Abstract
In the era of intravascular approaches for regenerative cell therapy, the underlying mechanisms of stem cell migration to non-marrow tissue have not been clarified. We hypothesized that next to a local inflammatory response implying adhesion molecule expression, endothelial nitric oxide synthase (eNOS)-dependent signaling is required for stromal- cell-derived factor-1 alpha (SDF-1α)-induced adhesion of c-kit+ cells to the vascular endothelium. SDF-1α/tumor necrosis factor-alpha (TNF-α)-induced c-kit+-cell shape change and migration capacity was studied in vitro using immunohistochemistry and Boyden chamber assays. In vivo interaction of c-kit+ cells from bone marrow with the endothelium in response to SDF-1α/TNF-α stimulation was visualized in the cremaster muscle microcirculation of wild-type (WT) and eNOS (−/−) mice using intravital fluorescence microscopy. In addition, NOS activity was inhibited with N-nitro-L-arginine-methylester-hydrochloride in WT mice. To reveal c-kit+-specific adhesion behavior, endogenous leukocytes (EL) and c-kit+ cells from peripheral blood served as control. Moreover, intercellular adhesion molecule-1 (ICAM-1) and CXCR4 were blocked systemically to determine their role in inflammation-related c-kit+-cell adhesion. In vitro, SDF-1α enhanced c-kit+-cell migration. In vivo, SDF-1α alone triggered endothelial rolling—not firm adherence—of c-kit+ cells in WT mice. While TNF-α alone had little effect on adhesion of c-kit+ cells, it induced maximum endothelial EL adherence. However, after combined treatment with SDF-1α+TNF-α, endothelial adhesion of c-kit+ cells increased independent of their origin, while EL adhesion was not further incremented. Systemic treatment with anti-ICAM-1 and anti-CXCR4-monoclonal antibody completely abolished endothelial c-kit+-cell adhesion. In N-nitro-L-arginine-methylester-hydrochloride-treated WT mice as well as in eNOS (−/−) mice, firm endothelial adhesion of c-kit+ cells was entirely abrogated, while EL adhesion was significantly increased. The chemokine SDF-1α mediates firm adhesion c-kit+ cells only in the presence of TNF-α stimulation via an ICAM-1- and CXCR4-dependent mechanism. The presence of eNOS appears to be a crucial and specific factor for firm c-kit+-cell adhesion to the vascular endothelium.
Similar content being viewed by others
Main
The importance of chemokines for stem cell trafficking to injured tissue has been extensively discussed in the recent past; however, the underlying molecular mechanisms for stem cell directional migration and adhesion outside the bone marrow remain unclear.1 Stromal cell-derived factor-1 (SDF-1α) is a chemokine that can direct the homing of human CD34+ CD38LOW and murine Sca-1+ Thy-1+ cells back to the bone marrow. SDF-1α also plays a chemoattractant role for other leukocytes2, 3, 4, 5, 6 SDF-1α is crucial for progenitor cell trafficking not only to and from the bone marrow, but is also implicated in the migration to injured peripheral organs. SDF-1α has shown to enhance integrin-dependent adhesion of endothelial progenitor cells and interferes with endothelial progenitor cell differentiation and angiogenesis in ischemic hind limb models.7 The upregulation of SDF-1α in infarcted myocardium, for instance, is closely related to the recruitment of circulating stem cells and improvement of cardiac function.8, 9 However, Abbott et al10 found that SDF-1α alone is not sufficient to recruit stem cells to the ischemic heart. The involvement of SDF-1α-related cofactors for the early events in extravasation of transplanted c-kit+ bone marrow cells, however, is not clearly defined. Recently it was shown by Rüster et al11 in vitro and partly in vivo that mesenchymal stem cells interact with endothelial cells through P-selectin-mediated rolling and VCAM-1/VLA-1-mediated firm adhesion. Tumor necrosis factor-alpha (TNF-α)-induced firm leukocyte adhesion in the cremaster muscle, however, is mediated by an increase of local intercellular adhesion molecule-1 (ICAM-1) expression.12, 13
A previous report demonstrated that the nitric oxide (NO) pathway can modulate endothelial progenitor cell activity and plays a critical role in both post-injury angiogenesis and normal endothelial cell maintenance in the murine retina.14 Furthermore, therapeutically induced endothelial NO availability improves progenitor cell mobilization, cardiac neovascularization, LV dysfunction, interstitial fibrosis, and survival after myocardial infarction in mice.15 Recently, Sasaki and co-workers showed the crucial specific involvement of NO-producing enzymes in the migratory capacity of bone marrow mononuclear cells in vivo.16
In order to study the microenvironment that is essential for SDF-1α-mediated c-kit+ cell interaction with the vascular endothelium in non-marrow tissue, we examined c-kit+ cell shape change and migration in vitro and c-kit+ cell–endothelium interactions in cremaster muscle microvessels using intravital fluorescence microscopy. We tested the hypothesis that TNF-α-induced inflammation, most likely including increased ICAM-1 expression, is required for SDF-1α-dependent induction of peripheral c-kit+ cell recruitment in vivo. Owing to the known relevance of NO in stem cell trafficking, we additionally examined its involvement in c-kit+ cell adherence to the endothelium.
MATERIALS AND METHODS
Isolation and Labeling of c-kit+ Cells from Murine Bone Marrow and from Peripheral Blood
C-kit+ cells were isolated from murine (C57BL/6J mice; 8 weeks old) bone marrow and murine peripheral blood after stimulation with 1.3 mg/kg Neulasta® (granulocyte colony-stimulating factor (G-CSF), Amgen®, Thousend Oaks, CA, USA) using magnetic microbeads coated with anti-c-kit monoclonal antibody, Miltenyi Biotec MS columns®, and the MiniMacs® cell separation system (Miltenyi Biotec, Bergisch Gladbach, Germany). Two cell separation cycles were carried out. The purity of the enriched c-kit+ cell product was consistently higher than 95%, confirmed by fluorescent-activated cell sorter (FACS) analysis using PE-conjugated anti-CD117 antibody (Miltenyi Biotec, Bergisch Gladbach, Germany).
