Abstract
To investigate whether the multifocal inflammatory disease in TGFβ1-deficient mice is caused by self-antigen (self-Ag)-specific autoreactive T cells, or whether it is caused by antigen independent, spontaneous hyperactivation of T cells, we have generated Tgfb1−/− and Tgfb1−/− Rag1−/− mice expressing the chicken OVA-specific TCR transgene (DO11.10). On a Rag1-sufficient background, Tgfb1−/− DO11.10 mice develop a milder inflammation than do Tgfb1−/− mice, and their T cells display a less activated phenotype. The lower level of activation correlates with the expression of hybrid TCR (transgenic TCRβ and endogenous TCRα), which could recognize self-Ag and undergo activation. In the complete absence of self-Ag recognition (Tgfb1−/− DO11.10 Rag1−/− mice) inflammation and T-cell activation are eliminated, demonstrating that self-Ag recognition is required for the hyper-responsiveness of TGFβ1-deficient T cells. Thus, TGFβ1 is required for the prevention of autoimmune disease through its ability to control the activation of autoreactive T cells to self-Ag.
Similar content being viewed by others
Main
A deficiency in transforming growth factor beta 1 (TGFβ1) causes a lethal inflammatory disease in mice1, 2 that is eliminated in the absence of T cells but not B cells.3 The T-cell-dependent inflammatory disease is not pathogen mediated because in TGFβ1-deficient mice there is no evidence of bacteria in inflamed tissues, no antibodies to bacteria are found in serum, and no significant bacterial pathogens are detected when samples of inflamed tissues are cultured in pediatric broth.1 In addition, germ-free Tgfb1−/− mice (no enteric bacteria in the gut) develop the same inflammatory disease.4 Consequently, TGFβ1 plays an intrinsic role in preventing T-cell activation and activation-induced cell death.5, 6, 7
We have previously shown that Tgfb1−/− T cells are activated in vivo due to a lowered threshold of activation resulting from increased [Ca2+]i levels.8 Unlike TGFβ1 function in Treg cells which is SMAD3 dependent,9, 10 Ca2+/Calcineurin-mediated TGFβ1 function in T cells is SMAD3 independent since Smad3−/− mice do not have this autoimmune disease.5, 11, 12, 13 Consequently, TGFβ1 plays immune regulatory roles in different T cells through different signaling mechanisms, thereby enhancing the potential for fine-tuning the tolerance and response arms of the adaptive immune system. What is as yet unclear is whether the activation of TGFβ1-deficient T cells requires self-antigen (self-Ag) recognition, or whether it occurs spontaneously in the absence of any antigenic stimulation.
To test this we have combined Tgfb1−/− and Tgfb1−/− Rag1−/− mice with TCR transgenic mice expressing the OVA-specific TCR DO11.10. CD4+ T cells in DO11.10 mice are known to become activated only when the cognate peptide (a peptide derived from OVA) is presented by MHC II on an I-Ad background. Here, we show that complete elimination of self-reactive TCR-bearing T cells is sufficient to rescue Tgfb1−/− mice from their lethal autoimmune phenotype and to eliminate the hyper-responsiveness of TGFβ1-deficient T cells. Consequently, TGFβ1 is essential for preventing inappropriate activation of self-reactive T cells.
Materials and methods
Mice
Tgfb1+/− mice (BALB/c, N7) were kindly provided by James D Gorham (Dartmouth Medical School). DO11.10 mice were kindly provided by J Gabriel Michael (University of Cincinnati Medical School) and were genetically combined with Rag1−/− mice in our specific pathogen-free animal facility at the University of Cincinnati Medical Center. DO11.10 Rag1−/− mice were in turn combined with Tgfb1+/− mice to generate Tgfb1−/− DO11.10 and Tgfb1−/− DO11.10 Rag1−/− mice. All mice were used at the ages described in the text and figure legends. All the mice were housed and handled as per approved IACUC protocols at the University of Cincinnati.
Reagents
All media and reagents for cell culture studies were purchased from either Life Technologies (GIBCOBRL) (Rockville, MD, USA) or Sigma (St Louis, MO, USA). Paraformaldehyde was purchased from Electron Microscopy Sciences (Washington, PA, USA). Thymidine, [Methyl-3H]-(specific activity 6.7 Ci/mmol) was purchased from NEN™ Life Science Products Inc. (Boston, MA, USA). Tissue culture plates were purchased from Becton Dickinson (Franklin Lakes, NJ, USA). PMA (10 μM) and Ionomycin (100 μM) stocks were prepared in DMSO, aliquoted and stored at −80°C.
Antibodies
Purified anti-mouse CDɛ, anti-mouse CD28, anti-mouse CD16/CD32 (FcγIII/II receptor), anti-mouse interleukin-2 (IL-2) and anti-mouse interferon gamma (IFNγ) antibodies, FITC-anti-mouse CD3ɛ, FITC-CD69, FITC- or APC-CD44, FITC- or PerCP-anti-mouse CD4 (L3T4), APC-CD62L, R-PE-conjugated anti-mouse antibodies to CD25, CD44, CD49d, CD62L and CD69, and fluorochrome-conjugated isotype control antibodies were purchased from either BD Pharmingen (San Diego, CA, USA) or eBioscience (San Diego, CA, USA). R-PE-anti-mouse CD11a (LFA-1) was purchased from BioDesign (Saco, ME, USA). FITC-, PE- or APC-KJ1-26 (clonotypic anti-TCR Ab against DO11.10 TCR) was purchased from CALTAG (Burlingame, CA, USA). FOXP3 staining kit (clone FJK-16s) was purchased from eBioscience (San Diego, CA, USA).
