithelial permeability in guinea pigs. Infect Immun 58:433–438.
Azghani AO, Gray LD, and Johnson AR (1993). A bacterial protease perturbs the paracellular barrier function of transporting epithelial monolayers in culture. Infect Immun 61:2681–2686.
Azghani AO (1996). Pseudomonas aeruginosa and epithelial permeability: role of virulence factors elastase and exotoxin A. Am J Respir Cell Mol Biol 15:132–140.
Buisson AC, Zahm JM, Polette M, Pierrot D, Bellon G, Puchelle E, Birembaut P, and Tournier JM (1996a). Gelatinase B is involved in the in vitro wound repair of human respiratory epithelium. J Cell Physiol 166:413–426.
Buisson AC, Gilles C, Polette M, Zahm JM, Birembaut P, and Tournier JM (1996b). Wound-repair-induced expression of stromelysins is associated with the acquisition of a mesenchymal phenotype in human respiratory epithelial cells. Lab Invest 74:658–669.
Chambard M, Gavrion J, and Mauchamp J (1981). Influence of collagen gel on the orientation of epithelial cell polarity: follicle formation from isolated thyroid cells and preformed monolayers. J Cell Biol 91:157–166.
Dasgupta T, de Kievit TR, Masoud H, Altman E, Richards JC, Sadovskaya I, Speert DP, and Lam JS (1994). Characterization of lipopolysaccharide-deficient mutants of Pseudomonas aeruginosa derived from serotypes O3, O5 and O6. Infect Immun 62:809–817.
de Bentzmann S, Mongodin E, Roger P, and Puchelle E (2000). Bacterial adherence to airway epithelium. Eur Respir Rev (In press).
de Bentzmann S, Plotkowski MC, and Puchelle E (1996a). Receptors in the Pseudomonas aeruginosa adherence to injured and repairing airway epithelium. Am J Respir Crit Care Med 154:S155–S162.
de Bentzmann S, Roger P, and Puchelle E (1996b). Pseudomonas aeruginosa adherence to remodeling respiratory epithelium. Eur Respir J 9:2145–2150.
Ding Y, Uitto VJ, Firth J, Salo T, Haapasalo M, Konttinen YT, and Sorsa T (1995). Modulation of host matrix metalloproteinases by bacterial virulence factors relevant in human periodontal diseases. Oral Dis 1:279–286.
Dunsmore SE, Saarialho–Kere UK, Wilson CL, Mastrisian LM, Wergus HG, and Parks WC (1998). Matrilysin expression and function in airway epithelium. J Clin Invest 102:1321–1331.
Frithz-Lindsten E, Du Y, Rosqvit R, and Forsberg A (1997). Intracellular targeting of exoenzyme S of Pseudomonas aeruginosa via type III-dependent translocation induces phagocytosis resistance, cytotoxicity, and disruption of actin microfilaments. Mol Microbiol 25:1125–1139.
Fini E, Parks WC, Rinehart WB, Girard MT, Matsubara M, Cook JR, West-Mays JA, Sadow PM, Burgeson RE, Jeffrey JJ, Raizman MB, Krueger RR, and Zieske JP (1996). Role of matrix metalloproteinases in failure to re-epithelialize after corneal injury. Am J Pathol 149:1287–1302.
Fridman R, Toth M, Pena D, and Mobashery S (1995). Activation of progelatinase B (MMP-9) by gelatinase A (MMP-2). Cancer Res 55:2548–2555.
Giannelli G, Falk-Marzillier J, Schiraldi O, Stetler-Stevenson WG, and Quaranta V (1997). Induction of cell migration by matrix metalloprotease-2 cleavage of laminin-5. Science 277:225–228.
Heck LW, Morihara K, and Abrahamson DR (1986a). Degradation of soluble laminin and depletion of tissue-associated basement membrane laminin by Pseudomonas aeruginosa elastase. Infect Immun 54:149–153.
Heck LW, Morihara K, McRae WB, and Miller EJ (1986b). Specific cleavage of human type III and IV collagens by pseudomonas elastase. Infect Immun 51:115–118.
Herard AL, Zahm JM, Pierrot D, Hinnrasky J, Fuchey C, and Puchelle E (1996a). Epithelial barrier integrity during in vitro wound repair of the airway epithelium. Am J Respir Cell Mol Biol 15:624–632.
Herard AL, Pierrot D, Hinnrasky J, Kaplan H, Sheppard D, Puchelle E, and Zahm JM (1996b). Fibronectin and its α5β1-integrin receptor are involved in the wound-repair process. Am J Physiol (Lung Cell Mol Physiol) 15:L726–L733.
Jaffar-Bandjee MC, Lazdunski A, Bally M, Carr re J, Chazalette JP, and Galabert C (1995). Production of elastase, exotoxin A, and alkaline protease in sputa during pulmonary exacerbation of cystic fibrosis in patients chronically infected by Pseudomonas aeruginosa. J Clin Microbiol 33:924–929.
Kernacki KA, Goebal DJ, Poosch MS, and Hazlett L (1998). Early TIMP gene expression after corneal infection with Pseudomonas aeruginosa. Investig Ophtalmol Vis Sci 39:331–335.