Fluorescent-Activated Cell Sorter Analysis of Bone Marrow and Peripheral c-kit Cells
For flow cytometry analysis, cells were incubated for 20 min at 4–8°C with the following antibodies: anti-CD117 PE (clone 3C1; 1:10; Miltenyi Biotec, Bergisch Gladbach, Germany), anti-CXCR4 (clone 2B11; 1:50; Becton Dickinson, Heidelberg, Germany), anti-ICAM-1 (clone 3E2; 1:10; Becton Dickinson, Heidelberg, Germany), anti-P-selectin (clone RB40.34; 1:50; Becton Dickinson, Heidelberg, Germany), and anti-lymphocyte function-associated antigen-1 (LFA-1) (clone GAME-46; 1:50; Becton Dickinson, Heidelberg, Germany). For the indirect staining, polyclonal Alexa Fluor® 488 (1:1000; Invitrogen) was applied. After incubation in antibody, cells were washed with phosphate-buffered saline (PBS)/2 mM EDTA and analyzed by an FACS Calibur flow cytometer (Becton Dickinson, Heidelberg, Germany). Dead cells were excluded via propidium iodide staining. Data analysis was performed with BD CELLQuest software. Histograms of cell number vs logarithmic fluorescence intensity were recorded for 10 000–20 000 cells per sample.
Immunohistochemical Analysis of F-actin and CXCR-4 Expression of c-kit+ Cells Following Incubation with SDF-1α
C-kit+ cells were incubated for 40 h in RPMI 1640 supplemented with 10% FCS in the absence of cytokines or with SDF-1α (50 ng/ml; R&D Systems, Minneapolis, MN, USA). The cells were seeded on glass coverslips coated with 10 μg/cm2 fibronectin (BD Biosciences) and incubated for 2 h at 37°C in 5% CO2. Cells were fixed with 4% paraformaldehyde in PBS for 15 min and permeabilized with 0.1% Triton X-100 in PBS for 10 min. Cells were indirectly immunolabeled with rabbit anti-mouse CXCR4 polyclonal antibody (Chemicon International, Temecula, CA, USA), washed extensively with PBS, and incubated with fluorescein isothiocyanate (FITC)-phalloidin (Molecular Probes) for F-actin staining and goat anti-rabbit Alexa 488 (Molecular Probes). The coverslips were washed extensively and mounted in FluorSave™ (Calbiochem, San Diego, CA, USA). Immunofluorescence signal was imaged using Leica TCS SP2 confocal microscope.
Analysis of c-kit+ Cell Migration against SDF-1α in the Boyden Chamber
In vitro migration assays were performed in 24-well transwell plates with 3 μm pore filters (Costar, Lowell, MA, USA). The filter, which separates the upper and lower compartment of the transwell, was coated with 20 mg/ml of fibronectin (Sigma-Aldrich, Munich, Germany) for overnight at 4°C at a concentration of 20 mg/ml in PBS. Before addition of cells to the upper compartment, the coated transwells were washed three times with assay medium (RPMI 1640 with 0.25% BSA (Sigma). 2 × 104 freshly isolated c-kit+ cells in 1 ml of assay medium were seeded to the upper compartment. A series of 10–600 ng/ml of SDF-1α alone (R&D Systems, Minneapolis, MN, USA) and 200 U/ml TNF-α alone (R&D Systems) in 0.6 ml of assay medium were applied to the lower chamber. Finally, both chemokines SDF-1α and TNF-α were added to the lower compartment to analyze combined chemoattractant activities. After 4 h incubation at 37°C, the cells migrated to the lower compartment were collected and viable cell count was performed using Trypan Blue staining. All experiments were performed in triplicate wells.
Intravital Fluorescence Microscopic Analysis of c-kit+ Cell Interaction with the Venular Endothelium Following SDF-1α and TNFα Stimulation In Vivo
All animal experiments conformed to the Guide for the Care and Use of Laboratory Animals (NIH Publication No. 85–23, revised 1996) and were approved by the local Animal care and use committee. Male wild-type (WT) mice (C57BL/6J) and endothelial nitric oxide synthase (eNOS) (−/−) mice (B6.129P2-Nos3<tm1Unc>) weighing 20–25 g (Charles River, Sulzfeld, Germany) were anesthetized with ketamine (75 mg/kg) and xylazine (25 mg/kg). For intravital microscopy, c-kit+ cells were fluorescently labeled with CFSE (carboxy-fluorescein diacetate succinimidylester, Invitrogen, Carlsbad, CA, USA) according to the manufacturer's protocol. To compare the cellular behavior of c-kit+ cells with the adhesion of circulating endogenous leukocytes (EL) of recipient origin, EL were stained by intravenous injection with 0.1 ml of 1% rhodamine 6G (Sigma-Aldrich, Munich, Germany).
For c-kit+ cell injection, an arterial catheter was inserted retrograde into the left femoral artery. The right cremaster muscle was dissected and prepared for intravital fluorescence microscopy as described before.17, 18 An Axiotech® fluorescence microscope (Zeiss) was modified for epi-illumination and connected to a CCD video camera. For visualization of blood flow, fluorescently labeled dextrane (MW 150 000; rhodamine 6G (background for CFSE-labeled c-kit+ cells) or FITC (background for rhodamine-labeled EL)) was injected. Before cell injection, six postcapillary venules were stochastically defined for later analysis of cellular adherence. In the respective groups, the cremaster muscle was exposed to SDF-1α and/or TNF-α 15 min prior to the first c-kit+ cell injection as described in ‘Experimental groups’ section below. CFSE-labeled c-kit+ cells were administered at 0.4 × 106 cells per injection, with a total of five consecutive injections. C-kit+ cell ‘rolling’ was defined as a more than 50% reduction of cell velocity along the endothelial lining in combination with the typical cellular ‘stick and release’ movements. The rolling c-kit+ were quantified as the number of rolling cells expressed as percentage of all passing cells covering a predefined venular distance during 1 min of observation. Cells exhibiting random brief tethering phenomena were not counted as rolling cells. Firm adhesion was considered when no cell movement was detectable for 30 s. The number of firmly adherent c-kit+ cells was expressed in relation to the calculated endothelial surface of the predefined venules (diameter × length × π) and was expressed as adherent cells/mm2.