PCR Genotyping
The genotype of newborn pups from heterozygous matings was determined by PCR amplification of tail DNA and size fractionation on agarose gels.14 Genotyping of DO11.10 mice and TCR expression were also determined by PCR amplification of tail DNA and flow cytometry of splenic T cells.
Splenocyte proliferation and phenotype analysis
Single-cell suspensions were prepared, enumerated and assayed for their mitogenic response using a [3H]thymidine incorporation assay after 2 days of in vitro culture as described.7 Culture supernatants were collected and frozen until cytokines were analyzed by sandwich ELISA as described earlier.7
Phenotype analysis of splenocytes was determined by four-color flow cytometry using BD-LSR flow cytometer with the appropriate fluorochrome-conjugated antibodies (BD Pharmingen, San Diego, CA, USA) as described.7 Cells were stained for surface markers, as described previously.7 For detecting intracellular FOXP3 expression, the surface-stained cells were fixed and permeabilized using the Fix/Perm buffer overnight at 4°C and stained for FOXP3. Cytokines were assayed in culture supernatants, as described previously.7
Inflammation score
Animals were euthanized following institutional guidelines and tissues were fixed in 10% neutral-buffered formalin. Tissues were dehydrated through a gradient of alcohol and xylene, embedded in paraffin, and 5 μm sections were cut and H&E stained. An inflammation score was assigned to each tissue depending on the severity of the inflammatory cell infiltrate: 0 (no inflammation), 0.5 (very mild), 1.0 (mild), 2 (moderate), 3 (severe) and 4 (very severe).3, 7 Very mild: the inflammatory cells are very infrequent and usually involve less than 10 cells. Mild: inflammatory component is composed of less than 100 cells. The inflammation is confined to a few areas in the tissues. Moderate: inflammation involves multiple areas in the tissue or is a large area composed of more than 100 inflammatory cells but less than 1000 cells. There may be associated tissue damage near the inflammatory component. Severe: inflammatory cells comprise large multifocal areas of the tissue and usually involves at least 20% of the tissue. There are greater than 1000 cells involved. There is clear alteration of the adjacent tissues either due to compression from the inflammatory component or necrosis of the adjacent tissue. Very severe: similar to severe only nearly all areas of the tissue are affected. There is alteration of the normal parenchyma appearance. Data for the most commonly affected organs are shown in the figures.
Statistical analysis
Survival rates were calculated using Kaplan–Meier method, frequencies of affected tissues were calculated using χ2-test, and the mean body weights were compared using Student's t-test.
Results
TCR Transgenic Expression Prolongs Survival and Reduces Systemic Autoimmune Inflammation in Tgfb1–/– Mice
We have recently shown that splenic Tgfb1−/− T cells, but not B cells, exhibit features of prior in vivo activation as evidenced by downmodulation of CD3 and CD8 surface expression and increased CD11a (LFA-1) expression, IFNγ production, cytosolic [Ca2+]i levels and cell size.7 Additionally, the majority of Tgfb1−/− CD4+ peripheral T cells show downregulation of CD62L and upregulation of CD44, suggesting a marked increase in fully differentiated effector/effector memory cells in Tgfb1−/− mice (data not shown; Figure 2). To test this possibility, we genetically combined the Tgfb1 knockout (KO) allele with the DO11.10 transgene, which produces largely MHC II-restricted CD4+ T cells recognizing OVA peptide presented by I-Ad molecules (BALB/c background). Tgfb1−/− DO11.10 mice are healthy and live longer than Tgfb1−/− mice (mean age of death 6 vs 3 weeks for Tgfb1−/− mice) (P<0.0001, Kaplan–Meier log rank test; Figure 1a), but, as is also the case for Tgfb1−/− mice, they are smaller than their wild-type (WT) littermates and exhibit a wasting syndrome (P<0.01 at most age groups, Student's t-test; Figure 1b). This observation is consistent with our previous studies which suggested that the wasting syndrome is neither due to inflammation nor lymphocytes although inflammatory stress accelerates wasting in Tgfb1−/− mice.1, 14, 15 As failure to thrive and development of a wasting syndrome may occur due to abnormalities in the gastrointestinal tract, we investigated gastrointestinal tract lesions and found a moderate to severe loss of parietal cells in the stomach in 36% of mice, colon/cecal inflammation in 18%, and hyperplasia in colon/cecum in 9% (n=22 Tgfb1−/− DO11.10 mice). The loss of parietal cells in these mice could result from a humoral autoimmune response causing production of autoantibodies to parietal cells and development of autoimmune gastritis16 since Tgfb1−/− B cells are also hyper-responsive in these mice (Bommireddy et al3 data not shown). These findings are consistent with our earlier observations suggesting that the wasting syndrome in Tgfb1−/− mice is T-cell independent.15, 17 Further, neutrophils and macrophages are the major contributors to the mild inflammation observed in Tgfb1−/− Rag-deficient mice.14, 17
Inflammation is eliminated in Tgfb1−/− DO11.10 Rag1−/− mice. H&E-stained sections of heart from 2-week-old Tgfb1−/− mouse (left) and heart (middle) and liver (right) from an 8-week-old Tgfb1−/− DO11.10 Rag1−/− mouse are shown (a). Note that there were no lesions, and compare with the Tgfb1−/− NTg mouse liver shown in Figure 1e left panel. (b) Thymocyte development as shown by CD4 and CD8 expression is similar between a Tgfb1−/− DO11.10 Rag1−/− mouse and a Tgfb1+/− DO11.10 Rag1−/− mouse. (c and d) CD4+ KJ1-26+ T cells are not activated in Tgfb1−/− DO11.10 Rag1−/− mice in vivo. Splenocytes from one 8-week- (c) or one 4-months- (d) old Tgfb1−/− DO11.10 Rag1−/− and littermate control mice were prepared and stained for expression of TCR, CD4 and CD11a, CD44, CD62L, CD69 or CD25 (c) or KJ1-26, CD4, CD44 and CD62L (d). (e) Tgfb1−/− CD4+ T cells are activated in vivo. Splenocytes from three 2- to 3-week-old Tgfb1−/− and littermate control mice (d20 shown here) were prepared and stained for surface expression of CD4, CD44 and CD62L. CD44 and CD62L expression was analyzed on CD4+-gated splenocytes as described in Materials and methods.