Legrand C, Gilles C, Zahm JM, Polette M, Buisson AC, Kaplan H, Birembaut P, and Tournier JM (1999). Airway epithelial cell migration dynamics: MMP-9 role in cell-extracellular matrix remodeling. J Cell Biol 146:517–522.
Maeda H, Okamoto T, and Akaike T (1998). Human matrix metalloprotease activation by insults of bacterial infection involving proteases and free radicals. Biol Chem 379:193–200.
Matsubara M, Zieske J, and Fini ME (1991). Mechanism of basement membrane dissolution preceding corneal ulceration. Invest Ophtalmol Vis Sci 32:92–107.
Matsumoto K, Shams NBK, Hanninen LA, and Kenyon KR (1992). Proteolytic activation of corneal matrix metalloproteinase by Pseudomonas aeruginosa. Curr Eye Res 11:1105–1109.
McIver KS, Kessler E, Olson JC, and Ohman DE (1995). The elastase propetide functions as an intramolecular chaperone required for elastase activity and secretion in Pseudomonas aeruginosa. Mol Microbiol 18:877–889.
Morihara K and Homma JY (1985). Pseudomonas proteases. In: Holder IA, editor: Bacterial enzymes and virulence. Boca Raton: CRC Press, 41–79.
Okamoto T, Akaike T, Suga M, Tanase S, Horie H, Miyajima S, Ando M, Ichinose Y, and Maeda H (1997). Activation of human matrix metalloproteinases by various bacterial proteinases. J Biol Chem 272:6059–6066.
Parks WC, Sudbeck BD, Doyle GR, and Saariahlo-Kere UK (1998). Matrix metalloproteinases in tissue repair. In: Parks WC, and Mecham RP, editors: Matrix Metalloproteinases. San Diego: Academic Press, 263–299.
Planus E, Galiacy S, Matthay H, Laurent V, Gavrilovic J, Murphy G, Clérici C, Iasbey D, Lafuma C, and d'Ortho MP (1999). Role of collagenase in mediating in vitro alveolar epithelial wound repair. J Cell Sci 112:243–252.
Revel JP, and Karnovsky MJ (1967). Hexagonal array of subunits in intercellular junctions of the mouse heart and liver. J Cell Biol 33:C7–C12.
Salo T, Mäkelä M, Kylmäniemi M, Autio-Harmainen H, and Larjava H (1994). Expression of matrix metalloproteinase-2 and -9 during early human wound healing. Lab Invest 70:176–182.
Yao PM, Maitre B, Delacourt C, Buhler JM, Harf A, and Lafuma C (1997). Divergent regulation of 92-kD gelatinase and TIMP-1 by HBECs in response to IL-1β and TNF-α. Am J Physiol (Lung Cell Mol Physiol 17) 273:L866–L874.
Yu AE, Murphy AN, and Stetler-Stevenson WG (1998). 72-kDa Gelatinase (Gelatinase A): structure, activation, regulation, and substrate specificity. In: Parks WC, and Mecham RP, editors: Matrix Metalloproteinases. San Diego: Academic Press, 85–113.
Zahm JM, Chevillard M, and Puchelle E (1991). Wound repair of human surface respiratory epithelium. Am J Respir Cell Mol Biol 5:242–248.
Zahm JM, Pierrot D, and Puchelle E (1993). Epidermal growth factor promotes wound repair of human respiratory epithelium. Wound Repair Regen 1:175–180.
Zahm JM, Kaplan H, Herard AL, Doriot F, Pierrot D, Somelette P, and Puchelle E (1997). Cell migration and proliferation during the in vitro wound repair of the respiratory epithelium. Cell Motil Cytoskeleton 37:33–43.
Acknowledgements
The authors thank Dr. Christine Gilles (Liège, Belgium) for her helpful scientific assistance and discussion and Dr. J. M. Tournier for his helpful comments and for teaching us the zymographic techniques. This work was funded by the Association Française de Lutte contre la Mucoviscidose (AFLM).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
de Bentzmann, S., Polette, M., Zahm, JM. et al. Pseudomonas Aeruginosa Virulence Factors Delay Airway Epithelial Wound Repair by Altering the Actin Cytoskeleton and Inducing Overactivation of Epithelial Matrix Metalloproteinase–2. Lab Invest 80, 209–219 (2000). https://doi.org/10.1038/labinvest.3780024
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1038/labinvest.3780024
This article is cited by
-
Klotho modulates ER-mediated signaling crosstalk between prosurvival autophagy and apoptotic cell death during LPS challenge
Apoptosis (2019)
-
Molecular analysis of Pseudomonas aeruginosa isolated from clinical, environmental and cockroach sources by ERIC-PCR
BMC Research Notes (2018)
-
Clove Bud Oil Modulates Pathogenicity Phenotypes of the Opportunistic Human Pathogen Pseudomonas aeruginosa
Scientific Reports (2018)
-
Predatory bacteria are nontoxic to the rabbit ocular surface
Scientific Reports (2016)
-
Microbial inhibition of oral epithelial wound recovery: potential role for quorum sensing molecules?
AMB Express (2015)