Experimental Groups
In control mice, c-kit+ cells were injected under superfusion with PBS (‘control’, n=5). For analysis of SDF-1α, intravital microscopy was preceded by topical administration of 200 μl of SDF-1α (200 ng/ml in PBS) (‘SDF-1α’, n=5). In mice allocated TNF-α alone, superfusion with 200 μl TNF-α (2000 U) was performed (‘TNF-α’, n=5). In addition, both chemokines were administered simultaneously (‘SDF-1α+TNF-α’, n=5). Experiments were performed in WT and eNOS (−/−) animals. To exclude specific endothelial abnormalities in eNOS (−/−) mice, an additional set of experiments was carried out in WT animals following systemic treatment with N-nitro-L-arginine-methylester-hydrochloride (L-NAME) 90 min before the beginning of the experiments (20 mg/kg i.p., Merck, Darmstadt, Germany). Furthermore, WT mice were treated systemically with anti-ICAM-1 (5 mg/kg, Chemicon, Temecula, CA, USA) and anti CXCR4 mAb 12G5 (R&D Systems, Minneapolis, MN, USA; 10 μg/ml in 500 μl of RPMI, i.p. injection) 30 min before the beginning of the experiments. For confirmation of the baseline findings of SDF-1α+TNF-α-mediated c-kit+ cell adhesion and to compare the results from L-NAME-treated WT- and eNOS (−/−) mice, separate experiments for ‘WT control’ (n=5) and ‘WT SDF+TNF’ (n=5) were performed. Furthermore, the group ‘WT control’ and ‘WT SDF+TNF’ was repeated with c-kit+ cells obtained from peripheral blood.
The interaction of EL with the endothelial lining of cremaster muscle postcapillary venules of WT animals was analyzed after treatment with TNF-α and SDF-1 alone or in combination and compared to control animals. To study the role of the activity of endogenous NO-synthases for EL adhesion, WT animals were treated with L-NAME.
Care was taken to provide similar microcirculatory parameters such as blood flow velocity in the experimental groups. Red blood cell velocity profile was determined from intravital microscopy recordings using the line shift method (CapImage Software, Zeintl, Heidelberg, Germany). Microcirculatory analysis also included the determination of vessel diameter and wall shear rates based on the Newtonian definition γ=8 × v/d, were ‘v’ represents the red blood cell velocity divided by 1.6 according to the Baker-Vayland factor19 and ‘d’ represents the individual vessel diameter.
Immunohistochemical Analysis of Endothelial CXCR4 in Murine Cremaster Muscles
Tissue sections of cremaster muscle were fixed with 4% paraformaldehyde in PBS for 20 min. Sections were washed with PBS and incubated with Protein block Reagent (Dako, Denmark) to block unspecific protein-binding sites. Sections were then incubated overnight with antibody rat anti-mouse CXCR4 monoclonal antibody (1:200, BD Bioscience). Sections were washed extensively with PBS, and incubated with secondary antibody donkey-anti-rat IgG Alexa 488 (1:1000, Molecular Probes) and goat-anti-mouse IgG Alexa 568 (1:1000, Molecular Probes). For nuclear staining, sections were incubated with Draq 5 for 20 min, washed extensively and mounted in FluorSave™ (Calbiochem). Immunofluorescence signal was imaged using Leica TCS SP2 confocal microscope.
Statistical Analysis
Data were presented as mean±s.e.m. Statistical analysis between groups was performed using one-way analysis of variance followed by the appropriate post hoc comparison test. A P-value <0.05 was considered to be statistically significant.
RESULTS
Incubation with SDF-1α Causes a Modification of the F-actin Cytoskeleton and a Redistribution of the CXCR-4 Receptor of c-kit+ Cells In Vitro
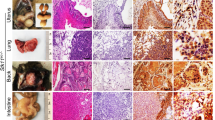
To examine the F-actin polymerization process after stimulation with SDF-1α in vitro, the migrated c-kit+ cells were double stained for CXCR4 and F-actin. There was a strong signal for CXCR4 surface marker at the filopodia in SDF-1α-stimulated c-kit+ cells and a rearrangement of the actin cytoskeleton when compared to control cells. In these cells, F-actin was concentrated mainly at the plasma membrane together with the CXCR-4 protein. In consistence with the in vitro cell migration assay, SDF-1α induced polarization and membrane protrusions in c-kit+ cells (Figure 1).
Confocal laser microscopy analysis F-actin and CXCR-4 protein distribution in c-kit+ cells after stimulation with SDF-1α in vitro. c-kit+ cells were extracted after migration in the Boyden chamber assay with and without SDF-1α stimulation. In cells without SDF-1α stimulation, CXCR4 (red fluorescence) and F-actin (green fluorescence) expression was equally distributed along the plasma membrane. After SDF-1α stimulation, a reorganization of the cytoskeleton represented by a modified intracellular F-actin distribution and a concentration of CXCR4 protein at the filopodia (magnification: × 1000).
SDF-1α Alone Induces c-kit+ Cell Migration In Vitro
To analyze the chemoattractant capacity of SDF-1α on c-kit+ cells, we investigated the effects of SDF-1α on the migration of c-kit+ cells in a dose-dependent manner. There was a clear dose–response relationship between percentage of migrated c-kit+ cells and concentration of SDF-1α (Figure 2a). In the control experiments, 6±3% c-kit+ cells migrated spontaneously compared to 40±3% cell migration at 200 ng/ml SDF-1α. TNF-α had a minimal effect on c-kit+ cell migration in vitro in the presence and absence of SDF-1α (Figure 2b).
Quantitative analysis of c-kit+ cell migration in Boyden chamber assays. c-kit+ cells from murine bone marrow were seeded at the upper compartment of Boyden chamber assays with and without SDF-1α in the lower compartment. (a) The migration capacity of c-kit+ cells across the filter in the Boyden chamber is dependent on the concentration of SDF-1α. (b) SDF-1α application alone induced significantly c-kit+ cell migration while addition of TNF- α did not lead to further increase in migration. Data are expressed as mean±SD (*P<0.05 vs control).