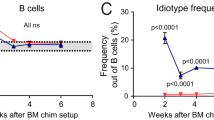
Survival, growth pattern and inflammation in Tgfb1−/− DO11.10 mice. Tgfb1−/− (n=35) and Tgfb1−/− DO11.10 Rag1+/+or+/– littermates (n=22) were monitored and weighed weekly until they were moribund or euthanized for tissue collection. H&E-stained tissue sections were assessed for the presence of inflammation. Data are represented as percent survival (a), body weight (b), percentage of mice with the number of inflamed tissues (c) and inflammation score for individual tissues (d). (a) Tgfb1−/− DO11.10 mice live longer than Tgfb1−/− mice (P<0.0001, Kaplan–Meier log rank test). (b) Tgfb1−/− DO11.10 mice have reduced body weights (P<0.0002 at 8 weeks age; n=8 and 11 for Tgfb1+/+or− DO11.10 Rag1+/+or− and Tgfb1−/− DO11.10 Rag1+/+or−, respectively; Student's t-test). A square and an arrow indicate the age by which all Tgfb1−/− mice are dead. (c) Numbers of tissues with inflammatory lesions are lesser in Tgfb1−/− DO11.10 Rag1+/+or− mice (2 to 15-week-old; black bars) than in Tgfb1−/− (10–20-d old; gray bars) mice (P<0.0001, χ2-test). (d) Inflammation scores for the most commonly affected organs in Tgfb1−/− DO11.10 mice with age range from 2 to 15 weeks. Each symbol represents one mouse and both black and white symbols represent the same group of mice but different tissues (see text). (e) Representative H&E-stained liver sections showing inflammation in d20 Tgfb1−/− (left) and Tgfb1−/− DO11.10 mice (right).
Evaluation of inflammatory lesions shows that among the 22 Tgfb1−/− DO11.10 mice that we have analyzed thus far, most Tgfb1−/− DO11.10 mice either have no inflammation in all tissues examined (14%) or have inflammation in only 1–4 tissues (77%), which is in contrast to the immunocompetent Tgfb1−/− BALB/c (Tgfb1−/− TCR nontransgenic) cohort where 96% of 25 mice have inflammation in ≥4 organs and no mice are devoid of inflammation (Figure 1c).3, 7 The inflammation index, defined as the sum of the severity (0–4) of inflammation from 25–30 tissues divided by the number of tissues evaluated (Figure 1d), was dramatically reduced in Tgfb1−/− DO11.10 mice relative to Tgfb1−/− animals (0.11 vs 0.49, ie, 4.5-fold reduction).7 Further histological analysis of individual tissues reveals that 59% of mice have either mild or no inflammation in the tissues examined, 32% of the mice have moderate to severe inflammation in lungs and pancreas, and only 9% have moderate inflammation in all other tissues examined (Figure 1d). This is in contrast to Tgfb1−/− mice which show moderate to severe inflammation in all tissues examined by 3 weeks of age.1 Representative tissue sections show that whereas no significant inflammation is seen in the liver of Tgfb1−/− DO11.10 Rag1+/− mice (Figure 1e, right panel), a severe necroinflammatory liver disease, a characteristic feature of Tgfb1−/− mice on a BALB background,18 occurs in the littermate Tgfb1−/− TCR nontransgenic mouse (Figure 1e, left panel). Thus, reducing self-Ag recognition in TGFβ1-deficient mice through the introduction of a TCR transgene whose cognate peptide is not present in vivo lessens the severity of inflammation.