In Vivo Interaction of c-kit+ Cells with the Endothelium Occurs Predominantly in Postcapillary Venules
In general, interaction of c-kit+ cells with the vascular endothelium was rare and occurred exclusively in postcapillary venules (diameter: 30–80 μm) but to a different extent in the respective experimental groups. The microcirculatory conditions represented by the blood flow velocity and wall shear rate did not significantly differ between the respective experimental groups (Table 1). In the observed venules, rolling and firmly adherent c-kit+ cells could be clearly quantified in response to chemokine treatment (Figure 3).
Intravital microscopy of c-kit+ cells in a murine cremaster muscle preparation. Intravascular background is visualized by rhodamin-dextran. (a–f) A series of six consecutive images with rolling (black arrows) and firmly adherent (white arrow) carboxy-fluorescein dacetate succinimidylester- labeled c-kit+ cells in the venular vasculature. The recording time is displayed in the right upper corner to demonstrate the slow movement pattern (rolling) and firm adhesion of representative c-kit+ cells on the endothelium.
SDF-1α Alone Enhances Venular Rolling of c-kit+ Cells In Vivo
In vivo, we observed rolling of c-kit+ stem cells using intravital microscopy. We quantitated the percentage of cells with more than 50% reduction of velocity along the endothelial lining. In the PBS-superfused cremaster muscle (‘control’), the fraction of rolling c-kit+ cells was 6±1%. Following local SDF-1α administration, a two-fold increase in c-kit+ cell rolling was detected (P=0.03). In animals treated with TNF-α alone, the fraction of rolling c-kit+ cell was nearly identical to that in control mice. In response to combined treatment with TNF-α and SDF-1α, the fraction of rolling c-kit+ cells was not significantly different compared to c-kit+ cell rolling after exposure to SDF-1α alone (all Figure 4a).
Quantitative analysis of interactions between c-kit+ cell and endothelial cells based on intravital fluorescence microscopic images. (a) The number of rolling c-kit+ cells on venular endothelium (expressed in percentage of all passing cells) in murine cremaster muscles exposed to SDF-1α, TNF-α or a combination of both compared to c-kit+ cell injection without chemokine pretreatment (control). Treatment with SDF-1α alone and the combination of SDF-1α+TNF-α increased percentage of rolling c-kit+ cells. (b) The number of firmly adherent c-kit+ cells per mm2 of venular endothelial lining is significantly increased only after treatment with the combination of SDF-1α+TNF-α. Data are expressed as mean±s.e.m. (*P<0.05 vs control).
SDF-1α Requires Local Stimulation with TNF-α to Induce Firm Endothelial Adhesion of c-kit+ Cells In Vivo
To analyze the role of inflammatory stimulation with TNFα in vivo, we quantified the number of firmly adherent c-kit+ cells on predefined venules following SDF-1α application. To elucidate the presumed selective adhesion behavior of c-kit+ cells, EL adhesion was additionally analyzed.
In the PBS-superfused cremaster muscle (‘control’), the number of firmly adherent c-kit+ cells was 3±1 cells/mm2 (Figure 4b), while the number of firmly adherent EL was 187±38 cells/mm2 (Figure 5). In animals treated with TNF-α alone, the number of firmly adherent c-kit+ cells increased moderately, within the same range as observed after treatment with SDF-1α alone (Figure 4b). In contrast, application of TNF-α alone boosted the number of adherent EL and resulted in a four-fold increase (EL adhesion: 955±145 cells/mm2 in ‘TNF-α’ vs 187±38 cells/mm2 in ‘control’, P=2.02E-06) (Figure 5).
Quantitative analysis of rhodamine-labeled EL–endothelial interactions based on intravital fluorescence microscopic recordings. Number of adherent leukocytes (expressed as cells per mm2 venular endothelium) at endothelium of murine cremaster muscle exposed to SDF-1, TNF-α or a combination of SDF-1 and TNF-α was quantitated. Experiments were performed in WT animals with (open bar) and without (black bar) systemic antagonism of endogenous NO production by L-NAME and compared to controls without local chemokine treatment. Data are expressed as mean±s.e.m. (#P<0.05 vs ‘WT’, *P<0.01 vs ‘WT+L-NAME/control’, °P<0.01 vs ‘WT/control’).
In response to combined treatment with TNF-α and SDF-1α, the number of firmly adherent c-kit+ cells was significantly higher than in response to SDF-1α or TNF-α alone (c-kit+ cell adhesion: 43±13 cells/mm2 in ‘SDF-1α+TNF-α’ vs 8±4 cells/mm2 in ‘SDF-1α’ vs 10±3 cells/mm2 in ‘TNF-α’, P<0.05, each). In fact, stem cell adhesion after these combined tissue stimulation exceeded that of the untreated control mice more than 14-fold (P=0.02) (Figures 4b and 6). In contrast, mature EL adhesion behavior was only slightly changed in venules after the combined stimulation compared with TNF-α treatment alone (Figure 5).
Representative images of firmly adherent CFSE-labeled c-kit+ cells in a murine cremaster muscle preparation. Intravascular background is visualized by rhodamin–dextran. Representative images of control, cells without chemokine pretreatment; superfusion of cremaster muscle with TNF-α; response to superfusion with a combination of SDF-1α and TNF-α. There was a marked increase in the number of firmly adherent c-kit+ cells attached to the venular endothelium after combined treatment with TNF-α and SDF-1. Experiments were performed in WT mice.
Characteristics of c-kit+ (CD117+) Cells from Peripheral Blood and Bone Marrow
The average purity of the c-kit+-enriched cell products was 95.2±4%, with no difference between peripheral blood- and bone marrow-derived cells. Cell viability was consistently higher than 95%. We compared CXCR4, ICAM (CD54), P-selectin (data not shown) and LFA-1 (data not shown) surface expression on c-kit-enriched cell from peripheral blood with that from bone marrow by FACS. The majority of bone marrow and peripheral blood c-kit expressed surface CXCR4. In all, 99.2% of bone marrow c-kit and 99.9% of peripheral blood c-kit+ cells were found to be positive for CXCR4. (Figure 7a, upper panel). The ICAM-1 expression was found to be slightly higher in peripheral blood c-kit cells than in bone marrow c-kit (BM vs PB: 85.6 vs 99.5%) (Figure 7a, lower panel). There were similar surface expression patterns on P-selectin (data not shown) and LFA-1 (data not shown).