Elimination of Endogenous Antigen Recognition Prevents Activation of Tgfb1−/− DO11.10 T Cells
To test the hypothesis that activation of Tgfb1−/− DO11.10 T cells and mild inflammation in these mice is due to the presence of TCR nontransgenic T cells and hybrid TCR on DO11.10 T cells, we have generated Tgfb1−/− DO11.10 Rag1−/− mice which should harbor no hybrid TCR. Four mice were analyzed for inflammation and T-cell activation. As expected, these mice did not develop significant inflammation in any organ (Figure 2a). Only minimal inflammation, primarily due to neutrophil and macrophage infiltration, was present in the cecum (1 of 4), colon (1 of 4), liver (1 of 4) and lungs (2 of 4) of these mice. This is also consistent with our previous observation that neutrophils and macrophages do contribute to mild inflammation and inflammatory bowel disease-mediated colon cancer in Tgfb1−/− Rag2−/− mice,14 a disease that is not autoimmune in nature because it is completely eliminated by rendering the mice germ-free.15 Consistent with a low level of inflammation in Tgfb1−/− DO11.10 Rag1−/− mice, these mice are smaller than their Tgfb1+/+ littermate controls (Figure 1b), as also previously reported in Tgfb1−/− Rag2−/− and Tgfb1−/− Rag1−/− mice.14, 17
Flow cytometry of splenocytes and thymocytes revealed that thymocyte development in Tgfb1−/− DO11.10 Rag1−/− mice appears similar to that in control animals (Figure 2b). As expected, splenic T cells are not activated in these mice as revealed by FACS analysis of activation markers CD44, CD62L, CD11a, CD69 and CD25 on splenic T cells from 2-month-old Tgfb1−/− DO11.10 Rag1−/− and littermate control mice (Figure 2c). Similar results were obtained from a 4-month-old mouse as most of the Tgfb1−/− DO11.10 Rag1−/− T cells were CD44lo and CD62Lhi (Figure 2d). In contrast, splenic T cells in TCR nontransgenic Tgfb1−/− mice are markedly activated, with a massive increase in CD4+ effector/effector memory (CD62Llo CD44hi) cells (Figure 2e). These striking data (Figure 2d vs e) suggest that Tgfb1−/− T cells must be presented with self-Ag in order to undergo activation and cause autoimmunity. Thus, there is no constitutive hyperactivation of Tgfb1−/− T cells in the absence of a cognate antigen. Taken together these data demonstrate that limiting the T-cell repertoire to a single TCR that recognizes a nonpresent foreign Ag eliminates T-cell-mediated autoimmune disease in Tgfb1−/− mice.
TCR Transgenic Expression Rescues Tgfb1−/− Mice from a Thymic T-Cell Developmental Anomaly, but Their Peripheral T Cells Still Show Evidence of In Vivo Activation
We have previously shown that thymic T-cell development is normal until 1 week after birth in Tgfb1−/− mice;8 but as these mice start developing inflammatory lesions in peripheral tissues, the thymus becomes smaller and is often invisible by the time they are moribund at about 3 weeks of age. This is due to cortical depletion as evidenced by a severe reduction in CD4+CD8+ thymocytes and a consequent increase in the proportion of CD4+CD8− thymocytes.8, 19 We have previously suggested that the impairment in thymocyte development in Tgfb1−/− mice is affected by the inflammatory environment8 and not due to the absence of TGFβ1 alone. To test this idea further we analyzed the thymocyte profile in 4 to 8-week-old Tgfb1−/− DO11.10 mice and their control littermate DO11.10 mice. Indeed, thymocyte development is nearly normal in these mice regardless of the presence or absence of TGFβ1 (Figure 3a, right and middle panels). This is in contrast to a day 21 Tgfb1−/− mouse which exhibits a severe decrease in double-positive thymocytes and a marked increase in CD4+CD8− cells in the thymus (Figure 3a, left panel). This demonstrates that elimination of self-Ag recognition, which reduces inflammation in Tgfb1−/− DO11.10 mice (Figure 1), restores normal thymocyte maturation and prevents the shift in thymocyte profiles to CD4+CD8− that normally occur in Tgfb1−/− mice.
Phenotype of Tgfb1−/− DO11.10 T cells. Thymocytes from 5-week old (a) or splenocytes from d44-old (b) Tgfb1−/− DO11.10 Rag1+/− and littermate control mice were stained for CD4, CD8, TCR using KJ1-26 antibody, and activation markers CD11a, CD44, CD25 or CD62L. Dot plots with percentage of populations in each quadrant are shown for thymocytes (a) and CD4+-gated splenocytes (b).
Further analyses of splenocytes and thymocytes demonstrate that there are both KJ1-26+ (KJ1-26 is a clonotypic antibody that recognizes DO11.10 TCR) and KJ1-26− T cells (TCR nontransgenic) in Tgfb1+/+ DO11.10 Rag1+/ and Tgfb1−/− DO11.10 Rag1+/ mice. We reasoned that the mild to moderate inflammation seen in the Tgfb1−/− DO11.10 Rag1+/ mice could be caused in part by TCR nontransgenic T cells (KJ1-26− CD4+), which would recognize self-Ag and undergo activation (Figure 3b, left quadrants). To our surprise, we observed that the transgenic T-cell population (KJ1-26+) also exhibits significant activation in Tgfb1−/− DO11.10 mice, as evidenced by an increase in the percentage of activated KJ1-26+ CD4+ T cells (Figure 3b). Further, the mean fluorescence intensity (MFI) of surface markers, such as CD11a, CD44 and CD49d, is increased, and that of CD62L, is reduced on Tgfb1−/− DO11.10 T cells (data not shown; Figure 5c), indicating their activation.