Immunophenotyping of c-kit+ (CD117) cells from murine bone marrow and peripheral blood and comparison of in vivo adhesion behavior in response to TNF-α and SDF-1α. (a) Representative flow cytometric analysis of CXCR4 on c-kit+ cells derived from bone marrow and peripheral blood. The shaded histograms show staining with isotype-matched control antibodies, and the open histograms show staining with CXCR4 (upper panel) or ICAM (down panel) antibodies. (b) Quantitative analysis of c-kit+ cells from murine peripheral blood and bone marrow to endothelial cell interactions based on intravital fluorescence microscopy recordings. Experiments were performed in WT mice in response to superfusion with TNF-α and SDF-1α and compared to controls. Data are expressed as mean±s.e.m. (#P<0.05 vs ‘control’, *P<0.05 vs WT).
Adhesion Behavior of c-kit-Positive Cells from Peripheral Blood
We investigated the c-kit cell rolling and firm adhesion in response to TNF-α and SDF-1 in combination by using peripheral blood c-kit+ cells in vivo. There is a similar induction of c-kit cell firm adhesion by TNF-α and SDF-1 (Figure 7b). Moreover, we found peripheral blood c-kit cell adhesion under the baseline condition was significantly higher than bone marrow c-kit (36±10 cells/mm2 in peripheral blood c-kit+ cells vs 3±1 cells/mm2 in bone marrow c-kit+ cells, P=0.005, Figure 7b), which may due to the higher ICAM cell surface expression (Figure 7a, lower panel). This finding is in agreement with our findings which demonstrated that ICAM-1 was involved in the c-kit cell adhesion (Figure 8b).
(a) Confocal laser microscopy images of CXCR-4 protein expression on venular endothelium of murine cremaster muscle venules after local stimulation with SDF-1α and TNF-α. CXCR4 expression (green fluorescence) is induced after local superfusion with a combination of TNF-α and SDF-1α. Triple staining additionally shows nuclei (blue) and endothelium marker (red). (b) Quantitative analysis of ICAM-1- and CXCR4-dependent c-kit+ cell to endothelial cell interactions based on intravital fluorescence microscopy recordings. Number of adherent c-kit+ cells (expressed as cells per mm2 venular endothelium). Experiments were performed in WT animals after systemic blockage with anti-ICAM-1 mAb (gray bars), anti-CXCR4 mAb (diagonal stripe bars) following local superfusion with SDF-1α and TNF-α and compared to WT mice (open bars). Controls were animals without chemokine, anti-ICAM mAb and anti-CXCR4 mAb treatment. Data are expressed as mean±s.e.m. (*P<0.05 vs ‘WT’, #P<0.05 vs ‘control’).
Stimulation with SDF-1α and TNF-α Induces the Expression of CXCR-4 on Venular Endothelium
To analyze the effect of treatment with SDF-1α and TNF-α on endothelial expression of CXCR-4 on the endothelial lining of cremaster muscle venules, confocal laser microscopy was performed.
In SDF-1α+TNF-α-treated cremaster muscles, we detected a clear induction of CXCR4 protein on endothelial cells when compared to untreated control tissue (Figure 8a). While the c-kit+ cell to endothelial interactions were selectively observed in venules, the CXCR4 expression could be detected in both venules and arterioles.
ICAM-1 and CXCR4 Expression Mediate the Firm Adhesion of c-kit+ Cells to Venular Endothelium In Vivo
To clarify the role of ICAM-1 and CXCR4 in response to SDF-1 and TNF-α, WT mice were pretreated systemically with an anti-ICAM-1 and anti-CXCR4 mAb. Treatment with anti-ICAM-1 mAb already reduced the number of adherent c-kit+ cells in control animals (c-kit+ cell adhesion: 3±1 cells/mm2 in ‘control’ vs 0.5±0.5 cells/mm2 in ‘control+anti-ICAM-1’ P=0.04) without any further change after the systemic blockage of CXCR4. However, following combined treatment with SDF-1α/TNF-α and additional application of both anti-ICAM-1 mAb or anti-CXCR4 mAb, firm c-kit+ cell adhesion was found to be almost completely abolished, when compared to SDF-1α/TNF-α treatment alone (P=0.02 and P=0.05), implying an essential function of both ICAM-1 and CXCR4 receptor in c-kit+ cell firm adhesion (all Figure 8b).
Firm Adhesion of c-kit+ Cells from WT Bone Marrow is Inhibited in eNOS (−/−) Mice
To further validate the effects of eNOS on c-kit+ cells' endothelial adhesion behavior, we studied stem cell endothelial interactions (cells from bone marrow of eNOS-expressing WT mice) in eNOS (−/−) mice in vivo.
Rolling
The fraction of rolling c-kit+ cells in control preparations did not differ between eNOS (−/−) and WT mice. In contrast to WT mice, the combined local treatment with SDF-1α and TNF-α in eNOS (−/−) mice did not induce rolling (Figure 9a).
Quantitative analysis of eNOS-dependent interactions between c-kit+ cells and endothelial cells based on intravital fluorescence microscopic recordings. (a) The number of rolling c-kit+ cells (expressed as percentage of all passing cells) in murine cremaster muscle venules exposed to SDF-1 (‘SDF-1’), TNF-alpha (‘TNF-alpha’), and a combination of both (‘SDF-1α+TNF-α’). Controls are mice without chemokine pretreatment (‘control’). (b) Number of firmly adherent c-kit+ cells per mm2 venular endothelial lining. Experiments were performed in WT animals (open bar) and eNOS (−/−) animals (black bar). Significant differences were detected by systemic ‘L-NAME’ pretreatment for antagonism of endogenous NO production in WT mice. Data are expressed as mean±s.e.m. (#P<0.05 vs ‘WT-TNF+SDF’, *P<0.05 vs WT).
Firm adhesion
The number of firmly adherent c-kit+ cells was clearly reduced in eNOS (−/−) control mice (c-kit+ cell adhesion: 0.4±0.4 cells/mm2 in ‘eNOS (−/−)-control vs 7.5±4.6 cells/mm2 in ‘WT-control’, NS) and also tend to be reduced in mice treated with SDF-1 only. In contrast to the findings in WT animals, there was no increase in stem cell adhesion after combined local treatment with SDF-1α and TNF-α in eNOS (−/−) mice (P=0.005 vs ‘WT- SDF-1α +TNF-α’) (all Figure 9b). The results demonstrate that eNOS is mandatory for SDF-1α-mediated c-kit+ cell recruitment.