Endogenous TCRvα2 expression is downmodulated on Tgfb1−/− CD3+CD4+ splenocytes. Splenocytes from 8-week-old Tgfb1−/− DO11.10 Rag1+/+or− and control (Tgfb1+/− DO11.10 Rag1+/+or−) mice were stained for CD3, CD4, KJ1-26 and TCRVα2. Note the reduced TCRVα2 MFI in Tgfb1−/− mice (a). Presence of hybrid TCR-bearing DO11.10 T cells (KJ1-26+TCRvα2+) is shown in upper right quadrants (b). (c) T-cell activation markers are upregulated on self-reactive T cells and are modulated by TGFβ1. Splenocytes from 5-week-old Tgfb1−/− DO11.10 and littermate control mice were stained for TCR, CD4 and CD11a, CD44, CD49d, CD62L or CD69. Histograms were generated for activation markers gated on KJ1-26+ (left panels) or KJ1-26– (right panels) CD4+ T cells from Tgfb1−/− (open histograms) and Tgfb1+/+ control mice (closed histograms). The results represent three to six experiments.
We have recently reported that in the periphery Tgfb1−/− T cells, but not B cells, exhibit a split anergic response to mitogenic stimulation as evidenced by decreased IL-2, IL-4 and IL-10 production and diminished [Ca2+]i flux in response to anti-CD3 stimulation.3, 7 This split anergic response to receptor-mediated stimulation is mainly due to prior activation in vivo as evidenced by CD3 and CD8 downmodulation, increased expression of CD11a (LFA-1) and IFNγ, elevated cytosolic [Ca2+]i levels and increased cell size.7 Also, stimulation of these cells with receptor-independent mitogenic stimulation such as PMA plus ionomycin rescues them from such ex vivo hyporesponsiveness.7 However, since inflammation develops very early in the life of these mice, it was difficult to conclude whether the hyporesponsiveness of T cells was due to the absence of TGFβ1, due to the highly inflamed environment, or due to their prior activation in vivo. Hence, we determined T-cell responses in the absence of any significant inflammation in Tgfb1−/− DO11.10 mice.
Mature Splenic T Cells Exhibit Split Anergic Response to Ex Vivo Stimulation
Consistent with the increase in activation markers on Tgfb1−/− DO11.10 T cells (Figure 3b), the Tgfb1−/− DO11.10 splenocytes, upon stimulation with mitogens, produce more IFNγ than the Tgfb1+/+ DO11.10 cells (Figure 4a, upper panels). IL-2 production in these cultures, however, is lower than in control cultures stimulated with anti-CD3 or Con A. Stimulation with PMA plus ionomycin, which causes TCR-independent activation by acting directly on cytosolic signaling targets, increases the production of IL-2 by Tgfb1−/− DO11.10 splenocytes (Figure 4a, lower panels). Such split anergy in T-cell responses to mitogens (decreased IL-2, but increased IFNγ production) in Tgfb1−/− DO11.10 mice is likely due to the prior activation of T cells in vivo as we have shown previously with T cells from Tgfb1−/− mice.7 Consistently, the T cells' proliferative response to mitogenic stimulation is also decreased in Tgfb1−/− DO11.10 mice compared with cells from control mice (Figure 4b). We think that CD4+ T cells become pathogenic upon self-Ag recognition and produce more IFNγ, and may not be called Th1 cells since they produce little IL-2 (discussed further in Bommireddy et al7). The reason for the relatively decreased proliferative response could not be due to a decreased number of T cells as there are equal percentages of CD3+ T cells (21% CD3+ T cells in both groups of mice). Analysis of CD3 expression suggests that there is downmodulation of TCR on KJ1-26+ as well as KJ1-26− CD4+ T cells in Tgfb1−/− mice (Figure 4c). Thus, Tgfb1−/− T cells exhibit evidence of in vivo activation even in animals that have minimal to no inflammation, suggesting that the observed T-cell phenotype does not occur as a consequence of inflammation.
‘Split’ (elevated IFNγ but reduced IL-2 and proliferation) T-cell responses upon ex vivo mitogenic stimulation in Tgfb1−/− DO11.10 splenocytes. Splenocytes from 2 to 6-week-old Tgfb1−/− DO11.10 Rag1+/+or− and littermate control mice were cultured as described for 2–3 days. (a) Culture supernatants collected after 2 days of culture with anti-CD3 (left panels), Con A (middle panels) or PMA+Ionomycin (right panels) were analyzed for IFNγ (upper panels) and IL-2 (lower panels) by sandwich ELISA. Data shown are from 4-week-old mice. Similar results were obtained from 2 and 5-week-old mice. Average cytokine levels in the control cultures without any mitogens were similar for both groups of mice (300 pg/ml [IFNγ] and 80 pg/ml [IL-2]). (b) Cultures were pulsed with tritiated thymidine for 12–14 h and harvested and counted. Data are presented as the mean dpm±s.d. from triplicate cultures from one of three similar experiments (n=total four mice per group). (c) Expression of CD3 and KJ1-26 on splenocytes from these mice described in (a) and (b). Percentage of populations in each quadrant is shown in the dot plots, and MFI of CD3 on KJ1-26+ and KJ1-26− splenocytes is shown in the Table. TCR downmodulation is consistent in all the KO mice tested thus far. Data shown are from a mouse that had moderate inflammation only in the lung and pancreas. Data represent three to six experiments. Ntg, nontransgenic.