In Vivo Adhesion of c-kit+ Cells to Venular Endothelium is Blocked after Systemic Treatment with L-NAME
To determine the effects of NOS inhibitors on c-kit+ cells and EL, we applied L-NAME before administration of SDF-1α to the cremaster muscle. L-NAME, an arginine analog, is widely used as a nonselective inhibitor of NOS enzymes. Our main finding on c-kit+ cell-endothelial interaction in eNOS (−/−) experiments after combined treatment with SDF-1α and TNF-α could be reproduced by systemic antagonism of endogenous NO-synthases. While c-kit+ cell rolling was not influenced by NOS antagonism, the L-NAME-treated WT mice showed a clear reduction of adhesion with similar values when compared to eNOS (−/−) animals (c-kit+ cell adhesion: 1.5±0.7 cells/mm2 in ‘L-NAME/SDF-1α+TNF-α’ vs 1±0.5 cells/mm2 in ‘eNOS (−/−)/SDF-1α+TNF-α’, NS, Figure 9b). EL displayed clearly different adhesion behavior in response to NOS antagonism when compared to c-kit+ cells. There was an increased number of adherent EL at baseline (NS) and after superfusion of SDF-1 (P=0.04) after pretreatment with L-NAME. The adhesion of EL in response to TNF-α alone slightly decreased after L-NAME. The combination of TNF-α and SDF-1α in L-NAME-pretreated mice induced EL adhesion when compared to the respective controls nearly two-fold (P=0.02) (Figure 5). Thus, in contrast to c-kit+ cell behavior, EL adherence is induced in response to endothelial SDF-1α stimulation and simultaneous systemic NOS antagonism.
Discussion
Our results demonstrate that SDF-1α alone facilitates the migration capacity of c-kit+ cells in vitro. In vivo, SDF-1α induces a transient c-kit+ cell–endothelial interaction (‘rolling’) and there seems to be no synergistic effect of SDF-1α and TNF-α. However, in terms of firm stem cell adhesion to endothelial cells, which is necessary for subsequent cellular migration across the endothelial layer, we observed that the presence of both SDF-1α chemoattractant activity and inflammatory endothelial activation by TNF-α is required for c-kit+ cells to form functionally relevant interactions with the endothelium in postcapillary venules. The presence of ICAM-1 and CXCR4 on the vascular endothelium appears to be crucial, since systemic blockade of these proteins abolished firm adhesion of c-kit+ cells despite application of SDF-1α and TNF-α. Moreover, firm stem cell adhesion is significantly reduced when eNOS is not present or systemic NOS is inhibited. A rapid induction of endothelial CXCR4 expression after combined local treatment with SDF-1α and TNF-α was observed and may explain the endothelium-linked mechanisms for stem cell recruitment in the peripheral organ.
The primary intention of this study was to investigate the initial interaction process of c-kit+ cells with the vessel wall and to further characterize the required environment and in particular potentially involved enzyme systems or adhesion molecules in a complex in vivo model. This model allowed us to reveal essential preconditions, namely an inflammatory stimulus and the presence of both eNOS, ICAM-1 and CXCR4, on the vascular endothelium, for initial SDF-1α-mediated stem cell recruitment to take place in a living organism. It was clearly not our aim to describe or explore possible downstream signaling pathways in detail or to establish a linkage between the respective findings. However, the interplay of cells, enzyme systems and adhesion molecules at the vascular wall in this context and its implications for the eventual regeneration of injured organs should be further studied.
Within the bone marrow, the interplay of endothelial selectins and cellular adhesion molecules, as well as the respective downstream signaling cascades have been well investigated20, 21, 22 and were analyzed by direct intravital microscopy observation of the murine bone marrow.23, 24, 25 In this context, the role of different integrin subfamilies is currently under intensive investigation.26, 27 With respect to non-marrow organs, extensive studies have been performed on mature leukocyte behavior,28, 29 but there are few reports on peripheral stem cell–endothelium interactions in vivo.11, 30
Intravital fluorescence microscopy allows direct visualization and quantitative analysis of stem cell–endothelium interactions while EL can serve as positive controls for validation and prove of principle of stem cell behavior. The cremaster muscle model is particularly useful since various chemical components can be selectively applied to the target tissue by simple superfusion technique. The finding that firm endothelial c-kit+ cell adhesion requires the interplay of SDF-1α and TNF-α in the postcapillary venular bed can be easily overlooked when attention is paid only to early events in the cellular interaction cascade (‘rolling’). Our current findings help to explain the apparent discrepancy between the results of in vitro stem cell migration assays, implying that SDF-1α alone is a potent chemokine and those of in vivo experiments highlighting the need for additional factors. It appears that in addition to the presence SDF-1α, a certain degree of local inflammation including the expression of ICAM-1 is necessary for firm stem cell adhesion to the endothelium. TNF-α is known to increase the adhesion molecule expression in endothelial cells12, 13 and there is also evidence that TNF-α modulates CXCR4 gene expression in specific cell types.31
Our results suggest that the activation of endothelium by an increase in CXCR-4 expression after SDF-1α and TNF-α stimulation lead to relevant stem cell attraction. While Peled et al. formerly described that pre-activation of human CD34+cells by SDF-1α/CXCR4 leads to LFA-1/ICAM-1-mediated firm adhesion and transendothelial/stromal migration, in our model for peripheral stem cell adhesion, the endothelial cells in the target organ are accordingly activated by SDF-1 induced CXCR4 with ICAM-1-related stem cell adhesion. Therefore both, the endothelial and the stem cell activation are capable to initiate the special interaction pattern for stem cell recruitment.