These data might suggest that DO11.10-positive T cells undergo activation and become effector/effector memory cells without any antigenic stimulation. One possible explanation could be that activation of transgenic T cells results from bystander activation from the few neighboring, nontransgenic (KJ1-26– CD4+) cells which would recognize self-Ag and undergo spontaneous activation. However, the activation of Tgfb1−/− DO11.10 T cells was observed even in animals that did not have any detectable inflammatory lesions, suggesting that bystander activation is less likely to be the reason for the activation of these T cells. Another possible explanation is that hybrid TCR (transgenic TCRβ and endogenous TCRα) are present which can recognize self-Ag.
Presence of Hybrid TCR in Tgfb1−/− DO11.10 T Cells
Activation of transgenic T cells in the absence of a cognate antigen (Figure 3b) suggests a possibility that these cells may harbor a hybrid TCR which could recognize self-Ag and undergo activation. This is possible because of endogenous TCRα chain productive rearrangement in a RAG-sufficient background such that the rearranged TCRα can then dimerize with the transgenic TCRβ chain. Indeed, the TCRvα2 chain that is known to be found on a small fraction of DO11.10 T cells20 is expressed on DO11.10 CD4+ T cells and is downregulated on Tgfb1−/− CD4+ T cells (Figure 5a, ∼2-fold decrease in MFI). Downregulation of TCRvα2 in Tgfb1−/− T cells was also observed on KJ1-26+ T cells (hybrid TCR-expressing T cells; upper right quadrants in Figure 5b) albeit to a lesser extent. This suggests that Tgfb1−/− DO11.10 T cells might utilize hybrid TCR to recognize self-Ag and undergo activation. Comparing activation markers and adhesion molecules on DO11.10-positive and -negative T cells within the same splenic population revealed that cells that can recognize self-Ag (DO11.10-negative; right panels in Figure 5c) have higher levels of CD11a, CD44, CD49d and CD69 than do the DO11.10-positive T cells (left panels in Figure 5c) that may not recognize self-Ag. Upregulation of these surface markers is further enhanced by the deficiency of TGFβ1 suggesting increased self-Ag recognition in the absence of TGFβ1 (Figure 5c, open histograms). Analysis of MHC expression on splenocytes revealed that MHC I (H-2Dd) expression is upregulated albeit to a lesser extent on total splenocytes in Tgfb1−/− DO11.10 mice compared to that of control mouse splenocytes. This upregulation is relatively more on KJ1-26+ CD4+ T cells than on other splenocytes. However, MHC II expression is not altered on Tgfb1−/− DO11.10 splenocytes (data not shown). These data demonstrate the presence of hybrid TCR in Tgfb1−/− DO11.10 T cells allowing them to recognize self-Ag and undergo activation.
Discussion
We and others have reported that Tgfb1−/− mice develop multiorgan inflammation, which is caused at least in part by in vivo T-cell activation.1, 2, 7 The mechanisms of T-cell activation and inflammation remain unclear. In this article we asked whether a TGFβ1 deficiency leads to enhanced self-Ag recognition by T cells, thus causing their inappropriate activation and T-cell-mediated inflammation. To address this question we generated Tgfb1−/− DO11.10 mice that carry primarily transgenic T cells as well as some endogenous T cells, and Tgfb1−/− DO11.10 Rag1−/− mice that carry only transgenic T cells. As the antigenic ligand for these T cells is not present in these mice, we did not expect to see spontaneous T-cell activation. Furthermore, we expected these mice to have less inflammation and survive longer, thus permitting future studies on the effect of TGFβ1 deficiency on T-cell activation in the absence of inflammation.
Reducing Endogenous T Cells Reduces Inflammation in Tgfb1−/− Mice, Whereas Eliminating Endogenous T Cells Completely Rescues Them from Autoimmune Inflammation.
In this paper we demonstrate that Tgfb1−/− DO11.10 mice live longer and develop a much milder inflammation in fewer organs than occurs in Tgfb1−/− nontransgenic animals. The reduced inflammation in Tgfb1−/− DO11.10 mice does not likely result from reduced T-cell numbers as the elimination of either CD4+ or CD8+ T cells neither lessens the severity of inflammation nor increases survival of Tgfb1−/− mice.3 As Tgfb1−/− DO11.10 mice still have some endogenous T cells, we generated Tgfb1−/− DO11.10 Rag1−/− mice to eliminate all nontransgenic T cells. These mice live even longer (mean of 8 vs 3 weeks) and do not exhibit significant inflammation in the organs that are usually affected by autoimmunity in Tgfb1−/− mice. Thus, endogenous (self-reactive) T cells play a critical role in the development of multiorgan inflammation in Tgfb1−/− mice.
TGFβ1 Deficiency does not Broadly Impair Thymic Development
In Tgfb1−/− mice that are less than a week old and have no significant inflammation,8 thymocyte development is nearly normal. The thymus becomes smaller, however, as these animals begin to develop inflammatory lesions. At that stage we find cortical depletion, depletion of double-positive thymocytes and an increase in the CD4+ population. This suggested to us that the cortical depletion observed in Tgfb1−/− mice is probably secondary to inflammation, rather than owing to a direct effect of TGFβ1 on thymocytes in the cortex. Improved survival and delayed inflammation in Tgfb1−/− DO11.10 mice allowed us to examine this issue further. Histological and flow cytometry analyses of thymus suggested that there was neither cortical depletion nor a shift in thymocyte profiles before the onset of wasting in Tgfb1−/− DO11.10 mice. Normal thymocyte profiles are seen even after 2 months of age in Tgfb1−/− DO11.10 mice. It is noteworthy that thymocyte development is similar to littermate controls in Tgfb1−/− DO11.10 Rag1−/− mice. Thus, we propose that it is the inflammation and not the lack of TGFβ1 that causes the thymic cortical depletion in Tgfb1−/− mice and that TGFβ1 probably does not play a direct role in thymic development.
Elimination of Endogenous TCR in Tgfb1−/− Mice Prevents Activation of Transgenic T Cells
As is the case for Tgfb1−/− T cells in nontransgenic mice,7 Tgfb1−/− DO11.10 CD4+ T cells exhibit a split anergic phenotype as demonstrated by increased IFN-γ production and TCR downmodulation, and reduced proliferation and IL-2 production in response to ex vivo receptor-mediated mitogenic stimulation. These data suggest that Tgfb1−/− DO11.10 T cells become activated in vivo in response to self-Ag presentation and display a split anergic phenotype when stimulated ex vivo with Con A or anti-CD3.
Interestingly, activation of DO11.10 transgenic T cells occurs in Tgfb1−/− mice without any cognate peptide-Ag in vivo. This phenomenon could be due either to the presence of bystander nontransgenic T cells that recognize self-Ag and undergo activation and activate KJ1-26+ T cells, to the presence of hybrid TCR which can recognize self-Ag, or to both. Indeed, some transgenic (KJ1-26+ CD4+) T cells also express endogenous TCRvα2, suggesting that hybrid TCR expression on KJ1-26+ T cells could be primarily responsible for their activation through the recognition of self-Ag. To test this further, we generated Tgfb1−/− DO11.10 Rag1−/− mice that have no nontransgenic T cells and no hybrid TCR-bearing transgenic T cells. In these mice, splenic T cells do not exhibit any evidence of activation. These data clearly indicate that Tgfb1−/− T cells undergo activation due to their reactivity towards self-Ag, and that elimination of self-reactive TCR-bearing T cells eliminates T-cell activation and inflammation in Tgfb1−/− mice.
Recent studies have suggested that TGFβ1 is required for peripheral maintenance of Treg cells, as the percentage of CD4+CD25+ T cells are decreased in the spleens of Tgfb1−/− mice.21, 22 To our surprise there was an increase in percentage of CD4+CD25+ T cells in the spleens of Tgfb1−/− DO11.10 mice compared to that of littermate control DO11.10 mice (Figure 3b). Consistent with that of others we also have seen a decrease in percentage of CD4+CD25+ T cells in 2-week-old Tgfb1−/− mice. This difference between Tgfb1−/− and Tgfb1−/− DO11.10 mice could be due to their difference in the TCR repertoire. The increased percentage of CD4+CD25+ in Tgfb1−/− DO11.10 mice is mainly due to an increase in the TCR-transgenic (KJ1-26+) CD4+CD25+ T cells. However, there was no detectable number of CD4+CD25+ T cells in the spleens of DO11.10 Rag1−/− mice whether they expressed Tgfb1 or not. This suggests that CD4+CD25+ Treg-cell generation is self-Ag dependent and TGFβ1 might modulate their generation indirectly. These findings are discussed further in a separate report (manuscript submitted).
Non-T-Cell Effects of TGFβ1 Deficiency
Despite a relatively modest systemic inflammation in Tgfb1−/− DO11.10 mice, these mice still exhibit a wasting syndrome similar to that of lymphocyte-deficient Rag1−/− TCR nontransgenic Tgfb1−/− mice, suggesting that TGFβ1 may have additional roles that contribute to the thriving of these mice. The wasting syndrome is independent of lymphocyte activation because Tgfb1−/− Rag2−/− and Tgfb1−/− Rag1−/− and Tgfb1−/− SCID-deficient mice can also die from wasting (Figure 1b, also see Bommireddy et al3). Tgfb1−/− mice usually die within 3–4 weeks after birth, and this depends on the genetic background. Tgfb1−/− mice on a BALB/c background develop disease earlier and die earlier than when on other backgrounds. Tgfb1−/− mice on SCID (primarily C3H) or RAG KO (primarily 129) backgrounds live longer, but eventually die (2–6 months) of either wasting (both backgrounds) or colon cancer (primarily 129 background only).
In summary, naïve T cells interact with self-MHC for long-term survival in the periphery. The signal strength generated during such interactions needs to be maintained at such a level that the T cells do not undergo inappropriate activation. TGFβ1 plays a critical role in regulating the threshold level of activation to induce tolerance instead of activation, thus maintaining immune homeostasis and preventing autoimmunity. Our data indicate that Tgfb1−/− T cells become activated through self-Ag recognition thus causing autoimmune inflammation.
References
Shull MM, Ormsby I, Kier AB, et al. Targeted disruption of the mouse transforming growth factor-beta 1 gene results in multifocal inflammatory disease. Nature 1992;359:693–699.
Kulkarni AB, Huh CG, Becker D, et al. Transforming growth factor beta 1 null mutation in mice causes excessive inflammatory response and early death. Proc Natl Acad Sci USA 1993;90:770–774.
Bommireddy R, Engle SJ, Ormsby I, et al. Elimination of both CD4(+) and CD8(+) T cells but not B cells eliminates inflammation and prolongs the survival of TGFbeta1-deficient mice. Cell Immunol 2004;232:96–104.
Boivin GP, Ormsby I, Jones-Carson J, et al. Germ-free and barrier-raised TGF beta 1-deficient mice have similar inflammatory lesions. Transgenic Res 1997;6:197–202.