Our finding that c-kit+ cells firmly adhered exclusively in response to SDF-1α and TNF-α-induced endothelial activation helps to explain the notion by Abbot et al,11 who showed the need of additional factors besides SDF-1α for effective trafficking of c-kit+ cells to the injured heart. Interestingly, we found that endogenous mature leukocytes behaved entirely different, indicating that the SDF-1α/TNF-α interplay has specific effects on c-kit+ cells and is not mediating endothelial adhesion for any cell type in general. Endothelial activation by TNF-α alone resulted in a significant increase in firmly adherent leukocytes to maximum values, whereas SDF-1α superfusion in addition to TNF-α had no further effect on mature leukocyte-to-endothelial interactions. These findings confirm the common understanding of leukocyte behavior in inflammatory environments as shown in the cremaster muscle29 and other models and underline the selective role of SDF-1 for stem cell behavior.
The obvious absence of stem cell adhesion in eNOS KO mice supports the current knowledge of the crucial relevance of endothelial NO production for stem cell mobilization and neo-vascularization in the presence of SDF-1α.32 The amount of endothelial injury in the target organ and time course of local NO production after eNOS activation by Akt may play an important role for therapeutic stem cell treatment.33 In human endothelial cells, the induction of eNOS by TNF-α has recently been described by De Palma et al.34 In contrast, a downregulation of eNOS was observed in association with high levels of TNF-α in patients with type 2 diabetes and microangiopathy.35 Systemic L-NAME treatment and thereby antagonism of NOS also in the injected stem cells led to a clear inhibition of c-kit+ cell adhesion with nearly identical amounts as detected in eNOS (−/−) mice. This result may underline the critical role of eNOS activity in mononuclear cells as reported by Sasaki et al.16 Further, the endothelium-derived NO is shown to be important for stem cell engraftment in the same manner.
Hence, NOS-mediated endothelial signaling cascades may be important to initiate stem cell-based repair processes in non-marrow tissue. At the same time, NOS actions might play a protective role against inflammatory injury by mature leukocytes which have been recently been described in the cremaster muscle36 and in ischemia and reperfusion injury to the heart.37 NOS might be a determinant for tissue to decide about the amount of inflammation and regeneration.
In conclusion, we have shown that the bone marrow-derived stem cell population acts autonomously with respect to endothelial adhesion in non-marrow tissue. Stem cell therapy strategies aiming at non-marrow tissue require inflammatory stress and intact endothelial NO production by eNOS in the target organ so as to fully exploit the stem cell-attracting potential of SDF-1α.
References
Vandervelde S, van Luyn MJ, Tio RA, et al. Signaling factors in stem cell-mediated repair of infarcted myocardium. J Mol Cell Cardiol 2005;39:363–376.
Ceradini DJ, Kulkarni AR, Callaghan MJ, et al. Progenitor cell trafficking is regulated by hypoxic gradients through HIF-1 induction of SDF-1. Nat Med 2004;10:858–864.
Ji JF, He BP, Dheen ST, et al. Interactions of chemokines and chemokine receptors mediate the migration of mesenchymal stem cells to the impaired site in the brain after hypoglossal nerve injury. Stem Cells 2004;22:415–427.
Kollet O, Shivtiel S, Chen YQ, et al. HGF, SDF-1, and MMP-9 are involved in stress-induced human CD34+ stem cell recruitment to the liver. J Clin Invest 2003;112:160–169.
Lapidot T, Petit I . Current understanding of stem cell mobilization: the roles of chemokines, proteolytic enzymes, adhesion molecules, cytokines, and stromal cells. Exp Hematol 2002;30:973–981.
Peled A, Petit I, Kollet O, et al. Dependence of human stem cell engraftment and repopulation of NOD/SCID mice on CXCR4. Science 1999;283:845–848.
De Falco E, Porcelli D, Torella AR, et al. SDF-1 involvement in endothelial phenotype and ischemia-induced recruitment of bone marrow progenitor cells. Blood 2004;104:3472–3482.
Askari AT, Unzek S, Popovic ZB, et al. Effect of stromal-cell-derived factor 1 on stem-cell homing and tissue regeneration in ischaemic cardiomyopathy. Lancet 2003;362:697–703.
Kucia M, Dawn B, Hunt G, et al. Cells expressing early cardiac markers reside in the bone marrow and are mobilized into the peripheral blood after myocardial infarction. Circ Res 2004;95:1191–1199.
Abbott JD, Huang Y, Liu D, et al. Stromal cell-derived factor-1alpha plays a critical role in stem cell recruitment to the heart after myocardial infarction but is not sufficient to induce homing in the absence of injury. Circulation 2004;110:3300–3305.
Ruster B, Gottig S, Ludwig RJ, et al. Mesenchymal stem cells display coordinated rolling and adhesion behavior on endothelial cells. Blood 2006;108:3938–3944.
Chandrasekharan UM, Siemionow M, Unsal M, et al. TNF-{alpha} receptor-II is required for TNF-{alpha}-induced leukocyte–endothelial interaction in vivo. Blood 2007;109:1938–1944.
Sumaqin R, Sarelius IH . TNF-{alpha} activation of arterioles and venules alters distribution and levels of ICAM-1 and affects leukocyte–endothelial cell interactions. Am J Physiol Heart Circ Physiol 2006;291:2116–2125.
Guthrie SM, Curtis LM, Mames RN, et al. The nitric oxide pathway modulates hemangioblast activity of adult hematopoietic stem cells. Blood 2005;105:1916–1922.
Landmesser U, Engberding N, Bahlmann FH, et al. Statin-induced improvement of endothelial progenitor cell mobilization, myocardial neovascularization, left ventricular function, and survival after experimental myocardial infarction requires endothelial nitric oxide synthase. Circulation 2004;110:1933–1939.
Sasaki K, Heeschen C, Aicher A, et al. Ex vivo pretreatment of bone marrow mononuclear cells with endothelial NO synthase enhancer AVE9488 enhances their functional activity for cell therapy. Proc Natl Acad Sci USA 2006;103:14537–14541.
Baez S . An open cremaster muscle preparation for the study of blood vessels by in vivo microscopy. Microvasc Res. 1973;5:384–394.
Vollmar B, Schmits R, Kunz D, et al. Lack of in vivo function of CD31 in vascular thrombosis. Thromb Haemost 2001;85:160–164.
Baker M, Wayland H . On-line volume flow rate and velocity profile measurement for blood in microvessels. Microvasc Res 1974;7:131–143.