Chen CH, Seguin-Devaux C, Burke NA, et al. Transforming growth factor beta blocks Tec kinase phosphorylation, Ca2+ influx, and NFATc translocation causing inhibition of T cell differentiation. J Exp Med 2003;197:1689–1699.
Chen W, Jin W, Tian H, et al. Requirement for transforming growth factor beta1 in controlling T cell apoptosis. J Exp Med 2001;194:439–453.
Bommireddy R, Saxena V, Ormsby I, et al. TGF-beta1 regulates lymphocyte homeostasis by preventing activation and subsequent apoptosis of peripheral lymphocytes. J Immunol 2003;170:4612–4622.
Bommireddy R, Ormsby I, Yin M, et al. TGFbeta1 inhibits Ca2+-calcineurin-mediated activation in thymocytes. J Immunol 2003;170:3645–3652.
Chen W, Jin W, Hardegen N, et al. Conversion of peripheral CD4+CD25- naive T cells to CD4+CD25+ regulatory T cells by TGF-beta induction of transcription factor Foxp3. J Exp Med 2003;198:1875–1886.
Fantini MC, Becker C, Monteleone G, et al. Cutting edge: TGF-beta induces a regulatory phenotype in CD4+CD25- T cells through Foxp3 induction and down-regulation of Smad7. J Immunol 2004;172:5149–5153.
Zhu Y, Richardson JA, Parada LF, et al. Smad3 mutant mice develop metastatic colorectal cancer. Cell 1998;94:703–714.
Datto MB, Frederick JP, Pan L, et al. Targeted disruption of Smad3 reveals an essential role in transforming growth factor beta-mediated signal transduction. Mol Cell Biol 1999;19:2495–2504.
Yang X, Letterio JJ, Lechleider RJ, et al. Targeted disruption of SMAD3 results in impaired mucosal immunity and diminished T cell responsiveness to TGF-beta. EMBO J 1999;18:1280–1291.
Engle SJ, Hoying JB, Boivin GP, et al. Transforming growth factor beta1 suppresses nonmetastatic colon cancer at an early stage of tumorigenesis. Cancer Res 1999;59:3379–3386.
Engle SJ, Ormsby I, Pawlowski S, et al. Elimination of colon cancer in germ-free transforming growth factor beta 1-deficient mice. Cancer Res 2002;62:6362–6366.
Takahashi T, Tagami T, Yamazaki S, et al. Immunologic self-tolerance maintained by CD25(+)CD4(+) regulatory T cells constitutively expressing cytotoxic T lymphocyte-associated antigen 4. J Exp Med 2000;192:303–310.
Schultz JJ, Witt SA, Glascock BJ, et al. TGF-beta1 mediates the hypertrophic cardiomyocyte growth induced by angiotensin II. J Clin Invest 2002;109:787–796.
Lin JT, Kitzmiller TJ, Cates JM, et al. MHC-independent genetic regulation of liver damage in a mouse model of autoimmune hepatocellular injury. Lab Invest 2005;85:550–561.
Boivin GP, O'Toole BA, Orsmby IE, et al. Onset and progression of pathological lesions in transforming growth factor-beta 1-deficient mice. Am J Pathol 1995;146:276–288.
Zhou P, Borojevic R, Streutker C, et al. Expression of dual TCR on DO11.10 T cells allows for ovalbumin-induced oral tolerance to prevent T cell-mediated colitis directed against unrelated enteric bacterial antigens. J Immunol 2004;172:1515–1523.
Marie JC, Letterio JJ, Gavin M, et al. TGF-{beta}1 maintains suppressor function and Foxp3 expression in CD4+CD25+ regulatory T cells. J Exp Med 2005;201:1061–1067.
Mamura M, Lee W, Sullivan TJ, et al. CD28 disruption exacerbates inflammation in Tgf-beta1−/− mice: in vivo suppression by CD4+CD25+ regulatory T cells independent of autocrine TGF-beta1. Blood 2004;103:4594–4601.
Acknowledgements
We thank Dr David A Hildeman (Cincinnati Children's Hospital) for critical comments. We also thank James Cornelius and Sandy Schwemberger for expert assistance in flow cytometry and Mark Kader for assistance with genotyping and cell preparation. We also thank Mouhamadou Niang for help in PCR genotyping. This study was supported by NIH HD26471, ES06096 and CA84291 to TD, AR50797, AR47322 and DK69282 to RRS, and by a grant from Shriners of North America to GFB.
Author information
Authors and Affiliations
Corresponding author
Additional information
Duality of interest
The authors declare that they do not have any duality of interest.
Rights and permissions
About this article
Cite this article
Bommireddy, R., Pathak, L., Martin, J. et al. Self-antigen recognition by TGFβ1-deficient T cells causes their activation and systemic inflammation. Lab Invest 86, 1008–1019 (2006). https://doi.org/10.1038/labinvest.3700460
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/labinvest.3700460
Keywords
This article is cited by
-
The roles of TGFβ in the tumour microenvironment
Nature Reviews Cancer (2013)
-
The mRNA level of the transforming growth factor β1 gene, but not the amount of the gene product, can be considered as a potential prognostic parameter in inflammatory bowel diseases in children
International Journal of Colorectal Disease (2013)
-
TGF-β puts the brakes on homeostatic proliferation
Nature Immunology (2012)