Peled A, Grabovsky V, Habler L, et al. The chemokine SDF-1 stimulates integrin-mediated arrest of CD34(+) cells on vascular endothelium under shear flow. J Clin Invest 1999;104:1199–1211.
Wang JF, Park IW, Groopman JE . Stromal cell-derived factor-1alpha stimulates tyrosine phosphorylation of multiple focal adhesion proteins and induces migration of hematopoietic progenitor cells: roles of phosphoinositide-3 kinase and protein kinase C. Blood 2000;95:2505–2513.
Zhang XF, Wang JF, Matczak E, et al. Janus kinase 2 is involved in stromal cell-derived factor-1alpha-induced tyrosine phosphorylation of focal adhesion proteins and migration of hematopoietic progenitor cells. Blood. 2001;97:3342–3348.
Frenette PS, Subbarao S, Mazo IB, et al. Endothelial selectins and vascular cell adhesion molecule-1 promote hematopoietic progenitor homing to bone marrow. Proc Natl Acad Sci USA 1998;95:14423–14428.
Hidalgo A, Weiss LA, Frenette PS . Functional selectin ligands mediating human CD34(+) cell interactions with bone marrow endothelium are enhanced postnatally. J Clin Invest 2002;110:559–569.
Mazo IB, Gutierrez-Ramos JC, Frenette PS, et al. Hematopoietic progenitor cell rolling in bone marrow microvessels: parallel contributions by endothelial selectins and vascular cell adhesion molecule 1. J Exp Med 1998;188:465–474.
Chavakis E, Aicher A, Heeschen C, et al. Role of beta2-integrins for homing and neovascularization capacity of endothelial progenitor cells. J Exp Med 2005;201:63–72.
Katayama Y, Hidalgo A, Peired A, et al. Integrin alpha4beta7 and its counterreceptor MAdCAM-1 contribute to hematopoietic progenitor recruitment into bone marrow following transplantation. Blood 2004;104:2020–2026.
Kantele JM, Kurk S, Jutila MA . Effects of continuous exposure to stromal cell-derived factor-1 alpha on T cell rolling and tight adhesion to monolayers of activated endothelial cells. J Immunol 2000;164:5035–5040.
Thorlacius H, Vollmar B, Guo Y, et al. Lymphocyte function antigen 1 (LFA-1) mediates early tumour necrosis factor alpha-induced leucocyte adhesion in venules. Br J Haematol 2000;110:424–429.
Torrente Y, Tremblay JP, Pisati F, et al. Intraarterial injection of muscle-derived CD34(+)Sca-1(+) stem cells restores dystrophin in mdx mice. J Cell Biol 2001;152:335–348.
Kury P, Koller H, Hamacher M, et al. Cyclic AMP and tumor necrosis factor-alpha regulate CXCR4 gene expression in Schwann cells. Mol Cell Neurosci 2003;24:1–9.
Hiasa K, Ishibashi M, Ohtani K, et al. Gene transfer of stromal cell-derived factor-1alpha enhances ischemic vasculogenesis and angiogenesis via vascular endothelial growth factor/endothelial nitric oxide synthase-related pathway: next-generation chemokine therapy for therapeutic neovascularization. Circulation 2004;109:2454–2461.
Mukai Y, Rikitake Y, Shiojima I, et al. Decreased vascular lesion formation in mice with inducible endothelial-specific expression of protein kinase Akt. J Clin Invest 2006;116:334–343.
De Palma C, Meacci E, Perrotta C, et al. Endothelial nitric oxide synthase activation by tumor necrosis factor alpha through neutral sphingomyelinase 2, sphingosine kinase 1, and sphingosine 1 phosphate receptors: a novel pathway relevant to the pathophysiology of endothelium. Arterioscler Thromb Vasc Biol 2006;26:99–105.
Makino N, Maeda T, Sugano M, et al. High serum TNF-alpha level in type 2 diabetic patients with microangiopathy is associated with eNOS down-regulation and apoptosis in endothelial cells. J Diabetes Complications 2005;19:347–355.
Sanz MJ, Hickey MJ, Johnston B, et al. Neuronal nitric oxide synthase (NOS) regulates leukocyte–endothelial cell interactions in endothelial NOS deficient mice. Br J Pharmacol 2001;134:305–312.
Bulhak AA, Sjoquist PO, Xu CB, et al. Protection against myocardial ischaemia/reperfusion injury by PPAR-alpha activation is related to production of nitric oxide and endothelin-1. Basic Res Cardiol 2006;101:244–252.
Acknowledgements
We gratefully acknowledge the technical help of M Nickel and M Fritsche. This work was supported by Helmholtz Gemeinschaft, Mecklenburg-Vorpommern (Nachwuchsgruppe Regenerative Medizin Regulation der Stammzellmigration 0402710), BMBF BioChance PLUS (0313191), Miltenyi Biotec, Sonderforschungsbereich/Transregio 7 B5, B2 and A4; START-MSC project (project 6: Kardiovaskuläre Differenzierung und Applikation definierter mesenchymaler Stammzellpopulationen), and Steinbeis Transfer Zentrum für Herz-Kreislaufforschung, Rostock, Germany.
Author information
Authors and Affiliations
Corresponding author
Additional information
CONFLICT OF INTEREST/DISCLOSURE STATEMENT
None.
Rights and permissions
About this article
Cite this article
Kaminski, A., Ma, N., Donndorf, P. et al. Endothelial NOS is required for SDF-1α/CXCR4-mediated peripheral endothelial adhesion of c-kit+ bone marrow stem cells. Lab Invest 88, 58–69 (2008). https://doi.org/10.1038/labinvest.3700693
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/labinvest.3700693
Keywords
This article is cited by
-
Early onset of aging phenotype in vascular repair by Mas receptor deficiency
GeroScience (2022)
-
c-kit+ cells: the tell-tale heart of cardiac regeneration?
Cellular and Molecular Life Sciences (2015)
-
Zellquellen für kardiovaskuläres Tissue Engineering
Der Chirurg (2011)
-
Kardiale Protektion und Regeneration
Zeitschrift für Herz-,Thorax- und Gefäßchirurgie (2010)
-
Chirurgische intramyokardiale Stammzelltherapie bei chronischer Myokardischämie
Herz (2010)